Editor’s 2025 Top 10: Outcomes With Distal Transradial Access in Patients With Advanced Chronic Kidney Disease
Dr Deepak L. Bhatt, editor-in-chief of the Journal of Invasive Cardiology, catches up with Dr Sripal Bangalore about his Editor’s 2025 Top 10 article, “Outcomes With Distal Transradial Access in Patients With Advanced Chronic Kidney Disease.”
Transcript:
Dr Bhatt: Hello, I'm Dr. Deepak Bhatt, the Editor-in-Chief of the Journal of Invasive Cardiology and also the Director of the Mount Sinai Fuster Heart Hospital in New York City. Really a pleasure to be here today with Dr Sripal Bangalore from NYU. I've known him for many years, a former superstar fellow, and just an incredible career trajectory.
I was going to chat with him today about a nice paper on which he was a senior author out of the NYU cath lab talking about distal transradial access in patients with advanced chronic kidney disease (CKD). Sometimes, operators are worried about patients with CKD and radial access in general, thinking, “what if the patient needs dialysis? Am I going to mess up a future vascular conduit?” And for that reason, there's some degree of debate about whether to go radial or not. In this study, the authors actually used distal transradial access. So, Sripal, first of all, welcome, great to be able to chat with you.
Dr Bangalore: Thank you, thanks for having me on, and great seeing you, Deepak.
Dr Bhatt: I was really wanting you to share with the audience, first of all, your experience with distal transradial access. Radial access now is catching on in the United States. The latest numbers show the majority of patients in the United States are now finally getting a cath via the radial approach. Distal transradial is still pretty uncommon overall. What are your thoughts about its incremental value?
Dr Bangalore: Great question. So, you know, I've been one of the radial-first operators for a long time, having trained with you and a lot of other people. I started doing distal transradial, I would say, almost a decade ago. This question came up because, interestingly enough, I was part of the 2021 REVASC guidelines, and we know now that even the guideline recommendation is for transradial access, both for acute coronary syndromes and for stable ischemic heart disease. Interestingly, if you look at the kidney guidelines, the KDIGO guidelines, if you have a patient with CKD, they would say to maybe avoid radial access in these patients because they may need it for future distal access. I was part of some of the iterations of the KDIGO, and because of this, a decade ago, I was like, okay, I'm seeing a lot of these patients who for preop evaluation will just go distal. That is the background for this publication.
Dr Bhatt: Terrific. Can you share with the audience what you found in your study?
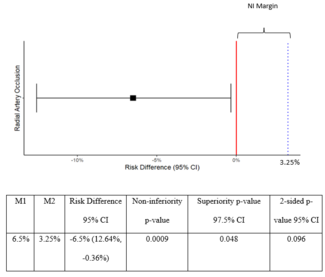
Dr Bangalore: What we did was we took patients with advanced CKD, so anybody with CKD stage 3 or greater, including patients on dialysis. We had 71 patients who had distal transradial access and also at least 30 days of follow-up, and 66% of the patients were on hemodialysis. This was a single-arm retrospective analysis, so it's not randomized.
Our primary endpoint was radial artery occlusion. In terms of access, we used either right radial or left radial, but it was distal. The way we did this procedure was ultrasound-guided, sticking in the anatomic snuff box. In the initial part, we were using a 5F sheath; later on, we have a 6F, 7 centimeters, so it's a short sheath so that you don't damage the more proximal part of those radial arteries. Also, it will stay in the distal part of the radial artery and several centimeters into it. And of course, we took all of the precautions, vasospastic agents, and giving heparin if it is diagnostic only, and patent hemostasis, all of those.
Our primary endpoint was radial artery occlusion, and we measured that using either a reverse Barbeau test or, if the patient came back for a second procedure, whether we were able to re-access the same site. We had 71 patients, 66% were on hemodialysis, and our radial artery occlusion rate was 0%, so none of the patient had radial artery occlusion. I just want to clarify that the radial artery occlusion we were looking at was proximal radial artery occlusion; it's not at the site of the distal radial artery access, but we were looking at proximal radial. The reason we looked at the proximal radial artery is because that's the place we want to spare these patients, so they can have future arteriovenous (AV) fistula access there.
Dr. Bhatt: It's a great study. In fact, it made the JIC Top 10 Articles for 2025, so congratulations on that.
I'm actually a big believer in distal radial access. This was after you left, but at Brigham and Women's, I actually did the first one there. It was a patient who had really, really bad peripheral arterial disease, so lower extremity access wasn't going to be possible at all in that case. I was just planning to do radial, but it turned out he had bilateral hemarthrosis, so his elbows were rotated inward like this and couldn’t be flexed or supinated or anything. So the only access, really, that was feasible would have been distal or transradial. It worked out well, so that was the first time. Actually, at Mount Sinai, I did the first distal radial access for that institution too.
