Performance of Large Language Models in Interventional Cardiology: The ILLUMINATE Blinded Model-Comparison Study
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00104. Epub November 21, 2025.
Abstract
Objectives. Large language models (LLMs) have the potential to assist in complex decision making for interventional cardiology (IC). However, their comparative performance in providing clinical recommendations remains uncertain. In this blinded model‑comparison study, the authors evaluated and compared the quality of recommendations produced by 6 LLMs for complex IC cases.
Methods. Twenty detailed and complex clinical cases focusing on coronary artery disease (n=10) and structural heart disease (n=10) were developed. Six LLMs were tested: default ChatGPT (ChatGPTd), ChatGPT with European Society of Cardiology guidelines (ChatGPT-gl), ChatGPT with internet search enabled (ChatGPTi), Gemini (Google), Mistral 7B (Mistral AI), and Perplexity AI (Perplexity AI, Inc.). Only the ordering of anonymized outputs was randomized to ensure blinding. Five expert ICs independently assessed the anonymized and randomized responses using a 0 to 10 scale for appropriateness, accuracy, relevance, clarity, and clinical utility, generating a composite score. Statistical analysis was performed using a mixed linear model.
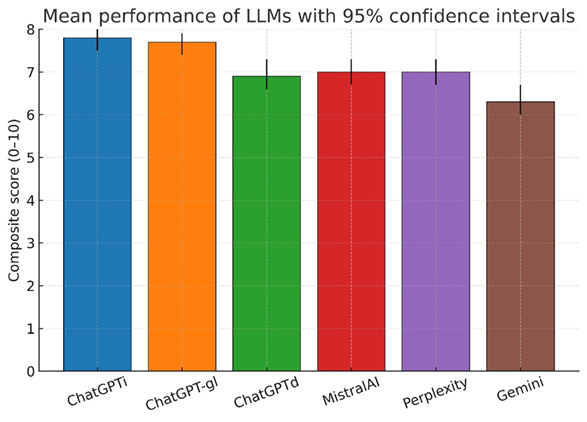
Results. Six hundred blinded evaluations (20 cases x 6 models x 5 raters) were analyzed, yielding an overall composite score of 7.1 (95% CI, 7.0-7.2). Performance significantly varied across LLMs (P < .001), with ChatGPTi (7.8 [7.5-8.0]) and ChatGPT-gl (7.7 [7.4-7.9]) outperforming others. ChatGPTd (6.9 [6.6-7.3]), Mistral 7B (7.0 [6.7-7.3]), and Perplexity AI (7.0 [6.7-7.3]) performed moderately, while Gemini had the lowest score (6.3 [6.0-6.7]). These differences were consistent across all scoring dimensions (P < .001). Case type did not affect LLM performance (P = .900).
Conclusions. LLMs show promise in IC decision making, but their performance remains suboptimal. Maximizing their potential requires systematic integration of web search capabilities and guideline-based knowledge retrieval.
Introduction
The rapid evolution of artificial intelligence (AI) presents new and original opportunities for enhancing clinical support, particularly in diagnostics, therapeutics, and decision-making processes. Current literature indicates that AI represents a valuable tool in clinical decision making, especially within fields like cardiology, where its ability to process complex datasets and real-time analysis can provide significant support to clinicians.1-7 Furthermore, recent research has demonstrated instances where large language models (LLMs) like ChatGPT (OpenAI) have not only matched, but even surpassed the diagnostic accuracy and completeness of responses provided by emergency room physicians and cardiologists in specific scenarios.8 For instance, ChatGPT-4o achieved 100% correct responses in evaluations of cardiovascular emergencies and provided faster, more comprehensive answers than its human counterparts, including cardiologists, in detailed scenarios.8 Similarly, in the context of patient education about coronary artery disease (CAD), ChatGPT delivered accurate and reproducible responses.8
However, several challenges remain, such as variability in AI outputs, errors in interpreting clinical queries, and issues with accuracy, which underscore the need for cautious and controlled implementation in medical practice.3,4,6,7,9 Integration into routine practice is challenging; moreover, effectiveness and accuracy remain active concerns given imperfect performance and occasional hallucinations.4,7,8,10 Although several studies have investigated the diagnostic performance of LLMs in general cardiology and emergency care, their effectiveness in guiding complex interventional cardiology (IC) decisions has not been systematically evaluated using blinded assessments by expert operators.4 Continued research and development are fundamental to fully take advantage of AI’s capabilities in real-world clinical settings.
In this study, we evaluated the performance of various AI-based LLMs in addressing 20 complex IC cases. Rather than comparing AI responses directly with those of cardiologists, the study focused on assessing the quality of AI-generated responses as judged by experienced ICs, using standardized criteria including appropriateness (guideline-concordance), accuracy (scientific correctness), relevance (focus on the case), clinical utility (actionability/decisiveness/feasibility within standard care), and clarity (organization, unambiguity). To mirror how clinicians encounter these tools, we purposively included both proprietary systems (eg, GPT-4 family, Gemini, Perplexity) and an open-source model (Mistral), reflecting different access models and update cadences. We also contrasted purely parametric chatbots with configurations that add retrieval (web browsing) and a guideline-anchored scaffold, allowing us to test whether structured access to contemporaneous European Society of Cardiology (ESC) guidance improves adherence, decisiveness, and clinical realism. Our objective was to analyze the strengths, limitations, and variability in performance among different AI models, focusing on their current capabilities and role in IC. This paper aims to provide insights into how AI can complement clinical decision making, identify key areas for improvement, and discuss the challenges and opportunities for future advancements in this rapidly evolving field.
Methods
Study design
The ILLUMINATE study is a prospective, blinded, model‑comparison study designed to evaluate the performance of various LLMs in dealing with complex IC scenarios. Randomization was applied only to the order of the anonymized model outputs presented to evaluators to ensure blinding. No participants were randomized to interventions; therefore, trial registration was not applicable. The objective was to compare the ability of these models to provide appropriate, accurate, and clinically useful responses based on predefined criteria.
Ethics
For this study, we used deidentified clinical vignettes with no protected health information or direct electronic health record text. No patient intervention or data linkage were involved. Per institutional policy, it qualified as non-human subject research, so formal institutional review board review was not required.
Clinical case selection
Twenty real-world IC clinical scenarios were selected and administered to 6 different LLMs. Cases were rewritten as deidentified vignettes prior to any LLM interaction. The cases were equally divided between CAD (n = 10) and structural heart disease (SHD) (n = 10). These cases reflected complex scenarios frequently encountered in IC, designed to assess the models’ ability to support clinical decision making.
Evaluated language models, model configuration, customization, and case administration
The 6 LLMs evaluated in the study were ChatGPTd (OpenAI, GPT‑4; default chat configuration; all models were queried between November and December 2024), ChatGPT‑gl (OpenAI, GPT‑4; fixed system prompt privileging ESC guidelines; all models were queried between November and December 2024), ChatGPTi (OpenAI, GPT‑4 with internet browsing enabled; all models were queried between November and December 2024), Gemini (Google, Gemini 1.5 Pro; all models were queried between November and December 2024), Perplexity AI (Perplexity AI, Inc., free tier; all models were queried between November and December 2024), and Mistral 7B (Mistral AI, open‑source; all models were queried between November and December 2024). The guideline corpus pre‑specified for reference included the ESC guidelines for the management of chronic coronary syndromes (2024), ESC guidelines for the management of acute coronary syndromes (2023), ESC/ European Association for Cardio-Thoracic Surgery guidelines for the management of valvular heart disease (2021), ESC guidelines on myocardial revascularization (2018), ESC guidelines on atrial fibrillation (2024), and European Society of Gastrointestinal Endoscopy guidelines on endoscopic diagnosis and management of esophagogastric variceal hemorrhage (2022).
Web browsing was permitted to retrieve current guidance and primary literature. All models were provided with the same clinical cases and received identical text. Clinical cases were administered between November 1, 2024, and December 27, 2024. Where applicable, we recorded the model family, access tier, and month/year of access. Exact model names correspond to the providers’ public labels at the time of use. Each LLM was presented with the clinical case and asked the question: “How would you manage this scenario? What would you do?” If the provided responses were too general or lacked a definitive decision on the management of the clinical case, an additional prompt was administered: “What would you do in the end? Take a final decision.” This approach ensured that all models delivered conclusive recommendations about the management of the presented scenarios. Notably, in the specific scenario of clinical case administration to ChatGPT‑gl (guidelines‑privileged configuration), the corresponding guidelines’ .PDF files were uploaded along with an additional prompt: “Answer according to the European Society of Cardiology guidelines (ESC or others) uploaded for this case,” following the other standard commands administered in every case (“How would you manage this scenario? What would you do?”).
Evaluation criteria
The responses provided by the models were anonymized, randomized, and blindly assessed by 5 expert ICs. We did not include a comparator arm of human-generated recommendations. Because the ICs did not submit their own decisions on the vignettes, this was not a direct human-vs-LLM trial. The evaluation was conducted considering 5 specific criteria: (1) appropriateness, referring to compliance with clinical guidelines and best practices; (2) accuracy, meaning the scientific correctness and precision of the information provided; (3) relevance, measuring how pertinent the responses were to the presented clinical case; (4) clarity, referring to the comprehensibility and coherence of the response; and (5) clinical utility, assessing the practical value of the response in patient management. A composite score was calculated for each response with a maximum of 10 points. We did not pre-specify a binary threshold for correct vs incorrect answers. Instead, accuracy was scored on a 0 to 10 scale by 5 blinded ICs capture gradations from partially correct to fully guideline-concordant answers. Given clinical heterogeneity and acceptable alternative pathways, dichotomizing responses was deemed potentially misleading; accordingly, primary analyses used the continuous scores (accuracy and the composite index).
Randomization and anonymization process
The responses generated by the LLMs were collected and anonymized to prevent evaluation bias. A randomization of the answers was performed using a basic data handling software (Microsoft Excel) to ensure an impartial assessment by the evaluators. When the models quoted external sources or references to guidelines, those were removed from the exported text before grading to preserve blinding. To avoid model identification by style, we removed explicit citations and any provider identifiers from all outputs before randomization.
Statistical analysis
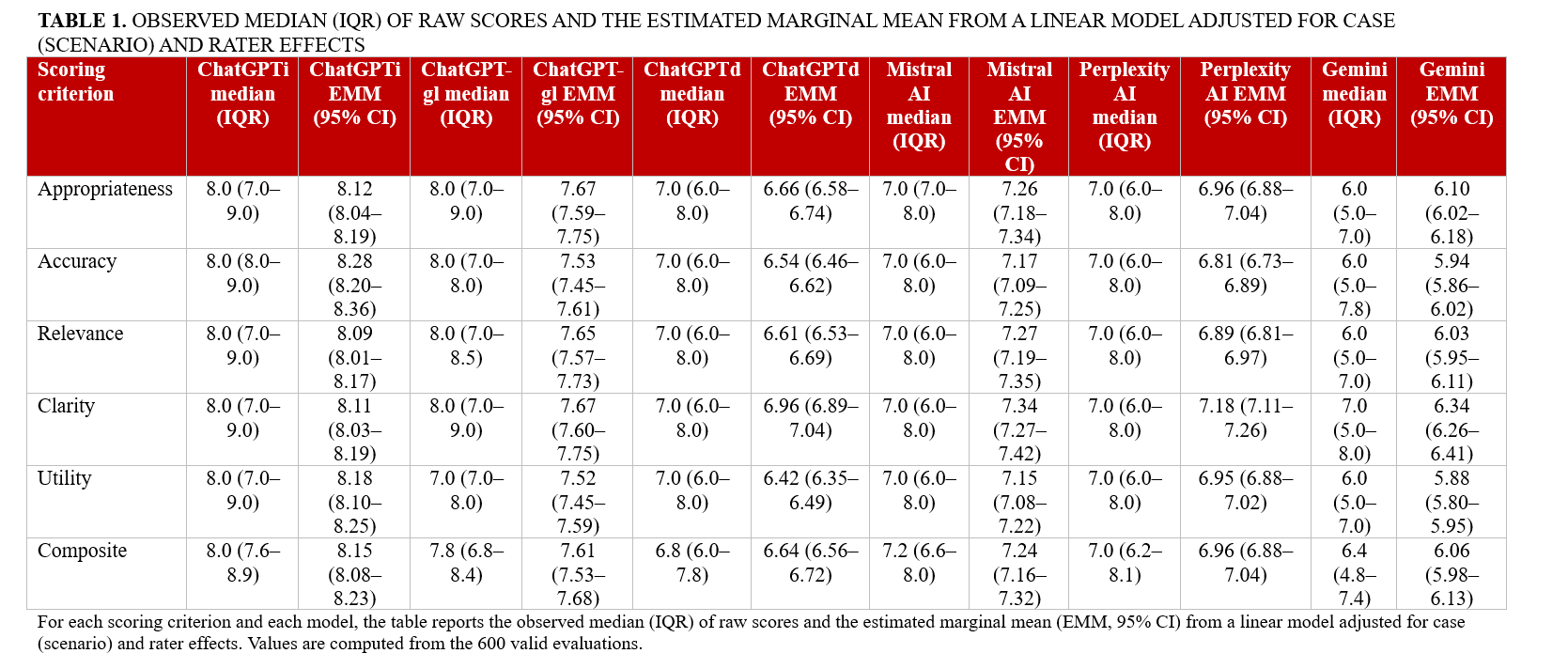
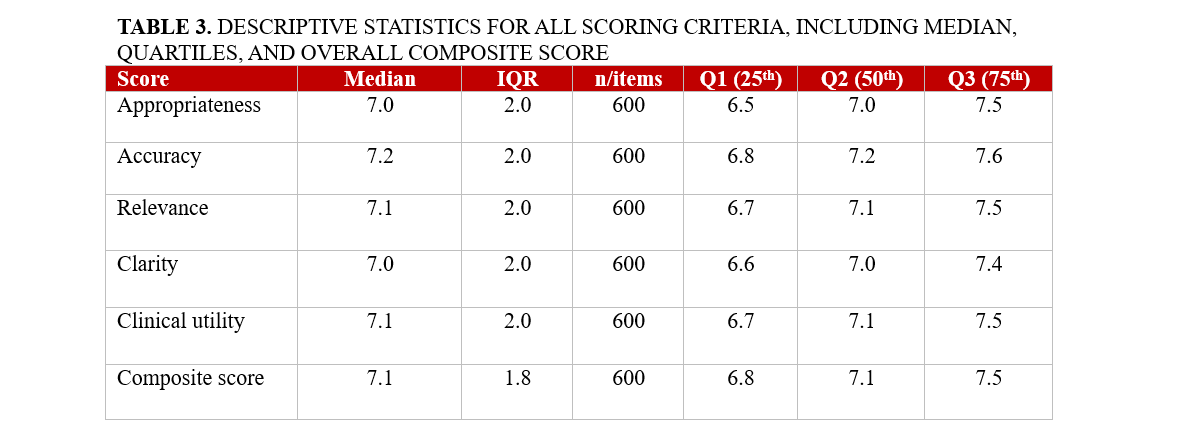
Analyses were performed post-collection in March 2025 using Python (Python Software Foundation) and R (The R Project for Statistical Computing). For descriptive purposes, evaluation scores for each domain and the composite score were reported as medians with IQRs. Inter-rater agreement for composite scores was quantified using a 2-way random-effects, absolute-agreement, single-measure intraclass correlation coefficient [ICC(2,1)] on complete-case evaluations, and agreement in case rankings across evaluators was assessed with Kendall’s coefficient of concordance (W). For inferential comparisons of performance across LLMs, we fitted linear mixed-effects models with random intercepts for case and rater and obtained model-specific estimated marginal means (EMMs) with 95% CIs. Between-model pairwise contrasts were adjusted for multiple testing using false discovery rate (FDR) control within each evaluation criterion. In addition to the composite score analyses, we summarized criterion-level performance for each model. For every scoring criterion (appropriateness, accuracy, relevance, clarity, and clinical utility) and each LLM, we reported both the observed median (IQR) of raw scores and the corresponding EMMs (95% CI) derived from the same mixed-effects framework. These domain-specific results are presented in Table 1 to highlight the strengths and weaknesses of individual models across evaluation dimensions.
