Ventricular Fibrillation as a Manifestation of Delayed Distal Coronary Perforation Induced by High Blood Pressure
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00384. Epub December 29, 2025.
An 81-year-old man with hypertension presented with worsening exertional angina. Coronary computed tomography angiography showed diffuse calcification and stenosis in the right coronary artery (RCA). He was admitted for elective percutaneous coronary intervention (PCI).
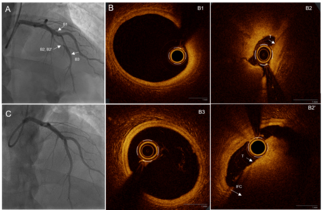
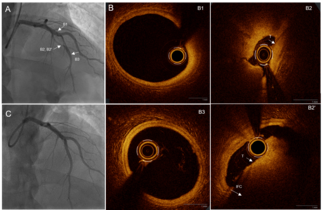
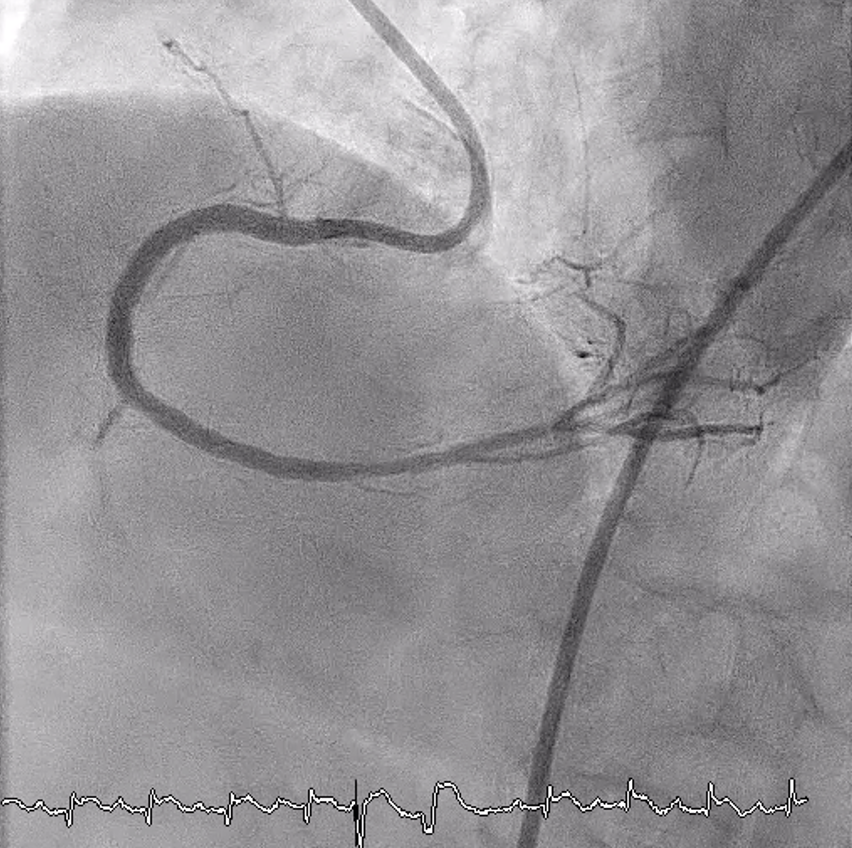
His baseline blood pressure (BP) was 180 to 190/90 to 100 mm Hg. An angiogram confirmed heavy calcification with 80% stenoses in the proximal/mid-RCA and subtotal occlusion distally (Figure 1). PCI was performed via femoral access using a 7F 0.75 Amplatz Left guide catheter (Medtronic). The RCA was successfully wired with a Fielder FC (ASAHI INTECC), supported by a FineCross microcatheter (Terumo). However, neither the microcatheter nor a 1.0 × 10-mm Sapphire balloon (OrbusNeich) could cross the mid-RCA lesion.