I think it's really useful in situations where someone, like I mentioned, for whatever reason, can't turn over their wrist. But there may be value beyond that, as you're pointing out, and there are a number of series we've actually published in JIC showing pretty good results with experienced operators. I think key things are ultrasound—personally, I think ultrasound should be used for all vascular access, but certainly for distal radial access I think it's an especially good idea. We published an image on this in JIC some years ago.
You have to be a little bit cautious as well, because in terms of potential complications, you can get bleeding from a radial, but usually not a big deal. Femoral is a big deal. Radial, usually not a big deal when people bleed, just apply some pressure. Rare to get a forearm compartment syndrome; it can happen, but it's extremely rare. On the other hand, with distal radial, you can get a compartment syndrome, but it won't be of the forearm, it would be of the hand. That's an extremely rare occurrence, obviously, but at least operators should be aware of that possibility. So, if someone's saying, “my hand's swollen, it hurts,” they shouldn't just assume it's a little bit of access site bleeding, nothing to worry about. They need to, at least in the back of their mind think, and make sure that there's no neurological or other compromise that might support a compartment syndrome.
But other than that caveat, and the need for some degree of technical proficiency and ultrasound proficiency, it seems like a great technique in general, especially in the circumstance that you're talking about, where the radial artery might be used for a dialysis conduit.
Dr Bangalore: Absolutely. And to weigh in on that, I remember my very first distal radial, we did this distal radial, it ended up to be a left main bifurcation. So, it just goes to show, my very first case, we were doing distal left main bifurcation stenting through distal radial. And of course, once you get access, once you're up there, you don't even notice the difference between a regular radial and distal.
Your point about hematoma is very well taken. One of the things that I always tell my fellows is, if you remember the first distal radial, one of the things that went viral on Twitter was hemostasis with the tip of a finger. The case was done, and they take out the sheath and tip of the finger, and it's done. Because it's distal, it's small, especially if it’s diagnostic only, it's just a couple of minutes of compression, and it is fine. One of the big challenges is if you use a TR band; it doesn't sit well there, it tends to slip away, etc. So now we have dedicated bands. Even in this study, we used what is called a [SafeGuard (Merit Medical)]; it has a foot plate, which actually sits in that anatomic snuff box, makes hemostasis much better, and it doesn't slip away. Our strategy has always been to do ultrasound-guided compression and use the SafeGuard, which has a nice, small footprint that sits in that anatomic snuff box, and the risk of hematoma is extremely, extremely rare.
Dr Bhatt: Oh, so you actually do ultrasound-guided compression first?
Dr Bangalore: Oh, no, ultrasound-guided access. The closure device is called the SafeGuard.
Dr Bhatt: Oh, sure. I was going to say ultrasound-guided compression would be a bit much, unless there was a pseudoaneurysm or something. Bu that sounds like a really great approach. You know, this will get posted out there in social media. Maybe when you see that, you can just sort of reply to it with this specific closure, or whatever technique you think is best in terms of hemostasis, because I think you're right—standard sorts of approaches for radial access, hemostasis, those types of bands don't really fit so well with distal radial access. You can jerry-rig them, you can sort of fold 4 x 4 gauzes and stick them underneath and kind of mimic them, but even if one's doing it infrequently, it’s probably good to have the dedicated devices.
Before we close, any final words of wisdom for the audience about distal radial access in general, or specifically in CKD patients?
Dr Bangalore: Specifically in CKD, as a cardiologist what we need to understand is that the AV fistula for these patients does not last forever; these patients go through AV fistula pretty frequently in their lifetime. Many of these patients are going to do 2 or 3 or even more. That's the main reason why we want to preserve as much of their access point as possible. As a cardiologist speaking to a cardiologist, I would say that AV fistula is the lifeline for these patients. So whatever we can do to preserve their future access will be much appreciated by the nephrology community.
Dr Bhatt: Do you happen to know, though, is it really such a big deal doing radial access in CKD patients, putting the KDIGO guidance aside? That is, some folks will lose a distal radial pulse, but it doesn't really cause a problem for the hand. Is it any worse than creating the AV fistula in that setting than it would otherwise be? Do you happen to know?
Dr Bangalore: That's a great question. So, we know from data that the incidence of asymptomatic radial artery occlusion is 1% to 10%, and that's higher if you have CKD. Interestingly, we don't know the actual rates in dialysis patients; it's likely even higher. What has happened in that field is there are percutaneous ways of doing AV fistula these days, so they can actually go through the radial artery and create a forearm AV fistula. So, if that radial artery is occluded there, that precludes them from doing it; that's the main reason that preserving the patency of the radial artery is very important. Of course, there are histopathological studies looking at all these histological changes, dissections, all of those things at the site of puncture when you do transradial access, which is a topic for different discussion. Even if the patient is undergoing CABG, there is some concern that maybe we can't use that as a graft conduit.
Dr Bhatt: Sure. Well, really great points, and once again, congratulations to you and your colleagues on this excellent paper, and to you on all your contributions to the field.
Dr Bangalore: Thank you very much, and thanks for publishing this in JIC.
The transcript has been lightly edited for clarity.
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.