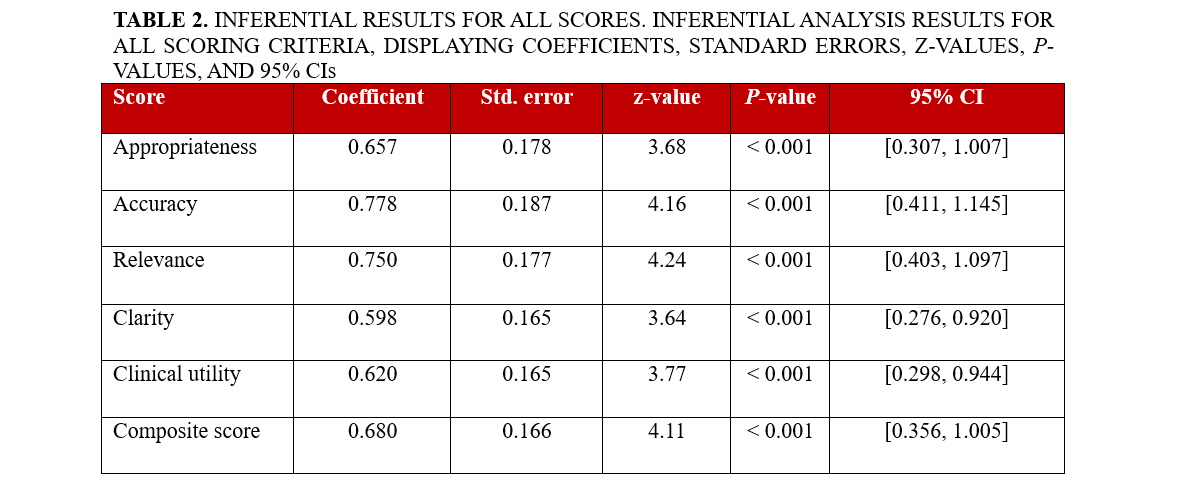
Associations between accuracy and clinical utility were assessed primarily with Spearman’s rank correlation coefficient (ρ, 95% CI), with Pearson’s r and partial correlations (after residualizing for case and rater effects) reported as supportive analyses. A 2-sided P-value of less than 0.05 was considered statistically significant. Additionally, to quantify how each evaluation domain related to perceived clinical utility, we fitted separate linear mixed-effects models with clinical utility as the dependent variable, the domain score as fixed effect, and random intercepts for case and rater; the resulting coefficients, standard errors, z-values, P-values, and 95% CIs are reported in Table 2.
Results
We analyzed 600 blinded evaluations (20 cases × 6 models × 5 raters), corresponding to 120 case-model composite scores. The overall composite score for AI performance in complex IC cases was 7.1 (95% CI, 7.0-7.2). The distribution of domain-specific scores and composite scores is summarized in Table 3. However, significant differences were observed among the models (P < .001). ChatGPTi achieved the highest performance with a composite score of 7.8 (95% CI: 7.5-8.0), followed closely by ChatGPT-gl, which scored 7.7 (95% CI: 7.4-7.9). ChatGPTd performed notably worse, achieving a score of only 6.9 (95% CI: 6.6-7.3). Similarly, Mistral 7B and Perplexity AI both recorded a composite score of 7.0 (95% CI, 6.7-7.3). The lowest-performing model was Gemini, which scored 6.3 (95% CI, 6.0-6.7) (Figure 1; Table 4).
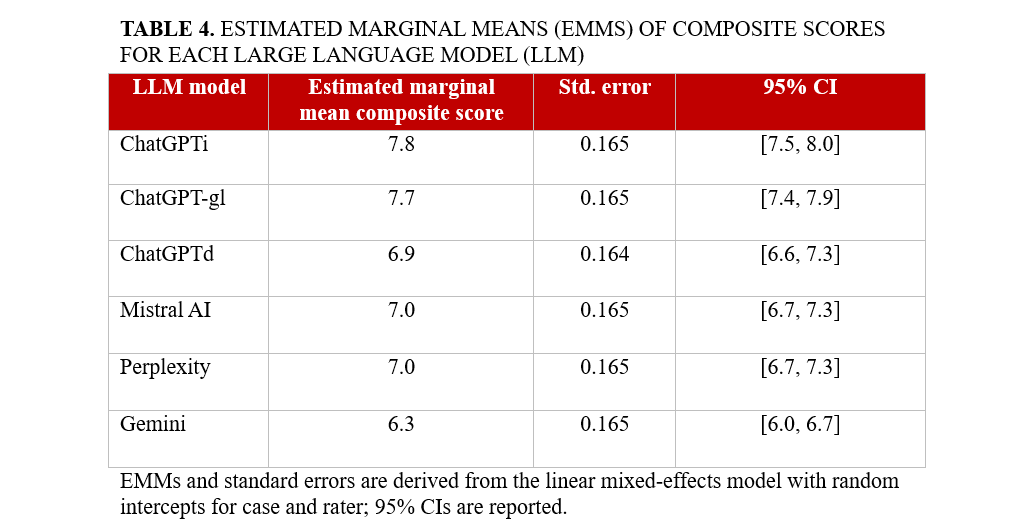
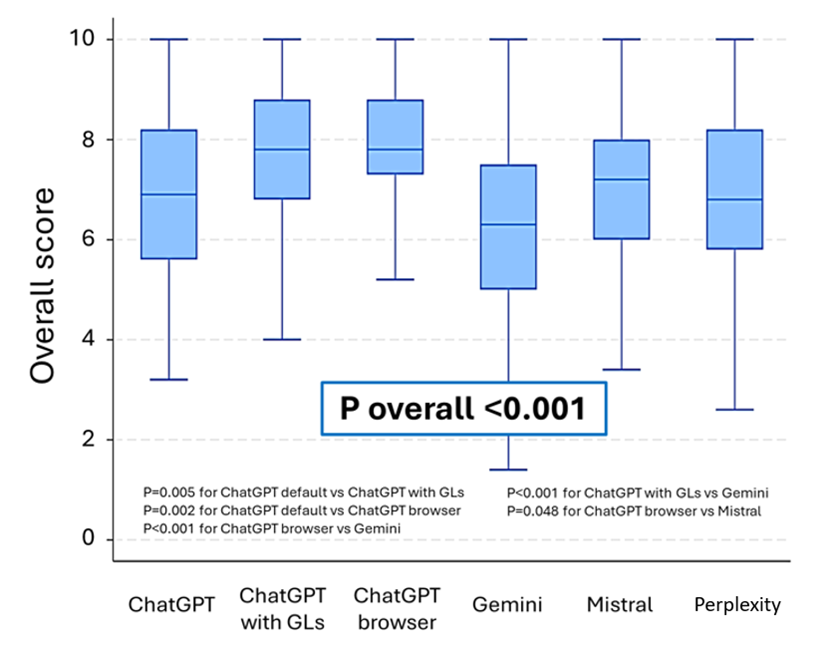
All 5 evaluation criteria (appropriateness, accuracy, relevance, clarity, and clinical utility) followed a similar trend, with ChatGPTi and ChatGPT-gl performing better than the other models (all P < .001). Models equipped with integrated guideline access and internet search capabilities generated more contextually relevant and accurate responses. Criterion-level performance by model is detailed in Table 1. ChatGPTi and ChatGPT-gl consistently achieved the highest median and EMM values across all 5 domains, particularly for appropriateness, accuracy, and clinical utility, confirming their overall superiority across evaluation criteria. Mistral 7B and Perplexity AI showed intermediate performance with generally acceptable scores, whereas Gemini systematically underperformed with lower appropriateness, accuracy, and clarity scores. These domain-specific patterns are fully consistent with the composite score rankings reported in Table 4.
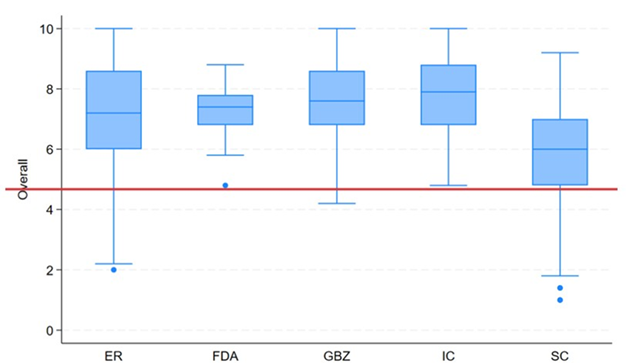
We flagged an additional prompt when a model’s initial output lacked a firm, actionable decision. Extra nudges were frequent with non-scaffolded models—ChatGPTd 15/20 (75%), Gemini 18/20 (90%), Perplexity AI 12/20 (60%), Mistral 7B 13/20 (65%)—and less common with scaffolded variants—ChatGPT-gl 4/20 (20%), ChatGPTi 6/20 (30%). This pattern indicates that guideline/retrieval scaffolding improves first-pass completeness by reducing the need for follow-ups. No significant performance differences were observed between cases related to CAD and those involving SHD (P = .900), suggesting that model performance was consistent across the different domains of IC evaluated in this study.
To test whether clinical utility reflected an independent judgment or was driven by accuracy, we quantified their association across all evaluations (N = 600). Accuracy was strongly correlated with clinical utility (Pearson r = 0.860; 95% CI, 0.838-0.880). This relationship persisted, though attenuated, after controlling for evaluator and model via fixed-effects residualization (partial r = 0.796; 95% CI, 0.764-0.824). Rank-based analyses were consistent (Spearman ρ = 0.826; partial ρ = 0.767; both P < .001). Thus, while clinical utility is not redundant with accuracy, greater accuracy substantially increases perceived clinical usefulness.
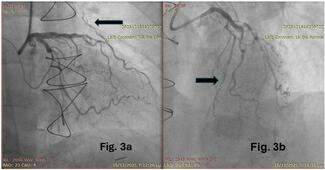
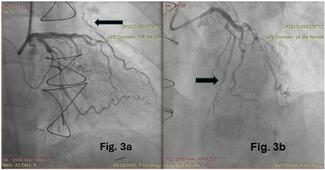
To contextualize between-model differences, we examined how cardiologist evaluators distributed scores across the same items. Figure 2 shows, for each evaluator, the distribution of composite scores (0-10) across complete subjects (ie, case × model combinations with all 5 ratings). Inter-rater reliability for the composite score—estimated with a 2-way random-effects, absolute-agreement, single-measure intraclass correlation—was ICC(2,1) = 0.208 (95% CI, 0.183-0.361), indicating poor absolute agreement between individual raters. Rank concordance across evaluators was Kendall’s W equal to 0.436, P-value of 9.37×10⁻¹², consistent with moderate concordance of ranks. Item-level and composite ratings are reported as median (IQR). Model-level performance panels show EMMs (95% CI) from the mixed model (Figure 3).
Discussion
Our findings extend a rapidly growing literature on LLMs in cardiovascular medicine. Prior studies have shown that LLMs can assist heart-team deliberations in severe aortic stenosis, often aligning with expert consensus while shortening decision cycles.11 Others have documented that off-the-shelf models achieve variable but non-trivial performance on interventional certification items2 and cardiology board-style multiple-choice questions.6 In acute care and general cardiology contexts, LLMs have sometimes matched or exceeded clinicians for specific tasks such as structured diagnostic reasoning or patient-facing education, though results are heterogeneous.2,4,6 Parallel methodological work has emphasized that guideline-aware prompting and retrieval-augmented generation can substantially improve adherence to evidence-based recommendations and that clinical utility hinges on transparency, calibration, and guardrails.12-16
This study provides a global assessment of the use of LLMs in decision making in IC. Through a systematic evaluation of 6 LLMs across multiple real-world cases, we identified key strengths and limitations in their capacity to deliver clinically relevant guidance. The findings of this study underscore the potential of AI-assisted decision making in IC, simultaneously highlighting the important variability in performance among different models. A critical finding of our study is that LLMs with access to external data sources, such as internet-enabled search capabilities (ChatGPTi) or preloaded clinical guidelines (ChatGPT-gl), significantly outperformed their counterparts (highlighted in Figure 1 and Table 4). This suggests that incorporating real-time access to evidence-based guidelines and literature enhances the reliability and applicability of AI-generated recommendations. Conversely, LLMs operating without external data integration, such as Gemini and ChatGPTd, demonstrated lower performance, emphasizing the limitations of static knowledge models in a rapidly evolving field like IC.
IC moves quickly, with frequent updates to antithrombotic therapy, device indications, and imaging-guided optimization. Models that rely on fixed training data and lack targeted retrieval tend to drift from current evidence and may default to generic or incorrect recommendations. By contrast, approaches that surface the latest guidance and explicitly anchor reasoning to class of recommendation and level of evidence statements reduce ambiguity and improve usability. In our evaluation, the web-enabled (ChatGPTi) and guideline-structured (ChatGPT-gl) configurations consistently outperformed the default, purely parametric versions across all 5 domains, with differences that were both statistically and practically significant.
While ChatGPTi and ChatGPT-gl performed well, none of the evaluated models achieved perfect scores, indicating room for improvement and progress to be made. The need for additional prompting to obtain definitive recommendations also highlights current limitations in AI autonomy (inter-evaluator variability illustrated in Figure 2). Designing prompt frameworks that demand a final, accountable decision tied to guideline classes/levels and key contraindications may therefore be a practical lever for improving clinical utility. Moreover, our study focused exclusively on AI-generated recommendations rather than a direct comparison with human decision making, leaving open the question of how LLMs compare to expert cardiologists in real-world patient management.
Limitations
Despite its design, our study has several limitations. We took into consideration a small sample of 20 clinical scenarios, which may limit the generalizability of the findings to broader clinical practice. The AI models’ responses could also be influenced by their training data, potentially leading to inconsistent outputs. Extensive web search capabilities and careful adherence to guidelines are also not systematically or explicitly implemented. Furthermore, it is worth considering that the rapid evolution of AI technology may result in findings that quickly become outdated, necessitating continuous evaluation.
Conclusions
The findings of the ILLUMINATE study highlight the significant potential of LLMs in supporting complex decision making in IC. Our analysis of 6 different AI-based models demonstrated notable variability in their performance, with ChatGPT versions that integrate internet search capabilities and ESC guidelines outperforming other models. These enhanced versions provided more appropriate and clinically useful responses compared with their counterparts that lack external information access. Ultimately, while LLMs show potential to help and to support ICs in managing complex cases, their integration into clinical practice is still far from perfect and requires further improvement. Future research should focus on optimizing AI performance through enhanced contextual understanding, real-time data integration, and systematic adherence to medical guidelines. Additionally, regulatory oversight and clinician involvement will be critical in the process of ensuring a safe and effective AI-assisted decision making in cardiology.
These findings may have practical implications for the integration of AI tools into the workflow of ICs. LLMs equipped with real-time internet access and guideline-based databases may be incorporated into clinical decision-support platforms to assist physicians during case planning and periprocedural strategy selection. As AI technology continues to evolve, future development should focus on increasing clinical contextual awareness, minimizing hallucinations, and incorporating regulatory safeguards to ensure patient safety. Prospective studies are needed to validate the real-world impact of LLMs on clinical outcomes and workflow efficiency in the catheterization laboratory.
Affiliations and Disclosures
Attilio Lauretti, MD1-9; Iginio Colaiori, MD1; Simone Calcagno, MD2; Enrico Romagnoli, MD3; Fabrizio D’Ascenzo, MD4,5; Antonio Di Matteo, MD1; Francesco Gemelli, MD1; Gaetano Pero, MD1; Marco Bernardi, MD1-6; Luigi Spadafora, MD1-6; Antonio Esposito, MD8; Marco Borgi, MD1; Giuseppe Biondi-Zoccai, MD, MStat6,7; Francesco Versaci, MD1
From the 1Division of Cardiology, Santa Maria Goretti Hospital, Latina, Italy; 2Cardiology Unit, Department of Emergency and Admission, San Paolo Hospital, Civitavecchia, Italy; 3Department of Cardiovascular Sciences, Fondazione Policlinico Agostino Gemelli IRCCS, Rome, Italy; 4Division of Cardiology, Cardiovascular and Thoracic Department, Città della Salute e della Scienza, Turin, Italy; 5Division of Cardiology, Department of Medical Sciences, University of Turin, Italy; 6Department of Medical-Surgical Sciences and Biotechnologies, Sapienza University of Rome, Latina, Italy; 7Maria Cecilia Hospital, GVM Care & Research, Cotignola, Italy; 8ICOT Marco Pasquali Institute, Cardiovascular Department Latina; 9Department of Clinical and Molecular Medicine, Sapienza University of Rome, Rome, Italy.
