Emerging Concepts and Technologies in Transcatheter Aortic Valve Replacement
Clinical Summary
- New TAVR systems demonstrated excellent safety and durability across aortic stenosis and aortic regurgitation populations, with low adverse event rates and improved quality of life.
- The novel device designs overall had high procedural success rates and improved hemodynamics.
- Personalized assessment tools and next-generation materials are reshaping the quantification, timing, and durability of transcatheter valve therapy.
Introduction
At the Transcatheter Cardiovascular Therapeutics (TCT) 2025 Conference in San Francisco, California, international investigators unveiled pivotal data on emerging transcatheter aortic valve replacement (TAVR) systems and analytic innovations. Presentations highlighted new research—including trials of the DurAVR Transcather Heart Valve (THV) (Anteris Technologies), Hanchor Valve (Healing Medical), J-Valve (JC Medical), Ken-Valve (Jenscare Scientific), Siegel THV (MiRus), and TaurusNXT System (Peijia Medical), as well as the Aortic Valve Area Reduction study—demonstrating advances in safety, valve performance, and patient outcomes across diverse anatomical and clinical subsets.
Session Highlights
DurAVR
Dr Rishi Puri of the Cleveland Clinic reported 1-year results for the DurAVR THV, which mimics native leaflet motion using ADAPT anti-calcification and anti-fibrotic tissue. Across various anatomies, the DuraAVR demonstrated technical and device success of 94% and 92%, respectively, and no occurrences of moderate or severe paravalvular leak or prosthesis-patient mismatch (PPM) at 1 year. In patients with small aortic annuli, researchers reported no valve-related mortality and a mean gradient drop from 46 to 8.6 mm Hg at 1 year; these patients also experienced a PPM rate of only 1.5% at 30 days, outperforming both balloon- and self-expanding valves.
Hanchor
On behalf of the HAVE AR investigators, Dr Wenzhi Pan of Fudan University shared results of the multicenter HAVE AR trial, which investigated early outcomes of the Hanchor Valve for treating patients with pure native aortic regurgitation (AR). In 128 high-risk patients implanted with the valve, the study reported 96.1% procedural success and a low frequency of adverse safety events. Left ventricular (LV) function and quality of life (QoL) improved significantly, and valve dysfunction occurred in less than 2% of cases at 1 year, affirming the Hanchor system’s suitability for this population.
J-Valve
Dr Santiago Garcia presented 6-month data on the novel J-Valve THV from the Transfemoral Early Feasibility Study, which looked at outcomes in high-risk patients with symptomatic AR (≥3+). Aimed at this specific population, the J-Valve’s design incorporates unique rounded, atraumatic anchor rings for optimal alignment and position; it also comes in 5 sizes to accommodate perimeters from 57 to 104 mm, expanding access to more patients. Among 25 patients, 92% achieved successful implantation with more than 90% experiencing no or trace regurgitation, and no cardiovascular deaths were reported. LV mass and volumes decreased significantly, and improvement in QoL was noted.
Ken-Valve
Dr Anson Cheung of St. Paul’s Hospital, Vancouver, reported 1-year outcomes from 142 patients treated with the Ken-Valve, a TAVR device intended for AR featuring an innovative design that includes a soft polytetrafluoroethylene skirt to prevent PVL and enhanced radial force to counteract migration. Data showed 97.2% device success and, at 1 year, 94.7% mild-or-less AR or PVL. Based on these results as well as significant NYHA and QoL gains, the clinical trial team concluded that the valve is a promising option for treating patients with severe and mixed AR.
Siegel
Dr Pradeep Yadav presented early feasibility study results on the balloon-expandable Siegel THV for treating patients with symptomatic severe aortic stenosis (AS); this US-based study included 30 patients from up to 10 centers. The design of the Siegel is notable for being nickel-free, and its delivery system involves no foreshortening, allowing for higher, more precise placement. Thirty-day results showed an achievement of zero 30-day mortality or stroke, with the only noted clinical outcome being a 5.7% new pacemaker rate. Hemodynamics improved markedly, demonstrating superior results to the comparable market leader.
TaurusNXT
Dr Wenzhi Pan returned to discuss the 2-year results from the NXT-DURA trial, which included 150 patients with severe AS—approximately half of whom had bicuspid valves—treated with the TaurusNXT valve. The TaurusNXT incorporates several significant technological updates: non-aldehyde “dry-valve” leaflet processing; enhanced frame and skirt design, including optimized frame geometry and radiopaque markers improve commissural alignment; and a 3-dimensional steerable delivery system. Dr Pan emphasized that this design supports a “lifetime management” concept for self-expanding valves, accounting for future coronary reaccess and procedural reproducibility. Data confirmed that clinical needs were met, including success rates of >93% and PVL ≤1.4% at 2 years.
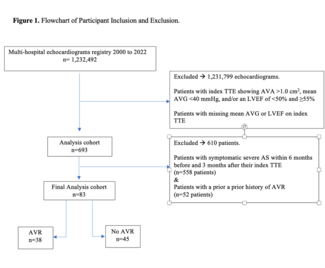
Personalized AS Quantification
Dr Miho Fukui and colleagues introduced a new method to assess AS severity via a personalized percent aortic valve area (%AVA) reduction rather than the traditional fixed cutoff of less than 1 cm2. Using a newly developed formula that estimates normal AVA from the annulus area, their analysis of over 1200 TAVR patients showed that greater %AVA reduction correlated with more advanced cardiac damage—suggesting earlier intervention may improve outcomes.
Conclusion
This session underscored the rapid evolution of TAVR technology—offering safer, more durable, and patient-tailored solutions across the spectrum of valvular disease. Upcoming data, including ongoing long-term follow-up from the NXT-Dura trial, a pivotal randomized control trial of the Siegel valve, and the recently approved global pivotal PARADIGM Trial (DurAVR), are expected to further validate these next-generation devices’ role in reshaping aortic valve care.
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.