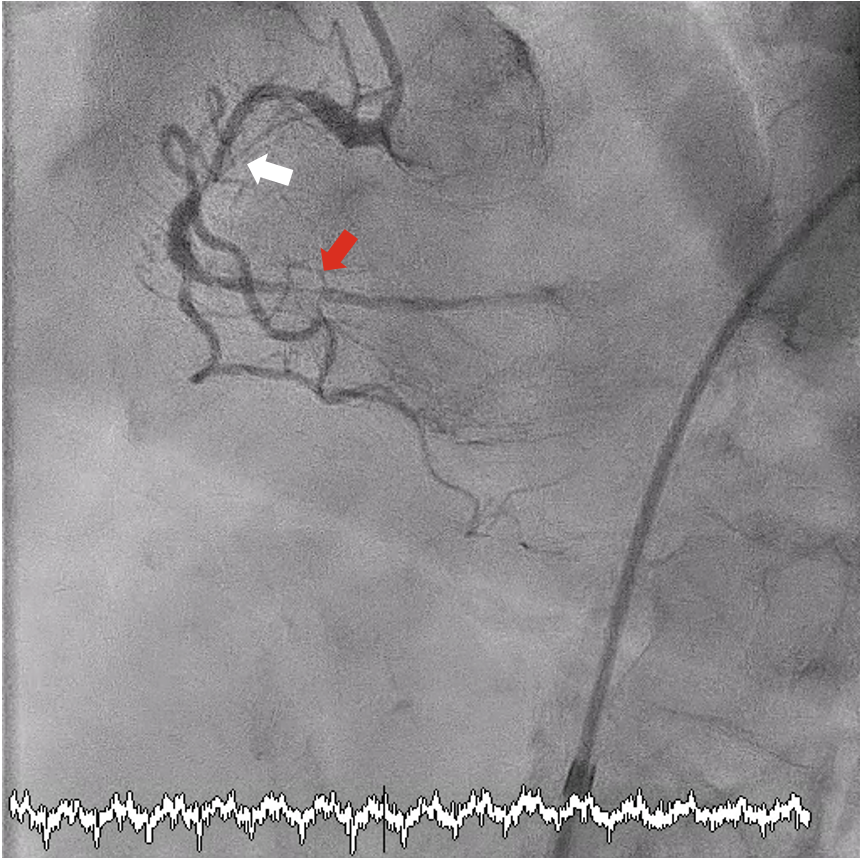
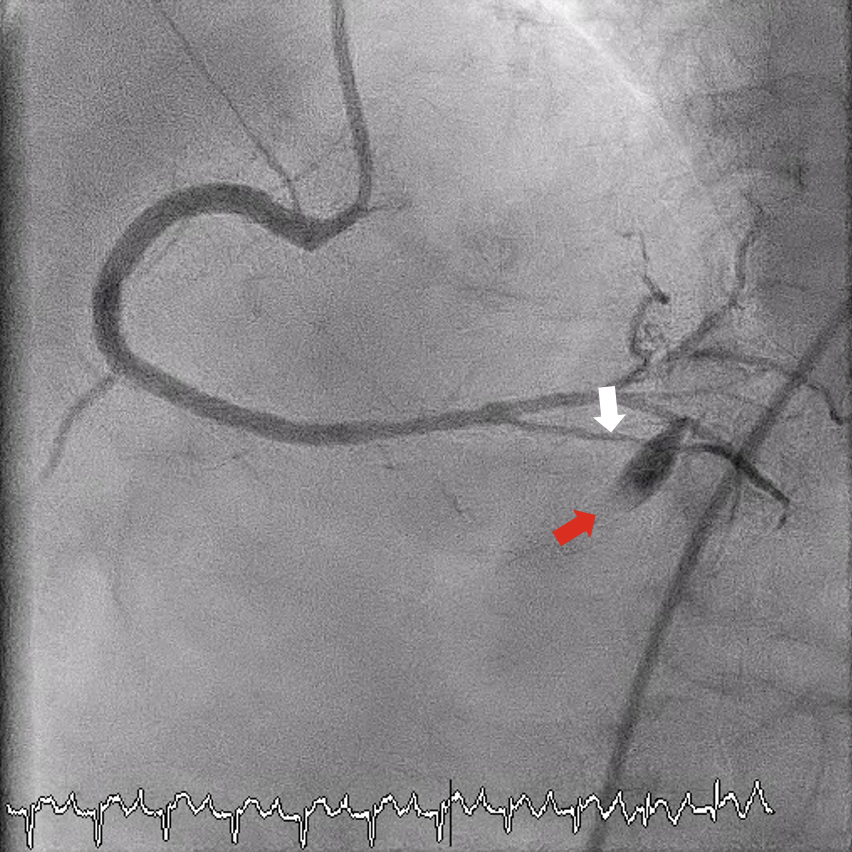
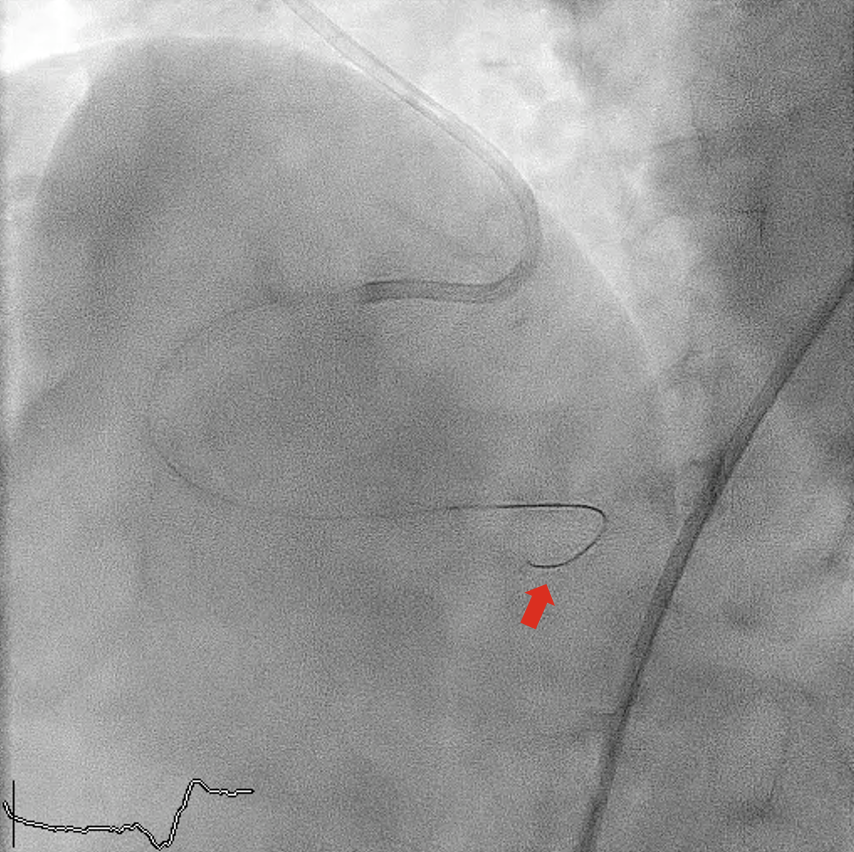
Excimer laser coronary atherectomy (ELCA; 0.9-mm catheter, escalated to 80 mJ/mm²/80 Hz, 25 cycles) (Philips) was used to facilitate crossing. During ELCA, hypotension (85/50 mm Hg) and chest pain occurred, which were attributed to dissection with slow flow (Figure 2, Video 1). Sequential balloon dilatations restored flow and hemodynamics stabilized at approximately 120/80 mm Hg without inotropes. Intravascular ultrasound (IVUS)-guided treatment included a 2.0 × 30-mm SeQuent Please NEO drug-coated balloon (B. Braun) distally and 2 overlapping Coroflex ISAR NEO drug-eluting stents (B. Braun) (2.25 × 38 mm and 3.5 × 32 mm) proximally, with excellent final angiographic (Figure 3, Video 2) and IVUS results.