Disclosures: Dr Biondi-Zoccai has consulted for Abiomed, Advanced Nanotherapies, Aleph, Amarin, Balmed, Cardionovum, Crannmedical, Endocore Lab, Eukon, Guidotti, Innovheart, Meditrial, Menarini, Microport, Opsens Medical, Terumo, and Translumina, outside the present work. The remaining authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Attilio Lauretti, MD, Division of Cardiology, Santa Maria Goretti Hospital, Via Lucia Scaravelli, 04100 Latina, Italy. Email: attilio.lauretti@uniroma1.it; Instagram: @attiliolauretti
Supplemental Material
The clinical cases administered to the AI-search engines, asking them to take a final decision on the management. Answers from the AI search engines are listed below each case.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER ONE: High-risk SCA-NSTE complicated by respiratory failure in an elderly patient with multiple comorbidities.
Premises:
An 82-year-old male patient, obese and smoker with arterial hypertension, dyslipidemia, hyperuricemia, peripheral vascular disease and COPD entered the emergency room for severe dyspnea and severe chest pain that occurred while climbing the stairs.
Vital signs: blood pressure 190/100 mmHg, HR 105 bpm, Spo2 88%, RR 25 per minute.
Physical examination: clear heart sounds, signs of pulmonary congestion, mild peripheral edema, widespread wheezing and whistles over all lung fields.
ECG: sinus rhythm at a mean heart rate of 110 bpm, significant ST segment depression from V1 to V4 and widespread nonspecific repolarization changes.
Echocardiogram: reduced ejection fraction (45%) with hypokinesia of the anterolateral wall. Hypertrophic right sections with preserved systolic function indices (TAPSE 17 mm). Moderate tricuspid regurgitation.
Blood gas analysis: pH 7.32 pO2 50 mmHg pCO2 20 mmHg Lac 3.5 HCO3- 25 mEQ/L.
Flectadol 250 mg IV, Clexane 8,000 IU SC, Lasix 60 mg IV were administered. Urbason 40 mg IV was administered. Oxygen therapy with non-invasive ventilation was set. Due to the persistence of high blood pressure values and severe chest pain, nitrates were administered in continuous intravenous infusion.
Blood tests: troponin 15,000, WBC 20,000, PCR 8.0, Hb 15 g/dl, Creatinine 2.0, platelets 200,000
With intravenous nitrate therapy chest pain decreased but did not disappear and blood pressure partially decreased. Despite optimization of ventilation with the use of a helmet and additional intravenous cortisone, bronchospasm and respiratory failure persisted. After a few minutes and an increase in the dosage of nitrates, chest pain disappeared and arterial pressure returned to normal values, but dynamic alterations of ventricular repolarization appeared on the ECG.
ANSWERS
ChatGPT
Default configuration
Early Invasive Coronary Angiography After Stabilization. In summary, the approach would be to stabilize the patient further with ongoing medical management and then proceed with early invasive coronary angiography when hemodynamic and respiratory parameters are more favorable.
Interrogation after upload of guidelines (ESC ACS 2023) and supplementary data
In light of the patient's clinical condition and according to the guidelines, here’s the final recommended course of action:
1. Immediate Coronary Angiography
Given the high levels of troponin, dynamic ST-segment changes, and persistent symptoms, this patient is at high risk for a major coronary event. An immediate coronary angiography is recommended to identify any critical coronary obstruction. If a significant blockage is found, percutaneous coronary intervention (PCI) should be performed to restore coronary flow and reduce myocardial ischemia. This invasive strategy aligns with best practices for managing non-ST elevation ACS in high-risk patients.
2. Stabilization in Intensive Care
While awaiting or post-angiography, the patient should remain in an intensive care unit to closely monitor cardiac function, oxygenation, and blood pressure. This level of care helps manage any complications from COPD, hypertension, or potential acute heart failure.
3. Medical Optimization
Continue oxygen therapy and non-invasive ventilation to address hypoxia and COPD exacerbation.
Adjust medications as necessary: Optimize nitrates to manage chest pain while avoiding hypotension, continue anticoagulation, and maintain bronchodilators and corticosteroids for COPD.
4. Evaluate for Secondary Prevention Post-Stabilization
After stabilization, secondary preventive measures should focus on controlling hypertension, dyslipidemia, and smoking cessation to reduce future cardiovascular risks. Long-term antithrombotic therapy and lifestyle changes will be crucial here.
This approach addresses both the acute ischemic and respiratory needs of the patient while following the 2023 ESC guidelines on high-risk ACS management(acs 2023 ing)(acs supplementary data).
Interrogation to ChatGPT browser
Here’s a structured approach:
1. Initial Stabilization and Symptom Control
Continue Oxygen Therapy and Non-Invasive Ventilation (NIV): Given the low oxygen saturation (SpO₂ 88%) and respiratory distress, continue NIV (helmet or mask) to improve oxygenation. Monitor for any signs of further respiratory compromise, as intubation may be necessary if respiratory failure worsens.
Control of Hypertension and Chest Pain: Nitrates should be continued carefully, titrating to maintain symptom relief and blood pressure control. Since his blood pressure has partially stabilized, further BP and pain management may involve careful IV nitrates, avoiding hypotension.
Anticoagulation and Anti-Ischemic Therapy: Enoxaparin (Clexane) has already been started, which should be continued for ACS. Given his elevated troponin (15,000), the goal is to prevent thrombosis while planning for potential coronary intervention. Consider adding an antiplatelet agent like aspirin if not contraindicated, though clopidogrel or ticagrelor may be withheld until definitive coronary assessment due to bleeding risks.
2. Management of Respiratory Failure and COPD Exacerbation
Corticosteroids: Methylprednisolone (Urbason) should continue to manage COPD exacerbation, and bronchodilators (e.g., nebulized albuterol and ipratropium) can be administered cautiously, especially if NIV provides sufficient ventilatory support.
Diuretics: IV Lasix (furosemide) should continue to reduce pulmonary congestion and improve respiratory function, titrating the dose to avoid hypovolemia, especially since his kidney function is impaired (creatinine 2.0).
Electrolyte Monitoring: Regular monitoring of electrolytes (K⁺, Mg²⁺) is necessary due to diuretics and potential arrhythmias, with supplementation as required.
3. Coronary Intervention Plan
Urgent Coronary Angiography: Given persistent chest pain, dynamic ECG changes, elevated troponins, and high-risk ACS, this patient requires coronary angiography to evaluate and treat any culprit lesions. Although high-risk due to age and comorbidities, angiography is indicated in this setting of refractory angina with hemodynamic and respiratory compromise.
PCI vs. Conservative Management: If a culprit lesion is found, percutaneous coronary intervention (PCI) with drug-eluting stents is likely preferable to surgery due to his age, COPD, and overall risk profile. CABG would generally be avoided unless absolutely necessary.
4. Address Renal Function and Potential Nephrotoxicity
Given his elevated creatinine, minimize nephrotoxic agents and ensure adequate hydration (without fluid overload). Use the lowest effective dose of contrast during angiography to prevent further renal impairment.
5. Final Decision and Goals
Proceed with Urgent Coronary Angiography and Possible PCI: The primary goal is symptom relief, stabilization, and prevention of myocardial damage by identifying and addressing coronary blockages. This decision is high priority given the patient's refractory chest pain, hemodynamic fluctuations, and elevated troponins.
Continued Monitoring and Intensive Care Support: Place the patient in the ICU for close monitoring of respiratory status, hemodynamics, and renal function post-intervention. Further cardiovascular and respiratory support may be needed, with adjustments based on clinical progress.
In summary, the final decision is to perform urgent coronary angiography with a view to PCI if feasible to address the high-risk ACS, while maintaining intensive medical management for his respiratory failure, ACS, and comorbidities. This approach balances immediate stabilization with a potentially life-saving intervention.
Gemini
Immediate PCI with close respiratory monitoring. It is recommended rapid stabilization with intubation and mechanical ventilation (: If non-invasive ventilation is insufficient).
Perplexity AI
Early Invasive Coronary Angiography After Stabilization. Once the patient is stabilized (e.g., improved oxygenation, resolution of severe dyspnea), proceed with early invasive coronary angiography to assess coronary anatomy and determine the need for revascularization.
Mistral AI
early invasive coronary angiography (within 24 hours) with continued optimization of respiratory status (with non invasive ventilation).
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER TWO: Stable angina in elderly patient with multiple comorbidities.
Premises:
78-year-old patient, ex-heavy smoker, suffering from arterial hypertension, type 2 diabetes on insulin therapy, dyslipidaemia, COPD. Despite the comorbidities, he was an independent patient at home and carries out almost all daily activities alone. Since nearly three months, onset of episodes of chest pain related to light physical effort, lasting about 30 minutes and regressing with rest. The patient was admitted electively to the cardiology department to undergo coronary angiography.
Physical examination: clear heart sounds, no signs of central and peripheral stasis.
ECG: sinus rhythm at an average heart rate of 85 bpm, nonspecific alterations of ventricular repolarization.
Echocardiogram: increased wall thickness, normal dimensions, EF 50% with hypokinesia of the lateral wall. Other findings within the norm.
Blood tests: creatinine 1.3, Hb 14.5 g/dl, PLT 150,000.
Coronary angiography was performed which showed: three-vessel critical coronary artery disease; critical stenosis of the proximal tract of the anterior interventricular artery, critical stenosis of the proximal tract of the circumflex artery and critical stenosis of the proximal-middle tract of the right coronary artery. Distal segments of the vessels of good quality; syntax score was 22.
ANSWERS
ChatGPT:
Default configuration
Final Decision:
PCI seems like the most reasonable choice for this patient, given the moderate Syntax score and the patient’s age and comorbidities. The distal vessels are of good quality, and the procedural risks of multivessel PCI are generally lower than CABG in this population.
CABG should still be considered if the PCI procedure is deemed technically difficult or if there are concerns about the long-term durability of PCI in this patient. If PCI is unsuccessful or complications arise, CABG would be an option at a later stage.
Medical optimization (antiplatelet therapy, statins, antihypertensives, and diabetic control) should continue alongside the decision to proceed with PCI or CABG.
Conclusion: I would proceed with PCI as the first-line intervention for this patient, given the moderate complexity of the coronary anatomy and the patient's comorbid conditions. If PCI is unsuccessful or complications arise, CABG would be reconsidered.
Interrogation after upload of ESC guidelines (ESC 2018 revascularization, ESC CCS 2024)
Given the critical three-vessel coronary artery disease with significant stenoses and a SYNTAX score of 22 in this patient, the ESC guidelines suggest that coronary artery bypass grafting (CABG) should be considered as the preferred revascularization strategy, especially in multivessel disease where a complete revascularization approach is beneficial to improve long-term survival and reduce cardiac events.
Interrogation to ChatGPT browser
Final Decision: Proceed with PCI with Drug-Eluting Stents:
Given his age, comorbidities, relatively stable EF, and intermediate Syntax score, PCI with drug-eluting stents to treat critical lesions in all three vessels is a suitable choice. This approach aims to improve his symptoms with a shorter recovery time and lower procedural risk compared to CABG.
Plan for Close Monitoring Post-PCI: Due to his comorbid conditions, regular follow-ups will be essential to monitor his angina symptoms, diabetes, blood pressure, and COPD status.
In conclusion, proceeding with PCI with drug-eluting stents is the final decision, prioritizing symptom relief with a lower-risk approach, followed by aggressive secondary prevention and close monitoring.
Gemini
Recommended Approach: Given the patient's age, comorbidities, and the severity of coronary artery disease, a CABG may be the most appropriate option.
Perplexity AI
The decision to proceed with CABG offers the best potential for long-term survival and quality of life improvement for this patient with complex coronary artery disease.
Mistral AI
Given the patient's complex three-vessel disease and the potential long-term benefits, CABG is the most appropriate management strategy. This decision balances the need for complete revascularization with the patient's clinical characteristics and comorbidities, aiming to improve symptoms and long-term prognosis.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER 3: NSTEMI and electrical instability in a young patient
Premises:
45-year-old patient, heavy smoker, suffering from hypertension, obesity, dyslipidemia and DM; positive anamnesis for drug abuse. He gets to the Emergency room suffering from acute chest pain and SOB during a night party, claiming that he experienced similar symptoms recently, especially when he was making significant physical efforts.
Physical examination: clear heart sounds, no signs of pulmonar stasis, no edema; High blood pressure (190/100 mmHg).
ECG: sinus rhythm at an average heart rate of 95 bpm, nonspecific alterations of ventricular repolarization.
Echocardiogram: increased wall thickness, EF 40 % with hypokinesia of the apex and anterolateral wall. Mild IM.
Blood tests: creatinine 1.4; HB 14; WBC: 13000; High troponine values.
NSTEMI diagnosis was made and the patient was conducted in ICU, in order to be stabilized and perform a coronary angiography once lowered the blood pressure values (IV nitrates were started). Suddenly, the patient complains about palpitations and oppressive chest pain. An other EKG was made:
This showed polymorphic ventricular tachicardia that caused a significant pressure drop (85/40 mmHg);
ANSWERS
ChatGPT
Default configuration
In the end, after stabilizing the patient with immediate interventions (such as cardioversion and medication), the final decision would focus on the following key steps. Once the patient is stabilized from the acute arrhythmia and hemodynamic instability, perform coronary angiography to assess for significant coronary artery disease that may be contributing to the NSTEMI and electrical instability.
Interrogation after upload of guidelines (ESC 2023 ACS)
Given the patient's sudden development of polymorphic ventricular tachycardia (VT) leading to hypotension in the setting of NSTEMI, urgent management is required as per the latest ESC guidelines. Here’s a recommended approach based on these guidelines and the provided information:
Immediate Stabilization:
Initiate advanced cardiac life support (ACLS) protocol, as this VT is causing hemodynamic instability.
If VT persists and the patient remains hypotensive (85/40 mmHg), immediate synchronized electrical cardioversion is warranted to restore normal sinus rhythm.
Pharmacological Support:
While preparing for cardioversion, administer IV amiodarone if available, as it is effective in controlling ventricular arrhythmias in NSTEMI.
For refractory VT, consider additional anti-arrhythmic agents as per ACLS guidelines and guidelines specific to acute coronary syndromes(acs 2023 ing)(acs supplementary data).
Ongoing Management:
Continue IV nitrates to manage blood pressure once stabilized, adjusting to avoid hypotension.
Optimize beta-blocker therapy (once stable) to reduce myocardial oxygen demand and arrhythmia risk, unless contraindicated.
Following stabilization, perform urgent coronary angiography to assess the need for revascularization, as myocardial ischemia may be contributing to electrical instability.
Intensive Monitoring:
Monitor with continuous ECG, and perform serial troponins and imaging to evaluate infarct size and recovery.
Assess need for further arrhythmia prophylaxis, and potentially consider an implantable cardioverter-defibrillator (ICD) if VT persists or there is high risk for recurrent arrhythmia.
This approach ensures rapid intervention to address both hemodynamic compromise and underlying ischemic triggers for VT.
Interrogation to ChatGPT browser
Immediate Management of Polymorphic VT
Immediate Electrical Cardioversion: Given the hemodynamic instability (BP 85/40 mmHg), immediate synchronized cardioversion is indicated. PVT, especially in the setting of ischemia, is unlikely to self-terminate and can rapidly deteriorate into ventricular fibrillation. This is critical to stabilize the patient's rhythm and blood pressure.
Intravenous Antiarrhythmic Therapy:
Amiodarone: Following successful cardioversion, intravenous amiodarone can be initiated to help stabilize the myocardium and prevent recurrence of arrhythmias. Initial bolus followed by a continuous infusion is typical.
Lidocaine: Alternatively, if amiodarone is contraindicated or ineffective, lidocaine may be used as an adjunct, particularly if there is ongoing ischemia or in cases of drug-related arrhythmias.
Optimize Myocardial Oxygen Supply and Demand:
IV Nitroglycerin: Continue IV nitrates to control blood pressure and reduce myocardial oxygen demand. Ensure blood pressure remains within a stable range (target <140/90 mmHg if possible) while avoiding hypotension.
Beta-Blockers: Avoid initially, as they may worsen hypotension in this acute setting. Beta-blockers may be reconsidered after stabilization to reduce heart rate and oxygen demand.
Correct Electrolyte Imbalances:
Ensure potassium levels are maintained at 4.0-4.5 mmol/L and magnesium at 2.0 mg/dL to minimize arrhythmogenic potential.
