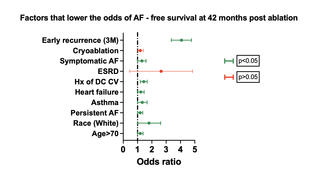
Right Internal Jugular Pulsed Field Ablation for Atrial Fibrillation in a Patient With an Inferior Vena Cava Filter
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2026. doi:10.25270/jic/26.00023. Epub January 29, 2026.
A 77-year-old man with peripheral arterial disease, sick sinus syndrome, hypertension, and paroxysmal atrial fibrillation (AF) presented for rhythm control. He had a normally functioning dual-chamber pacemaker but had frequent symptomatic AF episodes and elected catheter ablation.
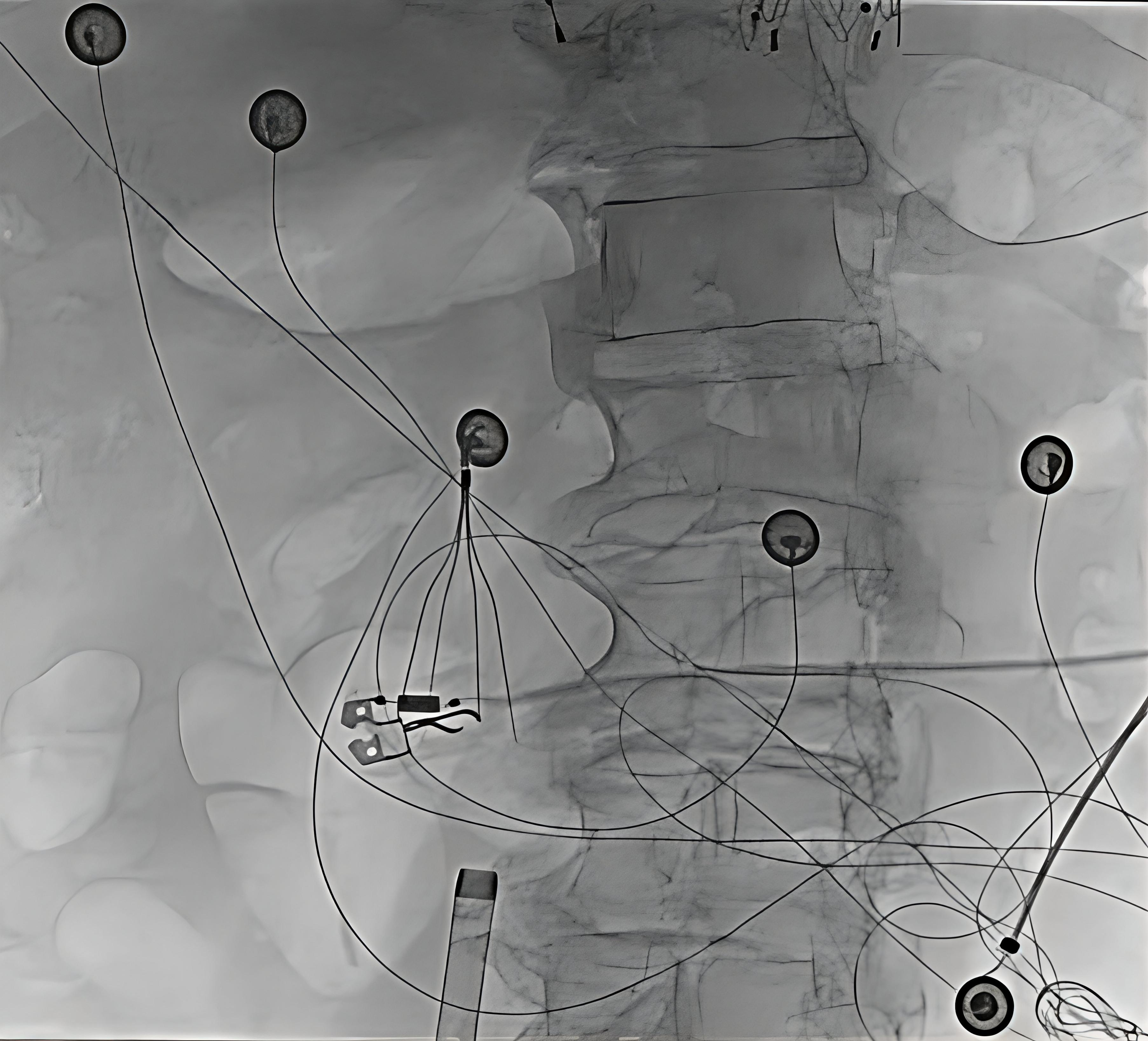
An initial femoral approach was aborted when an inferior vena cava (IVC) filter was encountered. Attempts to pass wires and sheaths through the filter resulted in appreciable filter movement under fluoroscopy, raising concern for dislodgment or vascular injury. The procedure was terminated without complication, and ablation was rescheduled using an alternative access strategy (Figure 1, Video).