After arrival in the coronary care unit, the patient’s BP returned to his baseline high BP of approximately 190/90 mm Hg; oral antihypertensive was given. One hour later, the patient suddenly developed ventricular fibrillation, which was successfully defibrillated. Echocardiogram showed no pericardial effusion.
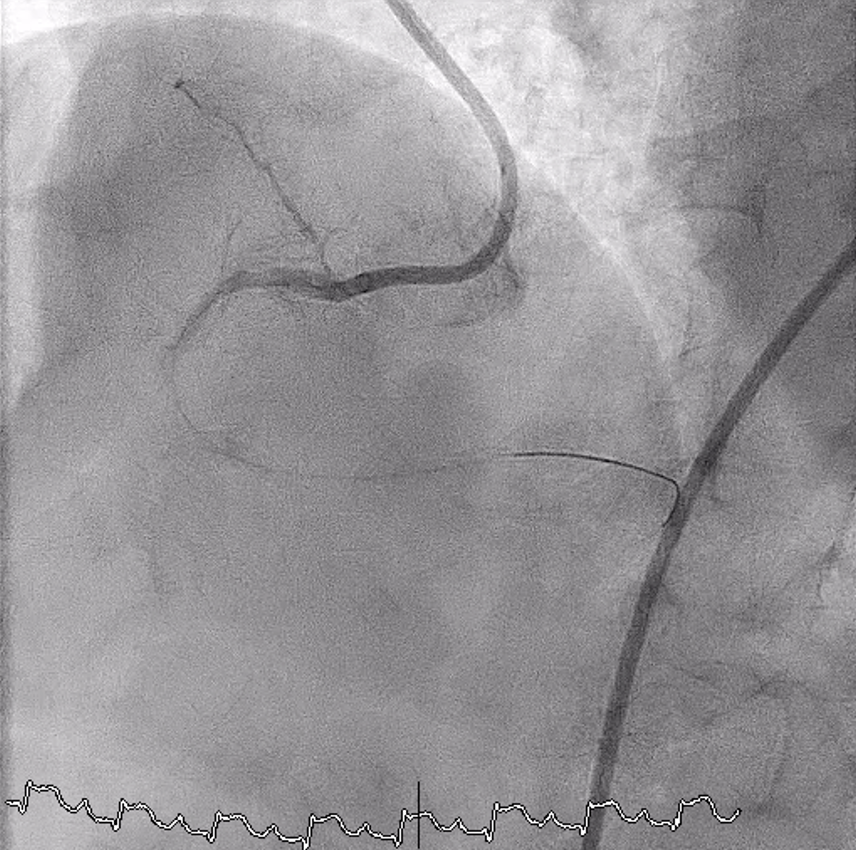
Urgent angiography revealed perforation of a small posterior descending artery branch (Figure 4, Videos 3A and 3B), likely from guidewire trauma (Figure 5). Prolonged balloon tamponade failed; successful sealing was achieved with a 2.0 × 20-mm Nester embolization coil (Cook Medical) (Figure 6, Video 4). No further events occurred.