Administer IV magnesium sulfate empirically, as it can be beneficial in the context of PVT even in the absence of hypomagnesemia.
Stabilization and Further Work-Up
Immediate Coronary Angiography:
Given the patient’s NSTEMI and high-risk features (e.g., persistent chest pain, high troponin, electrical instability), immediate coronary angiography should be performed after initial stabilization to assess for acute coronary occlusion or severe coronary artery disease requiring intervention.
Percutaneous coronary intervention (PCI) should be performed if a culprit lesion is identified.
Consideration of Mechanical Support:
If blood pressure remains unstable despite interventions, temporary mechanical circulatory support (such as an intra-aortic balloon pump or, in refractory cases, Impella or extracorporeal membrane oxygenation) may be considered, especially if significant left ventricular dysfunction is noted on echo.
Longer-Term Anti-Ischemic and Arrhythmic Strategy:
Beta-Blockers: Once the patient is hemodynamically stable, beta-blockers can be introduced to reduce arrhythmic risk and manage hypertension, titrating carefully in the setting of heart failure.
ACE Inhibitors/ARBs: These should be introduced after stabilization, considering his left ventricular dysfunction and history of hypertension, diabetes, and NSTEMI.
Statins: Initiate high-dose statin therapy early in hospitalization as part of secondary prevention.
Monitoring and Observation
Continuous telemetry monitoring in the ICU is essential given his high risk of recurrent arrhythmias.
Re-assess with repeat echocardiogram and potentially cardiac MRI later to evaluate for structural heart changes (e.g., cardiomyopathy or scar tissue) that might predispose to recurrent arrhythmias.
In summary, this patient’s management hinges on rapid cardioversion, antiarrhythmic stabilization, correction of any modifiable ischemic factors, and expeditious assessment and intervention for coronary artery disease. Close monitoring and a comprehensive secondary prevention strategy will also be crucial for long-term management and prevention of recurrence.
Gemini
Final Decision: Immediate Stabilization (suggested administration of amiodarone or magnesium sulfate to terminate the PVT) and Early PCI. Given the patient's presentation with NSTEMI and PVT, a rapid and aggressive approach is necessary.
PerplexityAI
Perform synchronized electrical cardioversion to treat the unstable polymorphic ventricular tachycardia (VT) in the patient with NSTEMI and significant hypotension (85/40 mmHg). Plan for coronary angiography once the patient is stabilized.
MistralAI
Immediate Defibrillation and Advanced Cardiac Life Support (ACLS) Protocol, followed by urgent coronary angiography once the patient is stabilized.
----------------------------------------------------------------------------------------------------------------------CASE NUMBER FOUR: A peculiar case of chest pain in a recently revascularized patient
Premises:
64 year-old patient; heavy smoker, family history of CAD.
The patient accessed the Emergency room suffering from acute oppressive chest pain occurring at rest and lasting almost 2 hours. PA: 180/90 mmHg.
ECG: Sinus rhythm at an average heart rate of 65 bpm, ST segment elevation and hyperacute T in the anteroseptal leads
Echocardiogram: increased wall thickness, EF 45 % with hypokinesia of the anterolateral wall. Mild to moderate MR, mild AR.
Thus, he was immediately conducted to the Cath lab in order to perform an emergency coronary angiography, that showed significant stenosis of the ADA, treated with angioplasty and deployment of a stent (3,5 x 33 mm) on mid ADA. The other vessels showed no significant stenosis.
After that, the patient reached the ICU, he was monitored and blood test were made. After few hours, the patient experienced another similar episode of chest pain, blood pressure was ok (120/85 mmHg) and ECG showed no significant alterations. However the pain was not responsive to IV nitrates and painkillers, so the decision to perform an other angiography was made.
This one showed optimal result of the stent previously deployed, but a detail showed up: there was a significant myocardial bridge at the distal edge of the stent.
ANSWERS
ChatGPT
Default configuration
Optimize Medical Therapy. Start or adjust the dose of beta-blockers to reduce myocardial oxygen demand. Consider adding a calcium channel blocker to help prevent vasospasm. If not already on board, initiate long-acting nitrates for chronic angina management.
Interrogation after upload of guidelines (ESC CCS 2024 and ACS 2023)
In summary, I would start with optimized medical therapy using beta-blockers, avoid nitrates, and monitor closely. Further invasive intervention would only be considered if symptoms persist.
Interrogation to ChatGPT browser
The primary approach is intensive medical therapy with beta-blockers and possibly calcium channel blockers to manage ischemia from the myocardial bridge. Avoid nitrates and focus on heart rate control to reduce systolic compression. If symptoms persist despite optimal medical therapy, consult for potential surgical myotomy. This plan provides a balance between effective ischemia management and minimally invasive intervention, with the goal of symptom relief and prevention of recurrent ischemia.
Gemini
Continue Medical Management. Optimize current medications: Ensure the patient is taking appropriate doses of antiplatelet agents, beta-blockers, statins, and potentially ACE inhibitors or ARBs to optimize cardiac health.
PerplexityAI
Continue Medical Management. Optimize Medical Therapy: Ensure that the patient is on optimal doses of antiplatelet therapy (e.g., aspirin and possibly clopidogrel), beta-blockers, ACE inhibitors, and statins. Consider adding antianginal medications such as ranolazine or long-acting nitrates if angina persists.
Mistral AI
Medical Therapy Optimization. Ensure the patient is on optimal medical therapy, including aspirin, a P2Y12 inhibitor (like clopidogrel or ticagrelor), a statin, and a beta-blocker or calcium channel blocker for symptom control.
----------------------------------------------------------------------------------------------------------------------CASE NUMBER FIVE: A complex case: STEMI and simultaneous massive gastrointestinal bleeding.
Premises:
A 65 year old male patient, suffering from arterial hypertension, diabetes, dyslipidaemia, liver cirrhosis (HCV related). Frequent drugs abuse in medical history. The patient was admitted to the emergency room for massive hematemesis. At the admission general conditions were poor, arterial blood pressure was 85/60 mmHg, cardiac frequency 60 beats per minute. Immediately after the access in the emergency department, strong chest pain occurred and and ECG was performed.
ECG: inferior STEMI with supra-ST elevation in inferior leads and right precordial leads.
Blood exams: Hb 8.0 g/dl, Low platelet count (30.000/ul), serum creatinine 1,1 mg/dl.
Echocardiography: it showed an EF of 45% with akinesia of the inferior wall of the left ventricle and a strongly reduced contractility of the free wall of the right ventricle (Tapse 6 mm).
ANSWERS
ChatGPT
Default configuration
In summary, prioritize stabilization (fluid resuscitation, blood products, and managing the GI bleed), and then assess the feasibility of urgent coronary angiography based on the patient's stability and response to initial treatments. If the patient is unstable, focus first on the gastrointestinal issue before proceeding to address the cardiac concerns.
Interrogation after upload of guidelines ESC ACS 2023 and ESGE guidelines
Here's a strategy drawing from both ESC guidelines for acute coronary syndromes and ESGE guidelines on variceal hemorrhage:
1. Stabilizing Circulatory and Hemodynamic Status:
Fluid Resuscitation: Administer fluids cautiously to support blood pressure without exacerbating right ventricular overload.
Blood Products: Transfuse red blood cells and platelets as needed to manage active bleeding, maintaining hemoglobin and avoiding transfusion-induced fluid overload, as per ESGE’s restrictive transfusion approach in stable patients(ESGE guidelines).
Vasopressors: Norepinephrine can be initiated for maintaining adequate mean arterial pressure (MAP), particularly as fluids alone may be insufficient in a setting of right ventricular strain.
2. Urgent Gastroenterology Intervention for Hemostasis:
Endoscopic Therapy: Perform endoscopy within 12 hours for hemostasis, ideally with band ligation for esophageal varices, following ESGE recommendations(ESGE guidelines).
Pharmacologic Management: Start vasoactive agents such as octreotide or terlipressin to reduce portal hypertension and control variceal bleeding, with a course of up to 5 days(ESGE guidelines).
Prophylactic Antibiotics: Initiate ceftriaxone to prevent sepsis, as per ESGE's recommendation for patients with cirrhosis and GI bleeding(ESGE guidelines).
3. Management of STEMI:
Modify Standard ACS Care Due to Bleeding Risks: Dual antiplatelet therapy (DAPT) is typically avoided due to active bleeding and thrombocytopenia, which aligns with ESC's careful approach in bleeding risk patients(esc acs 2024ù).
Primary Percutaneous Coronary Intervention (PCI): Collaborate with cardiology to evaluate options like aspiration thrombectomy or minimal stenting, potentially with lower anticoagulation strategies(esc acs 2024ù).
Right Ventricular Support: Avoid excessive fluids, and use norepinephrine for hemodynamic support of the right ventricle(esc acs 2024ù).
4. Intensive Monitoring and ICU Admission:
Given the critical instability, ICU admission is essential for close monitoring of hemodynamics, renal function, and potential rebleeding. Use frequent clinical reassessment to detect deterioration early.
5. Multidisciplinary Coordination:
Team Approach: Coordinate with cardiology, gastroenterology, and ICU teams to address the competing needs of managing both ACS and variceal bleeding, consulting hepatology as needed for liver disease management.
Final Decision Strategy:
Begin by stabilizing hemodynamics and controlling GI bleeding. Proceed with limited cardiac intervention if bleeding stabilizes to manage the high-risk STEMI cautiously. Continue vasoactive, endoscopic, and antibiotic interventions as indicated for bleeding control and infection prevention.
This balanced, multidisciplinary approach is crucial given the complexities in managing both bleeding and cardiovascular instability in a high-risk patient.
Interrogation to ChatGPT browser
Here’s a structured approach to this complex case:
1. Immediate Hemodynamic Stabilization
Fluid Resuscitation and Blood Product Transfusion:
IV Fluids: Begin cautious fluid resuscitation with crystalloid solutions to support blood pressure without overloading, especially given the patient’s cirrhosis.
Blood Transfusion: Rapidly administer red blood cells to increase hemoglobin levels, aiming for a target Hb ≥8–9 g/dL, as anemia could worsen myocardial ischemia. Consider transfusing fresh frozen plasma (FFP) and platelets, given the low platelet count and cirrhotic coagulopathy, but be cautious of volume overload.
Vasoactive Support: Initiate low-dose vasopressors (e.g., norepinephrine) if hypotension persists despite fluid and transfusion efforts to maintain adequate coronary and systemic perfusion.
2. Simultaneous Management of GI Bleeding
Urgent Gastroenterology and Endoscopy: Arrange for immediate GI consultation and prepare for endoscopy to locate and treat the source of bleeding.
Pharmacologic Support for Variceal Bleeding: Given the cirrhosis and likely portal hypertension, initiate therapy with intravenous octreotide to reduce portal pressure, and consider proton pump inhibitors (PPIs) to mitigate upper GI bleeding. If esophageal varices are suspected, band ligation or sclerotherapy can be performed during endoscopy.
Consider Temporary Reversal of Coagulopathy: Correct coagulopathy with FFP and platelets to reduce active bleeding, with the caveat of not overly raising portal pressure.
3. Management of Inferior STEMI
Reperfusion Strategy:
Primary Percutaneous Coronary Intervention (PCI) is typically preferred for STEMI, but balancing this with bleeding risk is complex in this scenario. Due to the active GI bleed, traditional anticoagulation and dual antiplatelet therapy (DAPT) pose a high risk.
If feasible, perform PCI with careful use of minimally necessary anticoagulation (e.g., a single bolus of heparin) without routine DAPT initially, and consider bare-metal stent (BMS) placement or even balloon angioplasty alone to minimize the need for prolonged antiplatelet therapy.
Alternative Approaches: If PCI is not immediately feasible due to the bleeding risk, consider delaying until hemodynamics stabilize, while providing supportive care for myocardial ischemia and closely monitoring for complications.
4. Balancing Bleeding and Antithrombotic Therapy
Limited Use of Antiplatelet Agents: With a critical platelet count of 30,000/μL and active GI bleeding, hold or minimize antiplatelet agents until bleeding is controlled and platelets are at a safer level (>50,000/μL).
Post-PCI Strategy: If PCI is successfully performed and bleeding is controlled, consider low-dose aspirin monotherapy temporarily until it is safe to add a P2Y12 inhibitor (e.g., clopidogrel). Platelet transfusion may be needed to maintain a safer platelet level if antiplatelet agents are initiated.
5. Post-Intervention Monitoring and Support
ICU Admission: Place the patient in an intensive care unit (ICU) for close hemodynamic and bleeding monitoring, with frequent reassessment of hemoglobin, platelet counts, and hemodynamic stability.
Optimize Heart Failure Management: The right ventricular dysfunction and reduced TAPSE (6 mm) suggest significant right-sided heart strain. Support with cautious diuresis if volume overload is evident but balance against hypovolemia risks. Pulmonary vasodilators or inotropes may be needed if right ventricular failure worsens.
Multidisciplinary Team Involvement: Engage a team with cardiology, gastroenterology, critical care, and hematology for coordinated management of this high-risk case.
Summary of Final Management Decision
In summary, the immediate priorities are stabilizing hemodynamics and addressing the GI bleed, then performing urgent PCI with a minimalistic antithrombotic approach. This strategy offers a balance between life-saving myocardial reperfusion and bleeding control, with careful post-PCI monitoring to address any ongoing risk of ischemia or recurrent bleeding.
Gemini
My final decision would be to:
Prioritize immediate resuscitation and stabilization of the patient.
Consult with a multidisciplinary team of experts, including cardiologists and gastroenterologists.
Carefully assess the risks and benefits of reperfusion therapy and endoscopic intervention.
Develop a tailored management plan based on the individual patient's circumstances.
Closely monitor the patient's condition and adjust the management plan as needed.
Remember, this is a general approach and should not be taken as medical advice. Always consult with a qualified healthcare professional for personalized guidance.
PerplexityAI
Final Decision
Immediate Resuscitation:
Initiate Fluid Resuscitation: Administer IV fluids rapidly to address hypotension (BP 85/60 mmHg). Start with crystalloids and consider blood transfusions to raise hemoglobin levels, targeting a more stable hemodynamic state.
Cardiac Management:
Reperfusion Therapy: Given the presence of STEMI, proceed with Primary Percutaneous Coronary Intervention (PCI) as the first-line treatment if facilities are available and the patient is stable enough for transport. If PCI cannot be performed quickly, consider thrombolytics while being cautious about the risk of exacerbating gastrointestinal bleeding.
Gastrointestinal Management:
Consult Gastroenterology: Urgently involve a gastroenterologist for assessment and potential endoscopy to manage the source of gastrointestinal bleeding. This may include interventions like band ligation or sclerotherapy if variceal bleeding is suspected.
Start Proton Pump Inhibitors (PPIs): Administer PPIs to manage gastric acidity and reduce the risk of further bleeding.
Monitoring and Support:
Continuous Monitoring: Maintain close monitoring of vital signs, cardiac rhythm, and laboratory parameters (especially hemoglobin and platelet count).
Multidisciplinary Team Approach: Engage cardiology, gastroenterology, and critical care teams to ensure comprehensive management.
Consideration of Surgical Options:
If endoscopic intervention fails or if there is significant ongoing bleeding, be prepared for surgical intervention to control the source of gastrointestinal bleeding.
Conclusion
The final decision is to proceed with immediate resuscitation, initiate reperfusion therapy for STEMI, consult gastroenterology for gastrointestinal bleeding management, and ensure continuous monitoring and multidisciplinary support. This approach aims to stabilize the patient while addressing both critical conditions effectively.
MistralAI
Given the hemodynamic instability and the concurrent inferior STEMI with right ventricular involvement, the patient should undergo urgent coronary angiography first, despite the bleeding. The rationale is that ongoing myocardial ischemia can lead to further hemodynamic compromise and even cardiac arrest.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER SIX: An unstable angina in an “angry” patient.
Premises:
A 78-year-old male patient, smoker, suffering from arterial hypertension, dyslipidaemia, atrial fibrillation, COPD. Previous revascularization 10 years before with PCI and positioning of 1 DES on the proximal tract of right coronary artery. In the last year the patient experienced episodes of typical angina occurring after discussions with his family and in the last 10 months for efforts of intermediate intensity, such as cleaning the garden and climbing two floors of stairs. General conditions of the patients were good despite comorbidities and he was autonomous in the ordinary daily activities. Patient was admitted electively to the hospital to undergo a coronary angiography.
ECG: atrial fibrillation at 80 bpm, anomalies of ventricular repolarization.