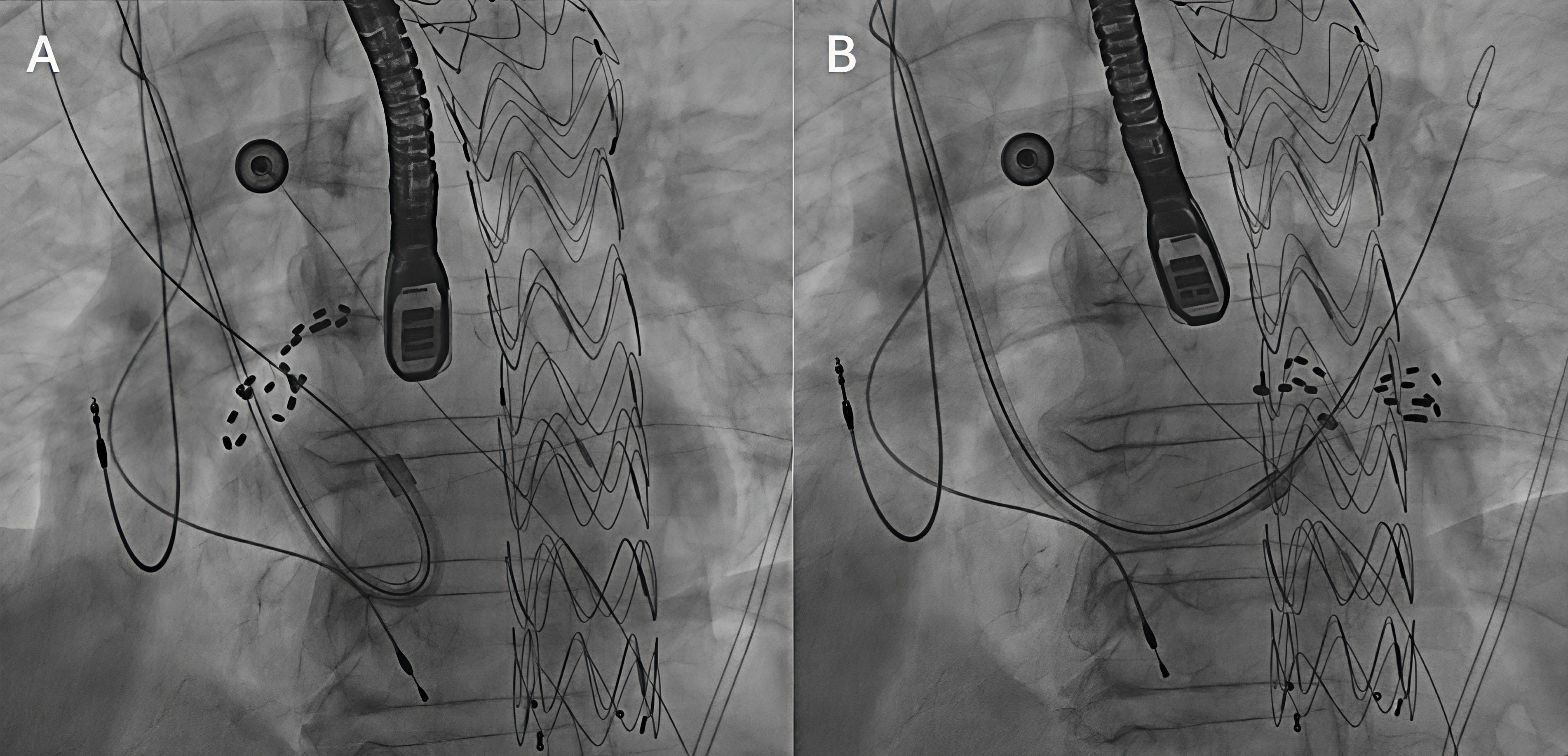
Pulmonary vein isolation was subsequently performed using pulsed field ablation (PFA) via the right internal jugular (RIJ) vein. RIJ access was obtained under ultrasound guidance. Transesophageal echocardiography excluded intracardiac thrombus and guided transseptal puncture using an Agilis steerable sheath (Abbott), ProTrack pigtail wire (Baylis), and a Bovie device (Medtronic Covidien). Because the superior route requires approaching the fossa ovalis from above, operators must work through a steeper and less favorable transseptal angle, and catheter manipulation can be more challenging. Awareness of reduced catheter stability, as well as the altered torque response and fluoroscopic orientation inherent to a superior-only approach, was important for navigation of the left atrium. Heparin was administered to maintain an activated clotting time of 300 to 350 seconds. The sheath was then exchanged for the FARAPULSE system (Boston Scientific), and all 4 pulmonary veins were successfully isolated with demonstration of exit block (Figure 2). PFA was selected for its tissue-selective, non-thermal mechanism that reduces collateral injury risk. Post-procedure electrocardiography showed atrial pacing with left axis deviation and left bundle branch block.
As electrophysiology procedures expand, more patients present without safe femoral access. In carefully selected cases, superior venous access can be a viable alternative when femoral access is limited by IVC filters, venous thrombosis, chronic occlusion, prior vascular surgery, or congenital IVC interruption. This report illustrates a novel alternative access strategy for FARAPULSE pulmonary vein isolation that was performed safely and effectively via the right internal jugular vein.
Affiliations and Disclosures
Jeong Hwan J. Kim, MD1; Leili Pourafkari, MD1,2; Jonathan Lalezari, MD1; Ali Sovari, MD1,3
From the 1Department of Cardiovascular Disease, Los Robles Regional Medical Center, Thousand Oaks, California; 2Department of Anesthesiology, Jacobs School of Medicine and Biomedical Sciences, Buffalo, New York; 3Department of Cardiology, St. John’s Regional Medical Center, Oxnard, California.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for intervention described in the manuscript and to the publication of their data including all images. The authors report that patient consent was provided for publication of the images used herein.
Address for correspondence: Ali Sovari, MD, Department of Cardiology, St. John’s Regional Medical Center, 1600 N Rose Ave, Oxnard, CA 93030, USA. Email: alisovari@gmail.com