Septal Coronary Artery Fistula After Implantation of a Left Bundle Branch Area Pacemaker
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2026. doi:10.25270/jic/26.00017. Epub January 28, 2026.
A 51-year-old man with a mixed-phenotype cardiomyopathy was referred for coronary angiography because of new-onset episodes of ventricular arrythmias. At his initial presentation in 2014, he was diagnosed with hypertrophic cardiomyopathy, presumably related to poorly controlled arterial hypertension. Since 2024, progressive dilatation of the left ventricle accompanied by the development of heart failure with reduced ejection fraction (HFrEF) with an EF of 22% had been observed.
Because of intermittent total atrioventricular block and severely reduced EF, cardiac resynchronization therapy with a defibrillator (CRT-D) in primary prevention was implemented. The left ventricular pacing lead was positioned in the left bundle branch area position (LBBAP). A single screw-in attempt at a depth of 16 mm within the hypertrophic septum was sufficient to achieve conduction system pacing.
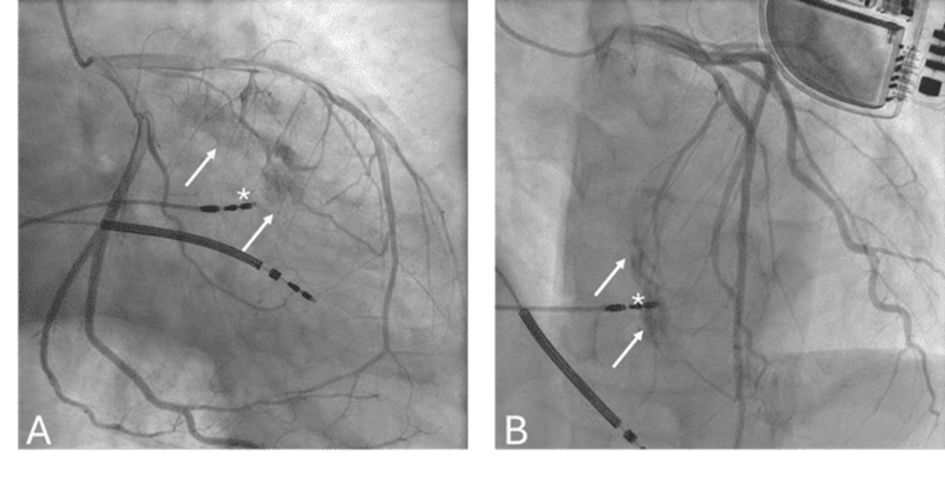
Coronary angiography (Figure) demonstrated contrast extravasation (Videos 1 and 2) from a large septal branch of the left anterior descending coronary artery toward the right ventricle. Given the small shunt and the asymptomatic presentation, a conservative management strategy was adopted.
Septal coronary artery fistulization after LBBAP implantation is considered a rare complication; the exact prevalence is unknown. Therefore, because most reported cases are in asymptomatic patients who do not require intervention, underdiagnosis is likely.1,2 The diagnosis can be established using echocardiography demonstrating a color Doppler jet1,3 or by coronary angiography.1,2 In our case, the ultrasound was negative for a septal color. As LBBAP becomes more widely implemented in clinical practice, the incidence of reported complications is expected to increase.
Affiliations and Disclosures
Nicolas Bradt, MD; Maxim Verlee, MD, PhD(c); Christophe Borin, MD; Hans Vandekerckhove, MD; Laurens De Vos, MD
From AZ Sint-Lucas Ghent, Ghent, Belgium.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication of their data/thereof, including any and all images.
Address for correspondence: Nicolas Bradt, MD, AZ Sint-Lucas Ghent, Groenebriel 1, 9000 Gent, Belgium. Email: nicolas.bradt@ugent.be
References
1. Kato H, Yanagisawa S, Ota R, et al. Septal coronary artery fistula after left bundle branch area pacing assessed by multi-imaging modalities and shunt volume quantification. Pacing Clin Electrophysiol. 2022;45(11):1299-1302. doi:10.1111/pace.14548
2. Ferrari ADL, Klafke LH, Soccol R, et al. Coronary artery complications after left bundle branch area pacing: an increasingly reported issue in the era of physiologic pacing. Pacing Clin Electrophysiol. 2024;47(1):101-105. doi:10.1111/pace.14710
3. De Pooter J, Calle S, Demulier L, Timmermans F, Van Heuverswyn F. Septal coronary artery fistula following left bundle branch area pacing. JACC Clin Electrophysiol. 2020;6(10):1337-1338. doi:10.1016/j.jacep.2020.08.038





