Echocardiography: hypertrofic left ventricle, ejection fraction of 48% with hypokinesia of the inferior and posterior walls.
Blood tests: Hb 15 g/dl, creatinine 1 mg/dl, platelets 170.000, WBC 9.000.
Coronary angiography: chronic total occlusion of the proximal tract of right coronary artery, partially revascularized downstream by heterocoronary and homocoronary collateral circulations, sub occlusive stenosis of the proximal tract of the left main (not involving the distal part), sub occlusive stenosis of the circumflex artery (not involving the bifurcation with interventricular anterior artery) and significant stenosis at the proximal-medium tract of interventricular anterior artery. Distal vessels were all good without presence of diffuse atheromatic illness. Syntax score was 46.
ANSWERS
ChatGPT
Default configuration
CABG is likely the best therapeutic option for this patient, considering his complex coronary anatomy, significant functional impairment, and overall clinical profile. A multidisciplinary approach involving cardiology and cardiothoracic surgery will be crucial for optimal management.
Interrogation after upload of guidelines (ESC 2018 revascularization and CCS 2024) and supplementary data
For this high-risk 78-year-old male patient with significant multivessel coronary artery disease (CAD), including sub-occlusive stenosis of the left main coronary artery (LMCA), chronic total occlusion of the right coronary artery (RCA), and a SYNTAX score of 46, the recommended approach would be:
Primary Recommendation: CABG
Given the involvement of the left main and multivessel disease with a high SYNTAX score, coronary artery bypass grafting (CABG) is strongly recommended. CABG has been shown to provide improved outcomes over percutaneous coronary intervention (PCI) in cases with high SYNTAX scores, complex anatomy, and left main involvement(revascularization ESC 2…).
CABG is likely to offer more complete revascularization, addressing all critical lesions and providing better long-term survival and symptom relief.
Heart Team Discussion
Given the patient’s comorbidities, including atrial fibrillation and COPD, a Heart Team (comprising interventional cardiologists, cardiothoracic surgeons, anesthesiologists, and pulmonologists) should assess surgical risk and confirm the feasibility of CABG.
Medical Optimization and Perioperative Considerations
Antithrombotic Therapy: In preparation for CABG, the patient should be on aspirin, with other antithrombotics withheld until post-surgery.
Anticoagulation for AF: Given the atrial fibrillation, anticoagulation needs to be managed carefully. The team may initiate anticoagulation postoperatively to reduce stroke risk, potentially combining it with aspirin if the bleeding risk is manageable.
COPD Management: Optimize COPD therapy preoperatively to reduce pulmonary risk during and after surgery.
Heart Failure Management: Begin or adjust heart failure medication, including beta-blockers, ACE inhibitors, and statins, based on the patient’s tolerance and comorbid status.
Shared Decision-Making with the Patient and Family
Discuss the risks and benefits of CABG versus PCI, emphasizing CABG’s potential for better long-term outcomes and relief of angina. Given the patient's autonomy and independence, CABG may help maintain quality of life by addressing the ischemic burden more comprehensively.
Postoperative Follow-Up and Rehabilitation
Plan for cardiac rehabilitation post-CABG to optimize recovery, improve functional capacity, and manage risk factors long-term.
Final Decision:
CABG is the preferred intervention due to the complex CAD and high SYNTAX score. This approach aligns with ESC guidelines, aiming to improve both survival and quality of life(LG SCC ing)(revascularization ESC 2…).
Interrogation to ChatGPT browser
Final Decision Summary: Given the complexity and extent of disease, the best course is to proceed with CABG for this patient. CABG provides comprehensive revascularization for his high-risk coronary anatomy, including the left main and multi-vessel disease, with expected improvements in symptoms, quality of life, and long-term survival.A careful discussion with the patient and family regarding the risks, benefits, and goals of care is crucial to ensure alignment with the patient's preferences and expectations.
Gemini
The optimal therapeutic option will depend on the patient's individual risk factors, comorbidities, and preferences. A multidisciplinary team, including a cardiologist, cardiac surgeon, and other specialists, should be involved in the decision-making process.
PerplexityAI
I would recommend proceeding with elective coronary artery bypass grafting (CABG). Prior to making this decision, I would ensure that a multidisciplinary team, including cardiology and cardiothoracic surgery, has evaluated the patient’s overall health status and surgical risks.
MistralAI
Recommend Coronary Artery Bypass Grafting (CABG) for this patient. I would also ensure that the heart team agrees with this decision and that the patient is optimized medically before the procedure.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER SEVEN: A complex three vessel disease.
Premises:
59-year-old patient, suffering from arterial hypertension, dyslipidemia, chronic renal failure. Smoker. Stable angina since 4 months for slight efforts.
ECG: sinus rhythm at mean HR of 85 BPM, ventricular repolarization abnormalities.
Echocardiography: EF 50%, preserved wall thickness, anterior wall hypokinesia. Mild aortic stenosis.
Elective coronary angiography: three-vessel coronary artery disease with common trunk with eccentric subcritical calcific stenosis in the distal segment; anterior interventricular artery with severe stenosis (90%) in the mid-segment; circumflex artery with 70% stenosis at the ostium. Patency of the previously implanted stent; right coronary artery with diffuse atheromatous and calcific disease with stenosis of 70% in the mid-segment. Inability to overcome the lesion on the anterior interventricular artery with coronary guidewires.
ANSWERS
ChatGPT
Default configuration
Given the patient's three-vessel disease and significant stenosis in the anterior interventricular artery (90%), along with the left ventricular dysfunction, coronary artery bypass grafting (CABG) may be the preferred option over percutaneous coronary intervention (PCI). CABG would likely provide better long-term outcomes, especially in the presence of complex multivessel disease and left ventricular dysfunction. The inability to traverse the lesion in the anterior interventricular artery with guidewires suggests that PCI may not be feasible or may carry a higher risk of complications.
Interrogation after upload of guidelines (ESC 2024 CCS and ESC revascularization 2018)
In this case, given the patient’s complex three-vessel disease and inability to cross the lesion in the anterior interventricular artery with guidewires, coronary artery bypass grafting (CABG) would be the preferred choice.
Rationale for CABG:
1. Severity and Accessibility of Lesions: CABG is generally recommended for patients with three-vessel disease, especially when one or more vessels cannot be accessed by PCI, as in this case.
2. Improved Prognosis and Symptom Relief: CABG has been shown to provide better long-term survival and relief of symptoms in patients with multivessel disease, particularly in those with significant stenoses like this patient.
3. Patient's Risk Profile: The patient’s comorbidities (chronic renal failure, hypertension, and smoking) place him at higher risk of future cardiovascular events. CABG could offer a more definitive revascularization with a likely reduction in re-intervention needs compared to PCI.
Thus, a recommendation for CABG with continued guideline-directed medical therapy to manage symptoms, control risk factors, and optimize long-term outcomes would be the final decision.
Interrogation to ChatGPT browser
Given the severity and extent of the coronary artery disease, CABG is the preferred revascularization strategy if the patient is deemed a surgical candidate after risk stratification. This approach has the potential for complete and durable revascularization, which is particularly beneficial in complex three-vessel disease. However, if CABG is too high-risk, consideration of advanced PCI with plaque modification techniques may be an alternative, albeit with the understanding that results may be suboptimal given the complexity of lesions and calcification.
Gemini
Given the severity of the stenosis in the anterior interventricular artery and the inability to cross it with guidewires, percutaneous coronary intervention (PCI) is not feasible in this case. Therefore, the most appropriate management strategy for this patient would be coronary artery bypass grafting (CABG).
PerplexityAI
Given the patient's significant three-vessel disease and severe stenosis in the LAD, I would recommend proceeding with elective CABG as the best therapeutic option. This approach aligns with current guidelines for managing complex coronary artery disease, particularly when significant functional impairment is present.
MistralAI
Given the complexity of the coronary artery disease, the inability to overcome the LAD lesion with PCI, and the patient's relatively young age, the best possible decision for this patient would be to recommend CABG.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER EIGHT: Three vessels disease and iliac-aorta aneurisms.
Premises
A 79-year-old patient with arterial hypertension, type 2 diabetes mellitus, dyslipidemia. A recent angio-TC found bilateral aneurysm of 4 cm of the iliac arteries in bifurcation with the abdominal aorta. Dyspnea for about 6 months on mild exertion. Impairment in activity daily life; patient could stand up and go to the toilet by himself but could not drive or having a long walk.
ECG: sinus rhythm at 80 BPM, alterations in ventricular repolarization.
Echocardiogram: preserved wall thickness and dimensions, EF 45% with diffuse global hypokinesia. Moderate mitral regurgitation.
Coronary angiography: three-vessel coronary artery disease with calcific subocclusive stenosis in the mid-distal segment of the anterior interventricular artery, subocclusive stenosis in the proximal segment of the right coronary artery, long subocclusive stenosis in the proximal-mid segment of the circumflex artery, in bifurcation with the first diagonal branch.
Syntax score 22.
ANSWERS
ChatGPT
Default configuration
Final Decision:
Coronary Revascularization:
Proceed with CABG (Coronary Artery Bypass Grafting) given the complexity of the three-vessel disease, reduced ejection fraction (45%), and the patient's significant symptoms of heart failure. CABG is generally preferred in cases like this, especially with the potential for improved outcomes in terms of survival and symptom relief.
Vascular Surgery Consultation:
Refer the patient for a vascular surgery evaluation regarding the 4 cm iliac aneurysms. If the aneurysms pose a significant risk or if symptoms worsen, consider endovascular repair or open surgical options as indicated.
Interrogation after upload of guidelines (ESC CCS 2024 and revascularization 2018)
Considering the patient’s high cardiovascular risk and complex comorbidities, a careful and prioritized approach to intervention is recommended:
Proceed with Coronary Artery Bypass Grafting (CABG):
Given the three-vessel coronary disease, high SYNTAX score, and moderate left ventricular dysfunction (EF 45%), CABG is preferred over PCI. The ESC guidelines for revascularization endorse CABG for multivessel disease when the SYNTAX score is ≥22, as in this case(LG SCC ing)(revascularization ESC 2…). CABG may improve survival and reduce recurrent cardiovascular events compared to PCI in patients with such extensive disease.
Address Aortoiliac Aneurysms Concurrently or Sequentially Based on Risk:
Depending on intraoperative findings and the patient’s stability, the aortoiliac aneurysms can be addressed through endovascular repair, either concurrently with CABG if feasible or as a staged procedure if not. Endovascular repair might offer a safer approach given the patient’s age and frailty, as it is less invasive than open surgery(revascularization ESC 2…).
Optimize Medical Therapy Pre- and Post-Surgery:
Antiplatelet Therapy: Initiate aspirin preoperatively and consider dual antiplatelet therapy post-CABG, with close monitoring for bleeding risk.
Lipid-Lowering Therapy: Start or intensify statin therapy preoperatively to manage dyslipidemia and continue postoperatively.
Diabetes Management: Adjust glucose-lowering therapy, potentially adding an SGLT2 inhibitor or GLP-1 receptor agonist, which are recommended in diabetic patients with cardiovascular disease for additional cardiovascular protection(LG SCC ing)(revascularization ESC 2…).
Beta-Blockers and ACE Inhibitors: Continue or initiate as tolerated to manage dyspnea and optimize cardiac function, given the patient’s moderate EF and mitral regurgitation.
Postoperative Follow-Up:
Engage in regular follow-up to monitor cardiac function, graft patency, aneurysm stability, and overall functional status. Rehabilitative support may help improve activity levels and quality of life, particularly given the patient’s current limitations with exertion(LG SCC ing).
Final Decision: A heart team meeting should prioritize CABG with potential endovascular repair of the aortoiliac aneurysms either in tandem or as a staged intervention. This comprehensive approach aligns with ESC recommendations, optimally balancing risk management with potential for improving the patient’s quality and duration of life.
Interrogation to ChatGPT browser
In the final decision for this 79-year-old patient with multi-vessel coronary artery disease and bilateral iliac aneurysms, I would prioritize coronary artery bypass grafting (CABG) over percutaneous coronary intervention (PCI), with coordinated monitoring and management of the aneurysms. Here’s the rationale for this approach:
Coronary Revascularization via CABG:
Why CABG?: CABG offers a more durable and effective revascularization approach for complex three-vessel disease, particularly in patients with diabetes, as it reduces long-term mortality and the risk of recurrent myocardial ischemia compared to PCI.
Multi-Disciplinary Team Involvement: A heart team, including a cardiac surgeon, cardiologist, and vascular surgeon, should be involved to assess the risks given the patient’s aneurysms and to plan surgical access routes carefully. CABG could be done with aneurysm surveillance unless complications arise.
Monitoring and Managing Aneurysms:
Surveillance: Given the aneurysms are stable at 4 cm, continue with non-interventional management and serial imaging (e.g., every 6 to 12 months). Aneurysms in this size range generally do not warrant immediate repair unless symptomatic or growing rapidly.
Surgical Coordination: Preoperative planning should ensure that surgical access or vascular perfusion is optimized to avoid stress on the aneurysms, with consideration for intraoperative monitoring by the vascular team.
Medical Optimization and Rehabilitation:
Heart Failure Optimization: Maximize heart failure therapy pre- and post-CABG to improve symptoms and maintain functional capacity.
Risk Factor Control: Intensive management of diabetes, hypertension, and dyslipidemia should be continued, along with lifestyle modifications and close follow-up.
Final Decision Summary
Proceed with CABG as the revascularization strategy due to the complex coronary anatomy and diabetes, with ongoing non-interventional monitoring of the iliac aneurysms and pre- and post-operative optimization of heart failure and risk factors. This decision aims to balance effective treatment of ischemic heart disease with safe management of aneurysms.
Gemini
Given the complex medical situation of the patient, a multidisciplinary approach is essential. Here's a potential final decision:
Cardiac Management:
PCI: Based on the coronary angiography findings, percutaneous coronary intervention (PCI) is likely to be the preferred treatment for the significant coronary artery disease. This would improve blood flow to the heart muscle and potentially alleviate symptoms like dyspnea.
Vascular Management:
Endovascular Aneurysm Repair (EVAR): If the patient's anatomy is suitable, EVAR would be the less invasive option for the iliac aneurysms. This procedure would involve inserting a stent graft to reinforce the weakened vessel wall.
Open Surgical Repair: If EVAR is not feasible, open surgical repair would be considered. This would involve a more extensive surgery with a longer recovery period.
PerplexityAI
Final Decision: Revascularization Approach: CABG First
Proceed with CABG: Given the SYNTAX score of 22, the presence of three-vessel disease, and the patient's symptomatic heart failure status, CABG should be prioritized over PCI. This approach is supported by evidence indicating that CABG provides better long-term outcomes in similar patient populations.
Surgical Planning
Coordinate with a multidisciplinary team including cardiology and vascular surgery to:
Address the coronary artery disease through CABG.
Evaluate the timing and necessity for intervention on the bilateral iliac artery aneurysms post-cardiac stabilization.
MistralAI
Based on the provided information and the discussion above, here's a final decision for the management of this complex patient:
Urgent Endovascular Aneurysm Repair (EVAR):
Given the size of the bilateral iliac artery aneurysms (4 cm), they should be addressed urgently to prevent rupture. EVAR is a less invasive option compared to open surgical repair, and it allows for a potentially faster recovery.
Coronary Artery Bypass Grafting (CABG) following EVAR:
The patient has complex three-vessel coronary artery disease with a high Syntax score of 22, favoring CABG over PCI.
After successful EVAR and a brief recovery period to ensure stability and optimize the patient's condition, CABG should be performed to achieve complete revascularization. The Heart Team should aim to perform CABG within a reasonable time frame following EVAR to minimize the risk of cardiac events while the patient awaits surgery.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER NINE: Diabetes and ACS: A case of N-STEMI in a decompensated diabetic patient.
Premises:
59 years old patient, heavy drinker, obese, no medical follow-up because of difficult social condition. Gets to the hospital taken by his wife because of a soporose state and confusion.
Blood analysis: HB: 14 g/dL; creatinine 1,5 mg/dL (eGFR: 90 ml/min); glycate HB: 14%; Glycemia: 690 mg/dL; Troponine Hs 18 (n.v. 1); LDL: 190 mg/dL; trygliceride: 600 mg/dL
The EGA showed metabolic acidodis with high potassium level.
So the patient was diagnosed of iperglycaemic coma and specific treatment was done. However, due to the patient condition and the absence of chest pain, no significant attention to the EKG was payed.
