BASILICA With Adjunctive Coronary Protection Enabling Valve-in-Valve Transcatheter Aortic Valve Implantation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00380. Epub December 29, 2025.
An 81-year-old woman with prior surgical aortic valve replacement (19-mm MAGNA bioprosthesis [Edwards Lifesciences], 10 years prior) presented with progressive dyspnea (New York Heart Association [NYHA] Class III). Echocardiography showed severe bioprosthetic aortic stenosis (aortic valve maximum velocity [Vmax]: 3.5 m/s; mean gradient: 28 mm Hg; aortic valve area [AVA]: 0.7 cm²) with mild paravalvular leak and preserved ejection fraction. Stress echocardiography increased the Vmax to 4.7 m/s with a mean gradient of 43 mm Hg and an AVA of 0.8 cm². Computed tomography (CT) revealed low coronary heights with ultra-low virtual transcatheter valve-to-coronary (VTC) distances (left main: 1.6 mm; right coronary artery: 2.4 mm), indicating prohibitive risk for coronary obstruction during valve-in-valve (ViV) transcatheter aortic valve implantation (TAVI).
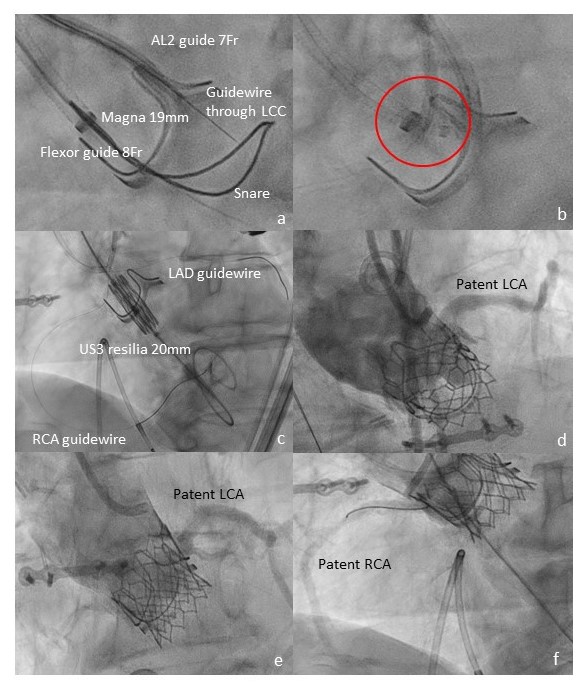
Given this high-risk anatomy, BASILICA (Bioprosthetic or Native Aortic Scallop Intentional Laceration to Prevent Iatrogenic Coronary Artery Obstruction)1 was planned. Under general anesthesia, a denuded 0.014-inch Astato guidewire (ASAHI INTECC) was advanced transleaflet within a microcatheter using radiofrequency energy. The wire was snared in the left ventricular outflow tract to form the laceration loop; only the left leaflet was targeted because of predominant left main risk (Video 1). Prophylactic coronary wiring was performed. Following successful leaflet laceration, a 20-mm SAPIEN 3 Ultra RESILIA valve (Edwards Lifesciences) was implanted with additional postdilation (Video 2). Final angiography confirmed unobstructed coronary flow and optimal valve expansion without regurgitation (Figure).
The patient recovered uneventfully and discharged on day 3. She reported NYHA I symptoms at 30 days and 6 months with excellent valve hemodynamics.
ViV TAVI in small surgical valves poses substantial coronary obstruction risk, particularly when the VTC distances are less than 2 to 3 mm. In this case, BASILICA combined with selective coronary protection enabled safe ViV implantation in a 19-mm prosthesis, avoiding chimney stenting or redo surgery. This report adds to the early experiences of BASILICA performed with the SAPIEN 3 Ultra RESILIA platform and emphasizes the importance of CT-based risk stratification and individualized protection strategies.
BASILICA with adjunctive coronary protection is an effective strategy to mitigate coronary obstruction in high-risk ViV TAVI, expanding treatment options for patients with degenerated small surgical bioprostheses.
Affiliations and Disclosures
Konstantinos Stathogiannis, MD, FACC; Michael Chrissoheris, MD; Kyriakos Katsianos, MD; Vivi Grammata, MD; Alexis Dimas, MD; Konstantinos Spargias, MD
From the Transcatheter Heart Valves Department, Hygeia Hospital, Marousi, Greece.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for this study described in the manuscript and to the publication, including any and all images.
Address for correspondence: Konstantinos Stathogiannis, MD, FACC, Transcatheter Heart Valves Department, Hygeia Hospital, Erythrou Stavrou 9, 15123, Marousi, Greece. Email: kstathog@hotmail.com
References
- Khan JM, Dvir D, Greenbaum AB, et al. Transcatheter laceration of aortic leaflets to prevent coronary obstruction during transcatheter aortic valve replacement: concept to first-in-human. JACC Cardiovasc Interv. 2018;11(7):677-689. doi:10.1016/j.jcin.2018.01.24