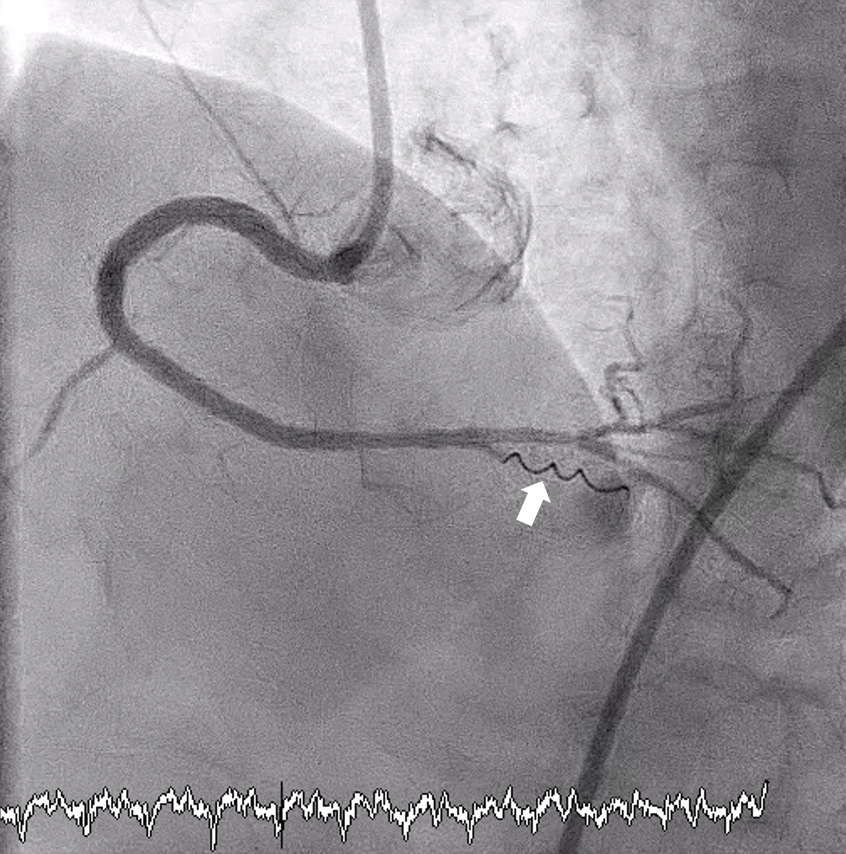
The final coronary angiography of the first PCI was reviewed in details and no distal perforation was revealed. It was likely that the perforation was concealed at the end of the first PCI because of the much lower BP. The delay in presentation was then likely related to the subsequent significant rise in BP, resulting in clinically manifested perforation.
This case demonstrates that distal coronary perforation secondary to guidewire trauma can have delayed manifestation after a rise in BP. In patients undergoing complex PCI with possible distal wire trauma—particularly those with labile or poorly controlled hypertension—close hemodynamic monitoring in the early postprocedural period is essential, even though no perforation may be obvious at the end of the procedure. Delayed distal perforation, although rare, should be considered in cases of sudden deterioration after an initially successful PCI.
Affiliations and Disclosures
Kwok-Ho Yau, MBBS; Tin Wah Christopher Lau, MBBS; Justin Ka-Ho Wong, MBBS; Kin-Lam Tsui, MBBS, FACC
From the Cardiology Team, Department of Medicine, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong SAR.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient(s) for the study and/or intervention(s) described in the manuscript and for the publication of their data/thereof, including any and all images.
Address for correspondence: Kwok-Ho Yau, MBBS, 3 Lok Man Road, Chai Wan, Hong Kong. Email: jason200200200@hotmail.com