ECG: synus rhythm and negative deep T waves (from v4 to v6) and diphasic T in V3. So another troponine determination was made (meanwhile the patient mental condition was getting better, he was at that time responsive and iperglycemia was properly corrected) showing a higher value (35). The ECG was revalued and so, the clinicians made the diagnosis of Wellens syndrome.
ANSWERS
ChatGPT
Default configuration
Final Decision:
Transfer the patient for urgent coronary angiography to assess coronary artery patency and determine the need for intervention (e.g., angioplasty or stenting).
While awaiting the procedure, ensure continuous monitoring, maintain glycemic control, and manage electrolyte imbalances.
This approach addresses the immediate life-threatening cardiac risk while also stabilizing the patient’s overall condition.
Interrogation after upload of guidelines (ESC 2023 ACS)
Immediate Cardiac Monitoring and Medical Stabilization:
Place the patient in a monitored setting for continuous ECG and vitals monitoring. Monitor glucose and potassium levels closely due to the hyperglycemic state and high potassium on initial labs.
Manage hyperglycemia aggressively with insulin to avoid further cardiac stress and complications, following protocols for diabetic ketoacidosis if indicated.
Early Invasive Strategy:
According to the ESC guidelines for acute coronary syndrome, an early invasive approach (within 24 hours) is indicated for patients with NSTEMI who have high-risk features, such as elevated troponin and Wellens syndrome (indicating a high likelihood of left anterior descending artery stenosis)(revascularization ESC 2…)(acs 2023 ing).
Perform coronary angiography to assess the extent of coronary artery disease and determine if revascularization is needed.
Antithrombotic Therapy:
Antiplatelet Therapy: Administer dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (e.g., clopidogrel, ticagrelor) unless contraindicated. For a patient with NSTEMI and Wellens syndrome, DAPT can help prevent further thrombotic events.
Anticoagulation: Start anticoagulation, such as low-molecular-weight heparin (LMWH), during the acute phase until revascularization is completed or unless contraindicated due to bleeding risk(acs 2023 ing).
Lipid and Lifestyle Management:
Given the patient’s LDL of 190 mg/dL, initiate high-intensity statin therapy to target LDL reduction, aiming for <70 mg/dL according to ESC recommendations for secondary prevention in high-risk patients.
Provide counseling on lifestyle changes, including alcohol cessation and dietary adjustments, to reduce cardiovascular risk(revascularization ESC 2…).
Secondary Prevention and Long-Term Management:
After stabilization, focus on secondary prevention measures, including continuation of antiplatelet therapy, statins, and possible addition of a glucose-lowering agent with cardiovascular benefits (e.g., SGLT2 inhibitor) given the patient’s diabetes and obesity(acs 2023 ing).
Final Decision: Conduct coronary angiography promptly to guide revascularization (likely percutaneous coronary intervention, PCI) due to the high-risk features. This approach aligns with ESC recommendations for managing NSTEMI with Wellens syndrome and addresses both the acute and long-term cardiovascular risks associated with the patient’s metabolic profile.
Interrogation to ChatGPT browser
Summary of Final Decision:
This patient requires urgent coronary angiography and likely PCI given Wellens syndrome, coupled with aggressive medical management of diabetes, hyperkalemia, and metabolic acidosis. Following coronary intervention, addressing long-term risk factors and facilitating lifestyle modifications will be critical to prevent recurrence and promote overall cardiovascular health.
Gemini
The final decision in this case would be to immediately proceed with cardiac catheterization. This is the most critical step to assess the severity of the coronary artery stenosis and to intervene with percutaneous coronary intervention (PCI) if necessary.
PerplexityAI
In this scenario, the final decision would be to proceed with urgent cardiac catheterization. This step is critical due to the diagnosis of Wellens syndrome, which indicates a high risk of an impending myocardial infarction due to significant coronary artery occlusion, particularly in the left anterior descending artery (LAD).
MistralAI
Based on the given information and the high suspicion of Wellens syndrome, which is a pre-infarction stage of proximal LAD occlusion, the final decision would be to proceed with urgent coronary angiography with a view to revascularization.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER TEN: A subacute anterior STEMI.
Premises:
History of presentation: A 79-year-old woman was admitted to the Emergency Department with shortness of breath, swollen ankles and cognitive impairment. Vital parameters were normal (Heart Rate 90 bpm and Arterial Blood Pressure 110/80 mmHg) The patient reported that the onset occurred approximately 48-72 hours before entering the hospital.
Past Medical History: She was affected by senile dementia and suffering from arterial hypertension and dyslipidemia. No other cardiovascular risk factors and no other previous cardiovascular events were known.
Differential diagnosis: Heart failure, myo/pericarditis.
Investigations: Initial cardiac assessment via ECG showed a significant supra-ST elevation from V1 to V6 of 3 mm. The echocardiography was early performed and showed a depressed systolic global function of the left ventricle (EF 35%), an apical pseudo-aneurism with hemorrhagic infarction and a large thrombus attached on the interventricular septum, compressing partially the right ventricle. Moreover a defect with shunt was detected at the middle portion of the interventricular septum.
The coronary angiography was performed without waiting for blood test results because of the ST elevation and symptoms complained by the patient. No antithrombotic pretreatment wasadministered.
Management (medical/interventions): The patient was transferred rapidly to the cath lab where a coronary angiography was performed and an occlusive stenosis of the proximal tract of the interventricular anterior artery were found. During the procedure, partial recanalization of the vessel was achieved by passing a coronary guidewire through the occlusive lesion and performing subsequently an angioplasty with a non-compliant balloon.
ANSWERS
ChatGPT
Default configuration
In this scenario, the final decision would be to proceed with the following steps:
Perform PCI with Stenting: Given the findings of significant occlusive stenosis in the proximal anterior interventricular artery and the complications of a thrombus and an apical pseudo-aneurysm, I would prioritize performing percutaneous coronary intervention (PCI) with the placement of a drug-eluting stent (DES) to ensure adequate revascularization and minimize the risk of future events.
Initiate Dual Antiplatelet Therapy: Following the PCI, I would start the patient on dual antiplatelet therapy (aspirin and a P2Y12 inhibitor) to prevent stent thrombosis.
Optimize Heart Failure Management: Given the low ejection fraction, I would initiate heart failure treatments, including:
ACE inhibitors or ARBs
Beta-blockers (once stable)
Diuretics to manage fluid overload.
Close Monitoring: The patient would be closely monitored in the ICU for hemodynamic stability, cardiac function, and signs of complications.
Multidisciplinary Follow-Up: I would ensure a follow-up plan involving cardiology, neurology for cognitive assessment, and possible rehabilitation services to address her comprehensive health needs.
Interrogation after upload of guidelines (ESC ACS 2023)
Initial Stabilization and Multidisciplinary Assessment:
Cardiac Intensive Care: Given the complexity of this presentation, the patient should be admitted to a cardiac intensive care unit (ICU) for continuous hemodynamic monitoring and close observation.
Heart Team Consultation: Involve a heart team, including interventional cardiologists, cardiac surgeons, and critical care specialists, given the patient’s high-risk features and the need for complex interventions.
Management of STEMI and Revascularization Strategy:
Percutaneous Coronary Intervention (PCI): Since partial recanalization was achieved with a non-compliant balloon, definitive revascularization should ideally be completed with a stent if feasible, to achieve optimal blood flow and limit further myocardial injury.
Antithrombotic Therapy: Given the thrombus presence, carefully administer anticoagulation therapy (e.g., low-molecular-weight heparin) post-PCI to manage thrombus risk. However, closely monitor for bleeding due to the hemorrhagic component within the pseudoaneurysm(acs 2023 ing).
Management of Mechanical Complications:
Left Ventricular Thrombus: Given the thrombus on the interventricular septum, consider anticoagulation therapy (such as heparin, followed by warfarin) to prevent embolic complications, but balance this against the bleeding risk. Adjust therapy based on ongoing imaging assessments and clinical stability.
Ventricular Septal Defect (VSD): Since the VSD is likely a result of ischemic injury, surgical repair may be necessary. Stabilization with medical management is possible in the short term, but surgical repair should be considered due to the hemodynamic compromise it introduces.
Pseudoaneurysm: This will require close monitoring with serial echocardiography or cardiac MRI to evaluate its stability. If the patient’s condition stabilizes, surgical repair can be considered, though high surgical risk should be factored into the decision-making process.
Secondary Prevention and Long-Term Care:
Antiplatelet Therapy: Dual antiplatelet therapy (DAPT) with aspirin and clopidogrel is recommended post-PCI for at least 12 months, as long as bleeding risk is manageable.
Lipid-Lowering Therapy: Initiate high-intensity statin therapy to achieve an LDL target of <55 mg/dL, given the patient’s acute coronary syndrome and dyslipidemia.
Heart Failure Management: Initiate heart failure medications, including beta-blockers, ACE inhibitors, and diuretics, titrated to tolerance, to support left ventricular function and manage symptoms.
Considerations for Age and Cognitive Status:
Tailor the treatment plan to balance aggressive management of her myocardial infarction with quality of life, given her dementia and advanced age. Involve her caregivers in discussions on the risks and benefits of further interventions to align with her and her family’s preferences.
Final Decision: Given the significant structural complications (thrombus, pseudoaneurysm, and VSD), an individualized approach balancing aggressive revascularization, anticoagulation, and potential surgical intervention is necessary. Surgical intervention may be required for definitive treatment of the VSD and pseudoaneurysm if the patient stabilizes and can tolerate surgery(acs 2023 ing).
Interrogation to ChatGPT browser
Final Decision and Summary
The immediate priority is stabilization with close monitoring and anticoagulation to prevent thromboembolism from the ventricular thrombus. Given the high surgical risk and complexity of her condition, surgical repair may need to be delayed if the patient stabilizes on medical therapy. However, if her hemodynamic status worsens, early surgical intervention may be inevitable, and a decision should be guided by her surgical evaluation and response to supportive measures.
Summary of Recommended Steps
Stabilize and monitor in the ICU with anticoagulation, cautious diuretics, and possible inotropes.
Engage a multidisciplinary team including cardiology, cardiothoracic surgery, and critical care to determine surgical versus percutaneous options.
Reassess surgical timing, aiming for delayed repair if possible, while managing with supportive therapy to optimize outcomes.
Proceed with surgery if her condition becomes unstable and intervention cannot be safely delayed.
Gemini
In this complex case, the primary goal is to stabilize the patient and limit myocardial damage. Given the delayed presentation, significant myocardial injury has likely already occurred.
Here's a final decision on the management strategy:
Immediate Management:
Continue Antithrombotic Therapy: Maintain the current antiplatelet and anticoagulant regimen to prevent further thrombotic events and promote vessel patency.
Close Monitoring: Closely monitor the patient's hemodynamic status, cardiac rhythm, and laboratory parameters.
Consider Additional Interventions:
Thrombectomy: Given the large thrombus burden and potential for improved reperfusion, a mechanical thrombectomy device could be considered, especially if there is persistent ischemia or ongoing myocardial injury.
Surgical Intervention: If the patient develops refractory heart failure, ventricular septal defect, or persistent ischemia despite optimal medical therapy, surgical intervention (e.g., coronary artery bypass grafting or ventricular septal defect repair) may be necessary.
PerplexityAI
The final decision emphasizes immediate PCI as a critical intervention for restoring coronary blood flow, coupled with comprehensive post-procedural management focused on heart failure treatment and cognitive support. This approach aims to optimize her recovery while considering her overall health status and quality of life.
MistralAI
The final decision involves stabilizing the patient's acute coronary syndrome with PCI, addressing the structural complications of the myocardial infarction (VSD, pseudo-aneurysm, and thrombus) with surgical consultation, and optimizing the patient's heart failure management and overall functional status with GDMT, cardiac rehabilitation, and regular follow-ups. The multidisciplinary team should work together to ensure the best possible outcome for the patient.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER ELEVEN: Emergency TAVI.
Premises:
A 74‐year‐old male patient was admitted to the hospital with progressive heart failure. He was diagnosed with severe aortic stenosis 3 years ago and has been suffering from exertional dyspnea and typical angina since that moment. Previous history of renal cell carcinoma with multiple several operations. On admission, transthoracic echocardiographic evaluation revealed severely impaired left ventricular systolic function (EF = 25 %, GLS = −4%), with inverse remodeling and low flow/low gradient severe aortic stenosis (AVmax = 3.2 m/sec, PeakPG = 41 mmHg, SVI = 23mL/m2. Coronary angiography was performed and did not reveal any stenosis, LV impairment and remodeling was attributed to the critical aortic stenosis, and TAVI was suggested as inevitable and urgent procedure. An elective procedure was planned but the patient's condition dramatically worsened, developing cardiogenic shock (BNP 3876 pg/mL), ischemic hepatitis (AST 5000 U/L, ALT 2900 U/L), acute renal failure (anuria), and severe lactic acidosis.
ANSWERS
ChatGPT
Default configuration
By prioritizing the urgent TAVI while providing comprehensive supportive care, we can optimize the chances of a favorable outcome in this critically ill patient.
Interrogation after upload of ESC guidelines (valvular illnesses)
Final Decision: Urgent TAVI with concurrent hemodynamic support, closely followed by post-procedural organ support. This approach offers the best balance of stabilization and definitive treatment for severe aortic stenosis, addressing the root cause of the patient’s cardiogenic shock and multisystem failure.
Interrogation to ChatGPT browser
In summary, emergent TAVI is indicated due to cardiogenic shock and severe AS with multi-organ dysfunction. Immediate hemodynamic stabilization using inotropes, vasopressors, and possibly MCS, combined with metabolic support (CRRT for renal failure, correction of acidosis), is essential. Following TAVI, the patient will require intensive post-procedure care in the ICU to optimize recovery.
Gemini
Given the patient's critical condition of cardiogenic shock secondary to severe aortic stenosis, immediate TAVI is the most appropriate course of action.
PerplexityAI
The urgency of the patient's condition necessitates swift action, prioritizing TAVI as a viable option to relieve severe aortic stenosis symptoms and improve overall prognosis.
MistralAI
The management of this critical scenario involves immediate stabilization and supportive care, followed by urgent TAVI to relieve the aortic stenosis and improve cardiac output. A multidisciplinary team approach is essential to coordinate care and optimize outcomes. The goal is to stabilize the patient's hemodynamic status, correct metabolic abnormalities, and proceed with TAVI as soon as possible to improve the patient's chances of survival and recovery.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER TWELVE: Decision-making on SAVR/TAVI and revascularization.
Premises:
Patient of 77 years old, suffering from diabetes type II, obesity, dyslipidaemia: Previous bilateral bilateral carotid thromboendarterectomy. Patient with exertional dyspnoea since 6 months and no chest pain. An elective coronary angiography was planned.
ECG: sinus rhythm with aspecific anomalies of repolarization
Echocardiography: augmented wall thickness, EF 50% with hypokinesia of distal lateral wall.
Blood test: PLT 200.000, creatinine 1,3 mg/dl
It was not still decided if defer the patient to surgical aortic valve replacement or TAVI implantation. An angio-TC of the chest and of lower limbs was performed, showing favourable vascular accesses and feasibility for eventual TAVI procedure. Coronary angiography showed critical stenosis of medium-distal tract of anterior interventricular artery. How would you manage this case? What would you do?
ANSWERS
ChatGPT
Default configuration
In summary, I would opt for TAVI first, followed by PCI for the critical coronary lesion. This approach balances the need for immediate relief of aortic stenosis symptoms while also addressing the coronary artery disease effectively.
Interrogation after upload of guidelines (ESC 2021 valvular heart disease) and supplementary data
Given the patient's characteristics and current guidelines, the most prudent approach would be to proceed with TAVI as the preferred method of aortic valve replacement due to the lower procedural risk. Simultaneously, perform PCI for the LAD stenosis, either before or during the TAVI, to address the coronary lesion and reduce the risk of future ischemic events.
In conclusion, the recommended management is TAVI with concurrent PCI for LAD stenosis, optimizing both valvular and coronary conditions while minimizing surgical risk.
Interrogation to ChatGPT browser
Final Recommendations
Proceed with PCI in the LAD prior to TAVI to alleviate any ischemic contribution to symptoms, optimize myocardial function, and reduce potential intra-procedural ischemia.
Perform TAVI after PCI as the primary intervention for severe AS, which is most likely contributing to the patient’s dyspnea and heart function issues.
Post-Intervention Management: Monitor the patient for bleeding risk and adjust antiplatelet therapy carefully, balancing the dual antiplatelet therapy needed post-PCI and the anticoagulation protocols post-TAVI.
Summary
For this 77-year-old patient with multiple comorbidities, the best course would be:
PCI for the mid-distal LAD stenosis to manage ischemia, ideally before TAVI.
TAVI as the valve intervention of choice based on favorable access and lower overall procedural risk compared to SAVR.
This strategy should optimize symptom relief and cardiovascular function while minimizing procedural risks, aligning with the patient's high surgical risk profile.
Gemini
I encourage you to discuss this case with a team of medical professionals to get their expert opinion.
PerplexityAI
Based on the comprehensive evaluation of the patient's clinical profile, comorbidities, and findings from diagnostic tests, the final decision would lean towards transcatheter aortic valve implantation (TAVI) with concurrent management of the critical coronary artery stenosis. Here’s the rationale for this decision.
MistralAI
In conclusion, my final decision would be to perform PCI first, followed by TAVI, with careful management of the patient's antithrombotic therapy and medical optimization of their comorbidities. This approach aims to minimize the patient's risk and improve their clinical outcome. However, it's crucial to emphasize that this decision should be made within the context of a multidisciplinary Heart Team and tailored to the patient's specific clinical situation
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER THIRTEEN: Atrial fibrillation in a patient with angiodysplasia of the colon.
Premises:
76-year-old patient with arterial hypertension and permanent atrial fibrillation. Overweight. In 2022 and 2024, previous hospitalizations for occult bleeding and anemia; therefore, in the last hospitalization, endoscopy with video capsule was performed which showed colon angiodysplasia. For anemia, de-escalation with anticoagulant was performed, going from Apixaban 5 mg 1 cp x 2 to Apixaban 2.5 mg 1 cp x 2, finally going to Clexane 6000 Ii 1 vial subcutaneously per day. In this way, a stability of hemoglobin values around 11 g/dl was achieved but the patient was substantially exposed to the risk of thrombosis and cardioembolic risk. Transesophageal echocardiogram: auricle free from thrombotic formations; left auricle measuring 34 mm x 22 mm. Percutaneous closure of the left atrial appendage was proposed.
How would you manage this scenario? What would you do?
ANSWERS
ChatGPT
Default configuration
In conclusion, I would proceed with the following final decision:
Schedule Percutaneous Closure of the Left Atrial Appendage (LAA): This procedure would help reduce the risk of stroke associated with atrial fibrillation, allowing for more flexibility in anticoagulation management.
Anticoagulation Management Post-Procedure:
After LAA closure, I would consider reinitiating a low-dose DOAC (such as Apixaban at 2.5 mg twice daily) if the patient's bleeding risk permits, or continue with low-dose Clexane for a limited duration until we establish stability.
Interrogation after upload of ESC guidelines (ESC 2024 atrial fibrillation)
In this complex case, my final decision would be to proceed with percutaneous left atrial appendage (LAA) closure. This approach aligns with the 2024 ESC guidelines for patients at high bleeding risk who cannot tolerate long-term anticoagulation. The LAA closure would aim to minimize the risk of thromboembolic events, especially stroke, without relying on anticoagulants that could exacerbate the patient's history of bleeding.
The steps would involve:
Scheduling the Percutaneous LAA Closure: This procedure would address the cardioembolic risk associated with AF while avoiding long-term anticoagulation that could increase bleeding risk.
Post-Procedure Monitoring: After LAA closure, I would recommend close follow-up to monitor hemoglobin levels, manage hypertension, and assess for any AF-related symptoms.
Reassessment of Comorbidities: Managing the patient's weight and hypertension would also be essential to support overall cardiovascular health.
This strategy provides a balanced approach by reducing stroke risk while prioritizing the patient's bleeding history and current stability on lower-intensity anticoagulation.
Interrogation to ChatGPT browser
Final Decision
Proceed with Left Atrial Appendage Closure:
LAA Closure Device (e.g., Watchman Device): Recommend percutaneous LAA closure to provide long-term protection against cardioembolic stroke while minimizing or potentially eliminating the need for long-term anticoagulation. This approach addresses the patient’s need for stroke prevention due to AF without ongoing risk of bleeding from anticoagulant therapy.
Short-Term Anticoagulation Post-Procedure:
Following the LAA closure, a short period of anticoagulation (typically 4–6 weeks) is generally recommended to allow endothelialization of the device. Given the patient’s bleeding history, this period should be carefully monitored, possibly using a lower-risk antiplatelet regimen if deemed safer by the managing team.
Long-Term Antithrombotic Strategy:
After the initial post-procedural anticoagulation period, transition to single antiplatelet therapy or potentially no antithrombotic therapy if the device successfully occludes the LAA and the patient’s bleeding risk remains high.
Ongoing gastroenterology follow-up for monitoring and managing angiodysplasia-related bleeding will be essential to prevent further bleeding episodes.
Summary
Primary Action: Proceed with percutaneous LAA closure to reduce the need for anticoagulation in the context of recurrent GI bleeding.
Secondary Action: Use short-term anticoagulation post-procedure, followed by a simplified long-term antithrombotic plan tailored to balance bleeding and thrombotic risks.
This approach minimizes stroke risk in AF while addressing the patient’s bleeding vulnerability, offering a balanced and sustainable long-term management strategy.
Gemini
Given the complex interplay of risks and benefits in this case, the final decision on management should be made in collaboration with the patient and a multidisciplinary team of healthcare professionals. However, based on the information provided, I would lean towards recommending percutaneous closure of the left atrial appendage (LAA) as a potential strategy to reduce the patient's thromboembolic risk while allowing for a significant reduction in anticoagulation therapy.
PerplexityAI
The final decision is to proceed with left atrial appendage closure followed by endoscopic treatment of angiodysplasia, with careful monitoring and adjustment of anticoagulation therapy thereafter. This approach aims to balance the prevention of thromboembolic events while effectively managing gastrointestinal bleeding, ultimately improving the patient's quality of life and clinical outcomes.
MistralAI
in conclusion, the final decision is to proceed with LAAC to reduce the risk of thromboembolism, optimize peri-procedural and post-procedural antithrombotic therapy with multidisciplinary input, and manage the colonic angiodysplasia with regular monitoring and follow-up. This approach aims to balance the risks of thromboembolism and bleeding while considering the patient's individual needs and preferences.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER FOURTEEN: A case of mitral and aortic regurgitation in a patient in frail status.
Premises:
78-year-old patient, suffering from dyspnoea on slight exertion, arterial hypertension and paroxysmal atrial fibrillation. Poor general conditions. He was affected by dilatation of the aortic root (48 mm) and ascending aorta (46 mm) with moderate aortic insufficiency and severe mitral insufficiency. Previous STEMI treated with PCI + 3 DES on CDx in 2008; revascularization with PTCA + DES on distal CDx in September 2021. Medical therapy for heart failure and valvular insufficiency was on top with the use of loop diuretics and spare potassium diuretics. Since some months patient declined progressively in his being autonomous.
Echocardiography: EF of 45%, global hypokinesia with dilated left ventricle (57 mm), flail of A2 and P2 of mitral valve.
How would you manage this scenario? What would you do?
Medical theraphy was already on top. what would you do in the end? take a final decision
ANSWERS
ChatGPT
Default configuration
Final Decision:
Percutaneous MitraClip for severe functional mitral regurgitation to improve symptoms and quality of life without the high risk of open-heart surgery.
Close monitoring of aortic insufficiency and root dilation, with serial imaging.
Palliative care referral to address symptom control, quality of life, and future decisions regarding the patient's goals of care.
Continue optimizing medical therapy for heart failure, including diuretics, beta-blockers, ACE inhibitors/ARNI, and SGLT-2 inhibitors.
Regular follow-up with multidisciplinary care, including cardiology, heart failure specialists, and palliative care.
In summary, the primary goal is to improve symptoms and quality of life while managing the patient’s advanced heart failure and valvular disease. The high surgical risks argue against aggressive surgical interventions, so a percutaneous approach with MitraClip for the mitral regurgitation and careful monitoring of the aortic regurgitation and root dilation is the most appropriate course of action. Palliative care should also be integrated to manage symptoms and prepare for potential future decisions.
Interrogation after upload of guidelines (ESC valvular heart disease 2021) and supplementary data
Considering all factors, if the patient remains symptomatic with severe mitral and moderate aortic regurgitation, a transcatheter intervention could be a reasonable approach, focusing on mitral valve repair first if feasible. Here’s how this could be approached:
Mitral Valve Repair (TEER):
Perform a transcatheter edge-to-edge repair (TEER), such as a MitraClip, to address severe mitral regurgitation if the anatomy is suitable. TEER is less invasive than surgery and could improve symptoms with lower perioperative risk in frail patients.
If the mitral anatomy does not allow for TEER, a palliative approach may be more appropriate given the limited expected benefits from high-risk surgery.
Monitoring Aortic Regurgitation:
Reassess the aortic valve following mitral intervention. Moderate aortic regurgitation may become better tolerated if mitral regurgitation is reduced, potentially delaying or avoiding aortic intervention.
If symptoms persist due to aortic regurgitation and the patient’s functional status allows, a second step with TAVI might be considered later.
Palliative Approach if Interventions Are Unfeasible:
If TEER is not possible or if the Heart Team assesses that even transcatheter interventions carry high futility risks, the focus should shift entirely to comfort measures, optimizing quality of life, and symptom control.
This decision should be made in close consultation with the patient and family, explaining both potential benefits and limitations of each approach.
Interrogation to ChatGPT browser
In the end, given the patient's frail condition, severe mitral regurgitation, and moderate aortic insufficiency, I would proceed with the following final decision:
Final Decision
Primary Intervention:
Transcatheter Mitral Valve Repair (MitraClip): Arrange for the MitraClip procedure to address the severe mitral regurgitation. This approach is minimally invasive and offers a chance to relieve symptoms and improve quality of life without the need for open-heart surgery, which would be high-risk given the patient’s frailty and comorbidities.
Secondary Management:
Conservative Management of Aortic Regurgitation: Continue with medical therapy for the moderate aortic regurgitation, as it does not yet warrant a separate intervention. Managing volume status and controlling blood pressure will help minimize the impact of AR on symptoms.
Optimize Heart Failure Medications: Ensure the patient is on guideline-directed medical therapy (GDMT) for heart failure, including diuretics to control volume overload and symptoms of dyspnea.
Supportive and Palliative Considerations:
If MitraClip is not successful or the patient’s condition continues to decline, consider a palliative approach focused on maximizing comfort and quality of life, possibly involving home-based palliative care services.
This plan emphasizes a minimally invasive option to improve the patient's quality of life with the least procedural risk, while ensuring supportive care if intervention is limited by the patient’s condition.
Gemini
Potential Management Strategies:
Conservative Management: If the patient is stable on medical therapy and their symptoms are well-controlled, a conservative approach with close monitoring might be the most appropriate option.
Minimally Invasive Procedures: If the patient is not a good candidate for open-heart surgery, minimally invasive procedures like transcatheter aortic valve replacement (TAVR) or transcatheter mitral valve repair (TMVR) could be considered, depending on the specific valve disease and the patient's anatomy.
Palliative Care: If the patient is very frail and has limited life expectancy, palliative care should be considered to focus on symptom management and improving quality of life.
Final Decision:
The final decision on the best course of action should be made in collaboration with the patient, their family, and a multidisciplinary team of healthcare professionals, including cardiologists, cardiac surgeons, and palliative care specialists. The decision should be individualized and based on a careful assessment of the patient's specific needs and preferences.
PerplexityAI
Final Decision: Surgical Intervention
Given the patient's severe mitral insufficiency, moderate aortic insufficiency, and declining functional status despite optimized medical therapy, surgical intervention is warranted. The following steps outline the rationale and approach for proceeding with surgery:
Multidisciplinary Team Evaluation: Ensure that a comprehensive assessment by a multidisciplinary heart team (MDT) is conducted to evaluate the patient's overall health, functional capacity, and potential surgical risks. This team should include cardiologists, cardiac surgeons, geriatricians, and anesthesiologists to provide a holistic view of the patient's condition.
Surgical Options:
Mitral Valve Repair or Replacement: Given the presence of severe mitral regurgitation and left ventricular dysfunction (EF of 45%), surgical intervention is indicated. Repair is preferred when feasible due to lower morbidity compared to replacement. The specific technique (e.g., valve repair vs. replacement) should be tailored based on the anatomical findings during surgery.
Aortic Valve Intervention: If significant aortic regurgitation contributes to symptoms, consider performing aortic valve replacement concurrently with mitral valve surgery. This dual approach may improve overall outcomes by addressing both valvular issues simultaneously
Consideration of Transcatheter Approaches: If the patient is deemed high-risk for open-heart surgery due to frailty or comorbidities, transcatheter options such as MitraClip for mitral regurgitation or transcatheter aortic valve replacement (TAVR) should be considered. These less invasive techniques can provide symptomatic relief with lower associated risks.
Postoperative Care: Following surgery, close monitoring in an intensive care setting will be essential due to the patient's frail status. A structured rehabilitation program should be implemented to support recovery and improve functional outcomes.
Palliative Considerations: If surgical intervention is not feasible due to extreme frailty or if the patient declines surgery, focus on palliative care measures to improve quality of life and manage symptoms effectively.
In conclusion, given the severity of the patient's valvular disease and current symptoms, surgical intervention is recommended as the most appropriate course of action, with careful consideration of the patient's overall health status and potential benefits versus risks involved in surgery.
MistralAI
Final Decision: Considering the patient's frail status, advanced age, and comorbidities, the most compassionate and reasonable approach may be to pursue a minimally invasive, transcatheter intervention, if anatomically feasible. This could involve:
MitraClip (TEER) for the severe mitral regurgitation due to flail A2 and P2 segments.
TAVR for the moderate aortic regurgitation, although this depends on the specific anatomy and mechanism of regurgitation.
However, if transcatheter interventions are not feasible or unlikely to provide significant benefit, the final decision should be to focus on optimizing palliative and medical management, with an emphasis on symptom control and maintaining the best possible quality of life.
This final decision should be made in consultation with the heart team, the patient, and the patient's family, ensuring that everyone understands the risks, benefits, and alternatives, and that the chosen path respects the patient's preferences and values. Regular follow-up and re-evaluation should be maintained, as the patient's clinical status may change over time.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER FIFTEEN: Complications during the prothesis delivery, a peculiar TAVR case.
Premises:
78-years old patient, in anamnesis: obesity, smoker, Hypertension. Symptomatic for shortness of breath and chest pain occurred while climbing the stairs. After several ambulatorial evaluations, due to persistance and worsening of symptoms, gets to the emergency room and was conducted to the cardiology department.
Echocardiogram: Hypertrophy of left ventricle with normal ejection fraction (FE: 55%), Widely calcification of aortic cusps and severe aortic stenosis (PGmed: 60 mmHG; vmax: 6 m/sec; iAVA: 0.4 mmq/mq). Mild mitral regurgitation. Normal ejection fracion of the right ventricle.
The CT-study showed normal diameters and viability of illiac-femoral axes and severe and widely calcification of the coronary cusps. Thus the strategy was to previously dilatate the valve, performing a valvuloplasty and then to deploy the new valve (an self-expandable , supranular protesis).
ECG: Left Ventricular Hypertrophy and aspecific abnormalities of the ventricular depolarization.
In the cath lab, valvuloplasty was performed, and the protesis was prepared in order to be properly deployed. However the blood pressure started to drop, and in brief time the patient was in shock. Echocardiography showed severe aortic regurgitation, likely due to the valve predilatation; so the prostetic valve had to be quickly positioned. However an other big issue occurred, the prothesis showed unfolding and for this reason had to be prepared properly again.
ANSWERS
ChatGPT
Default configuration
In the end, after stabilizing the patient’s hemodynamics and reassessing the situation with echocardiography, I would proceed with the following final decision:
Immediate Deployment of the Prosthesis: If the prosthesis can be effectively repositioned and deployed without significant delay, I would prioritize this to address the severe aortic regurgitation and stabilize the patient.
If Re-deployment Fails: If repositioning the prosthesis is unsuccessful or if the patient's condition worsens, I would immediately activate the cardiac surgery team. Preparing for surgical intervention would be critical to manage the aortic regurgitation effectively and prevent further hemodynamic collapse.
Continuous Monitoring: Regardless of the outcome, I would ensure the patient is continuously monitored for any changes in vital signs and hemodynamic status while preparing for either option.
This decision emphasizes rapid intervention to mitigate severe complications and preserve patient stability, recognizing the urgency of the clinical scenario.
Interrogation after upload of ESC guidelines(ESC valvular heart disease 2021) and supplementary data
To manage this complex TAVR case involving hypotension, shock, and unfolding of the prosthetic valve after initial valvuloplasty and valve preparation, consider the following multi-step approach:
Stabilize Hemodynamics: Initiate rapid fluid resuscitation and administer vasopressors if needed to support blood pressure and stabilize the patient’s hemodynamics.
Quick Valve Deployment: Since severe aortic regurgitation (AR) has occurred following the valvuloplasty, immediate and proper deployment of the prosthetic valve is critical. This may reduce the volume of regurgitation, thereby improving hemodynamic stability.
Reposition and Prepare Prosthesis: Given that the prosthetic valve unfolded, it’s essential to reposition and stabilize the device before redeployment. Ensure all necessary tools and technical support are available to address further unfolding risks.
Use of Additional Imaging: Utilize transesophageal echocardiography (TEE) or intravascular ultrasound to guide precise positioning and deployment, especially if the anatomy is challenging due to calcification or the device itself.
Consider Mechanical Circulatory Support: If the patient remains unstable despite these measures, you may consider a temporary mechanical circulatory support (MCS) device, such as an intra-aortic balloon pump (IABP) or an Impella, to support cardiac output during valve manipulation.
Post-Procedural Monitoring and Management: After the valve is successfully deployed and hemodynamics are stabilized, closely monitor for signs of any residual AR or perivalvular leaks and manage complications such as vascular access site bleeding or thromboembolism, as guided by post-TAVR protocols
Interrogation to ChatGPT browser
Immediate Management in the Cath Lab
Stabilize Hemodynamics:
Initiate Inotropic and Vasopressor Support: Administer inotropes (e.g., dobutamine) and vasopressors (e.g., norepinephrine) to support cardiac output and maintain blood pressure while the prosthesis is repositioned.
Rapid Volume Resuscitation: Volume loading may be needed if there is significant hypotension, but this should be balanced against the risk of exacerbating acute heart failure.
Deploy the Prosthetic Valve:
Immediate Prosthesis Positioning: Given the severe AR after predilatation, it’s essential to secure the prosthesis quickly. The unfolding issue with the prosthesis likely requires swift correction and repositioning.
Reprepare and Redeploy the Valve: Since the prosthesis showed unfolding, it must be re-prepared carefully to ensure that it deploys correctly. Ensuring proper alignment and readiness of the device is critical before the next attempt.
Echocardiographic Guidance:
Continuous Echocardiographic Monitoring: Use transesophageal echocardiography (TEE) to guide precise positioning of the prosthetic valve and assess for immediate improvement in aortic valve function after deployment.
Monitor for Complications: Watch for signs of paravalvular leak or incomplete valve expansion, which could necessitate repositioning or balloon post-dilatation to ensure effective sealing.
Post-Deployment Management
Assess Prosthetic Valve Function and Hemodynamics:
Perform TEE or transthoracic echocardiography (TTE) immediately after deployment to confirm proper positioning, adequate reduction of aortic regurgitation, and appropriate hemodynamic improvement.
Ensure there are no signs of paravalvular leak, migration, or under-expansion that could lead to continued hemodynamic instability.
Monitor for Other Immediate Complications:
Vascular Access Site Management: Assess femoral access sites for bleeding or hematoma, given that the patient may have received vasopressor support.
Rhythm Monitoring: The patient may be at risk for arrhythmias following valve deployment, so continuous ECG monitoring is essential.
Hemodynamic Support Tapering:
Gradually reduce inotropic and vasopressor support once the valve is confirmed to be functioning properly and the blood pressure stabilizes.
Closely monitor for signs of volume overload or worsening mitral regurgitation, especially in a patient with left ventricular hypertrophy.
Final Decision
Immediate Priority: Reprepare and reposition the prosthetic valve to promptly relieve severe aortic regurgitation and restore hemodynamic stability.
Secondary Priority: After successful deployment, continue hemodynamic monitoring, support, and echocardiographic assessment to detect any further complications or valve-related issues.
Summary:This case highlights the importance of quick, decisive action during TAVR when complications arise. Stabilizing the patient and swiftly re-preparing and deploying the prosthesis will help address the acute AR and prevent further hemodynamic deterioration.
Gemini
Final Decision: Aggressive Management of Acute Aortic Regurgitation Given the patient's critical condition with acute severe aortic regurgitation following TAVR, immediate and aggressive management is essential. Key Strategies:
Hemodynamic Stabilization:
Inotropic Support: Administer inotropic agents like dobutamine or norepinephrine to improve myocardial contractility and maintain blood pressure.
Vasodilators: Use vasodilators judiciously to reduce afterload, but avoid excessive hypotension.
Intra-aortic Balloon Pump (IABP): Consider IABP to augment cardiac output and reduce afterload.
Re-intervention:
Valve Repositioning: If feasible, attempt to reposition the valve to improve its function and reduce regurgitation.
Additional Stent Frame Deployment: In some cases, deploying an additional stent frame may help stabilize the valve and reduce regurgitation.
Surgical Intervention:
Emergency Aortic Valve Replacement: If re-intervention fails to stabilize the patient, consider emergency surgical aortic valve replacement.
Intensive Monitoring and Support:
Continuous Hemodynamic Monitoring: Closely monitor blood pressure, heart rate, and cardiac output.
Echocardiographic Monitoring: Perform frequent echocardiograms to assess valve function and left ventricular performance.
Renal Function Monitoring: Assess renal function and consider renal replacement therapy if needed.
Infection Prevention: Implement strict infection control measures.
By following these strategies and closely monitoring the patient's condition, we can improve the patient's chances of survival and recovery.
PerplexityAI
Here’s how I would summarize the approach: Final Decision: Immediate Deployment of the Prosthesis
Rapid Deployment:
Immediate Action: Given the severe aortic regurgitation and hemodynamic instability, I would prioritize the rapid deployment of the prosthesis. This is critical to restore hemodynamic stability and prevent further deterioration.
Re-crimping and Re-preparation: If the prosthesis is unfolding, I would ensure it is properly re-crimped and re-prepared for deployment. This may involve careful handling to avoid further complications.
Use of Balloon Valvuloplasty as Needed:
If the prosthesis cannot be deployed successfully due to unfolding or other issues, I would consider performing a balloon valvuloplasty again to temporarily alleviate severe regurgitation until the prosthesis can be positioned correctly.
Alternative Access Consideration:
If deployment continues to be problematic, I would evaluate the feasibility of switching to an alternative access route (like transapical) if available and appropriate for this patient.
Post-Deployment Monitoring:
After successful deployment, I would closely monitor the patient for hemodynamic stability, potential paravalvular leaks, and conduction abnormalities.
Initiate appropriate post-procedural care, including anticoagulation and multidisciplinary team involvement.
MistralAI
Final Decision:
Immediate Hemodynamic Support:
Start vasopressors (e.g., norepinephrine, phenylephrine) to support blood pressure.
Consider adding inotropes (e.g., dobutamine) to improve cardiac output if needed.
Administer IV fluids cautiously to support blood pressure without causing volume overload.
Rapid Pacing:
Initiate rapid pacing to temporarily reduce cardiac output and facilitate the deployment of the prosthetic valve.
Echocardiographic Guidance:
Use transesophageal echocardiography (TEE) or intracardiac echocardiography (ICE) to guide the procedure and assess the severity of aortic regurgitation and the positioning of the prosthetic valve.
Reposition and Redeploy the Valve:
Retrieve the Partially Deployed Valve: Attempt to retrieve the valve using a snare or other retrieval device if it is not fully deployed and is causing hemodynamic compromise.
Prepare the Valve Again: Ensure the valve is properly crimped and positioned on the delivery system.
Optimize Valve Positioning:
Reassess Annulus Size: Confirm the correct size of the prosthetic valve based on the annulus measurements.
Reposition the Valve: Use fluoroscopic and echocardiographic guidance to optimize the positioning of the valve before deployment.
Deploy the Valve:
Rapid Pacing: Use rapid pacing to minimize cardiac output during valve deployment.
Deploy the Valve: Carefully deploy the valve, ensuring it is fully expanded and properly seated.
Management of Complications:
Severe Aortic Regurgitation: If severe aortic regurgitation persists after valve deployment, consider performing balloon aortic valvuloplasty (BAV) to reduce the regurgitation and stabilize the patient. If necessary, implant a second valve (valve-in-valve procedure) to achieve a better seal and reduce regurgitation.
Valve Migration or Malposition: If the valve migrates or is malpositioned, use a snare to reposition it or retrieve it if necessary. If repositioning is not feasible, consider implanting a second valve to stabilize the first one and achieve a proper seal.
The management of this complex TAVR case involves immediate hemodynamic support, rapid pacing, and echocardiographic guidance to facilitate the successful deployment of the prosthetic valve. If complications such as severe aortic regurgitation or valve migration occur, prompt intervention with BAV, valve repositioning, or second valve implantation is necessary. Close post-procedure monitoring and follow-up are essential to ensure the best possible outcome for the patient.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER SIXTEEN: TAVR in elderlies; a complex case in a scenario of multiple comorbidities.
Premises:
85 years old female patient, heavy smoker, suffering from diabetes and arterial hypertension. In anamnesis multiple hospitalization due to cardiovascular issues (Acute Coronary Syndrome 7 years ago, 2 DES on interventricular anterior artery); bifemoral and carotid stenting deployed 5 and 8 years ago respectively; stroke 8 years ago with no significant consequences. No specific follow up during the years because of poor patient compliance.
The patient accessed to the hospital complaining about asthenia, shortness of breath, dizziness at rest and dyspnoea when laying down during sleeping.
ECG: Sinus rhythm, left ventricular hypertrophy, Q in anterior leads.
Blood analysis: HB: 10 g/dL, creatinine 1.8 mg/dL (eGFR 35 ml/min), no significant troponine alterations.
ECD was performed: Concentric LVH; EF: 50%, ipokinesia of the antero-lateral wall, Severe aortic stenosis (PG med: 45mmHG; vmax: 4,6 m/sec, iAVA: 0,55 mmq/mq). Mild to moderate mitral regurgitation, sPAP: 45 mmHG).
The patient was conducted to the cardiology department in order to choose the better therapeutic strategy.
An angioCT was performed, showing significant aortic calcification and partial cusps fusion.
Moreover, the evaluation of the iliac-femoral axes was even more crucial due to severe calcifications and myointimal proliferation from the previous stenting. This led to a significant reduction in vessel diameter, rendering the transfemoral approach unfeasible. The patient was highly symptomatic.
ANSWERS
ChatGPT
Default configuration
In this case a trans axillar approach was chosen; So the valve was delivered using a tranaxillar access (the equipe was composed both of cardiologists and cardiosurgeons) and the temporary pacemaker was positioned using a giugular access. The procedure was effective and the patient was discharged after five days of observation, asymptomatic. Given the complexity of the case and the significant comorbidities of the patient, I would recommend proceeding with a transapical TAVR if a transfemoral approach is not feasible due to severe iliac-femoral calcifications.
Interrogation after upload of ESC guidelines and supplementary data
Final Decision: Proceed with TAVR using an alternative access route, given the high risk of SAVR and the patient’s severe symptomatic profile. Ensure vigilant peri-procedural monitoring and a tailored post-TAVR care plan to manage frailty and comorbidities effectively
Interrogation to ChatGPT browser
Given her severe aortic stenosis and contraindications to transfemoral access, alternative approaches such as transcaval or transapical TAVR seem most appropriate, with comprehensive pre-procedural optimization. Close monitoring, both peri- and post-operatively, and involvement of the heart team are key to managing this high-risk patient with complex comorbidities.
Gemini
TAVR (Transcatheter Aortic Valve Replacement):
Given the patient's severe aortic stenosis symptoms and limited surgical options, TAVR appears to be the most appropriate treatment.
However, the significant vascular disease and calcifications make the transfemoral approach challenging.
Alternative access routes (transapical, transcarotid, transaortic) should be considered, but they also have their own risks and limitations.
PerplexityAI
Given the comprehensive evaluation of the patient's condition, including her severe symptomatic aortic stenosis, multiple comorbidities, and the anatomical challenges for transfemoral access, the final decision would be to proceed with Transcatheter Aortic Valve Replacement (TAVR) using an alternative access route.
MistralAI
Proceeding with transapical TAVR is the most appropriate course of action given the patient's complex medical history and the anatomical challenges presented by the iliac-femoral calcifications. This decision is supported by a multidisciplinary approach and careful planning to ensure the best possible outcome for the patient.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER SEVENTEEN: cardiogenic shock secondary to severe mitral regurgitation.
Premises:
A 78-year-old male with a history of diabetes, atrial fibrillation and hypertension accessed emergency room with acute shortness of breath and arterial hypotension that led to in-hospital cardiac arrest. Immediately after resuscitation, the patient required mechanical circulatory support and endovenous inotropes.
ECG: sinus tachycardia with non-specific anomalies of ventricular repolarization.
The patient was stabilized and subsequently TEE was performed, revealing torrential mitral regurgitation secondary to P2 flail with an 11mm flail gap. Systolic flow reversal in pulmonary veins along with severely reduced EF were noted. Due to the comorbidities the patient was considered at high risk for a surgical repair.
ANSWERS
ChatGPT
Default configuration
Given the high-risk nature of the patient and the severe mitral regurgitation causing cardiogenic shock, the final decision would be to pursue a minimally invasive approach, specifically a Mitral valve clip (MitraClip) procedure. This option balances the need to address the torrential mitral regurgitation effectively while minimizing the surgical risk associated with a more invasive operation.
Interrogation after upload of guidelines (ESC 2021 valvular heart diseases) and supplementary data
In managing this critical scenario of cardiogenic shock due to severe mitral regurgitation (MR) secondary to P2 flail, especially in a high-risk 78-year-old patient with multiple comorbidities, the ESC/EACTS guidelines provide a structured approach:
Stabilization and Immediate Support:
The immediate use of mechanical circulatory support (MCS), as was done, is crucial in stabilizing hemodynamics for patients in cardiogenic shock secondary to severe MR. Inotropes are typically used as a bridge to a definitive intervention, given the reduced ejection fraction and torrential MR observed(valvulopatie eng).
Surgical vs. Transcatheter Intervention:
Although surgical mitral valve repair is generally preferred for acute severe MR, the high surgical risk in this patient due to advanced age, diabetes, atrial fibrillation, and hemodynamic instability makes transcatheter edge-to-edge repair (TEER) (such as MitraClip) an attractive option. TEER is increasingly recommended for patients who are poor surgical candidates due to comorbidities, and it has shown benefits in reducing mitral regurgitation severity, potentially stabilizing patients who cannot tolerate surgery(valvulopatie eng).
Heart Team Evaluation:
A Heart Team assessment is essential to weigh the risk-benefit ratio of TEER versus conservative management, considering this patient’s overall condition. The team may consider TEER if a quick, minimally invasive intervention is feasible and likely to improve clinical stability and quality of life, particularly since the patient presents systolic flow reversal in pulmonary veins, indicating significant hemodynamic impact from MR(valvulopatie eng).
Monitoring and Serial Testing:
Following intervention, close monitoring of hemodynamic parameters, pulmonary pressures, and left ventricular function is crucial. If TEER or any intervention is successful, serial echocardiographic follow-up is essential to assess the mitral valve function and potential improvement in left ventricular function(valvulopatie eng).
Supportive Care and Management of Comorbidities:
Optimal management of diabetes, atrial fibrillation, and blood pressure is essential post-intervention to reduce the cardiac workload and prevent further complications. Given the patient’s atrial fibrillation and high thromboembolic risk, appropriate anticoagulation should also be maintained.
In summary, TEER appears to be the most suitable intervention in this patient, balancing the need to urgently address the severe MR while minimizing surgical risk.
Interrogation to ChatGPT browser
In managing this 78-year-old male with severe mitral regurgitation (MR) due to a P2 flail leaflet and significant comorbidities, the optimal approach would be to proceed with transcatheter edge-to-edge repair (TEER) using the MitraClip device. This minimally invasive procedure is particularly suitable for high-risk patients who are not ideal candidates for open-heart surgery. TEER has
demonstrated efficacy in reducing MR severity and improving clinical outcomes in similar patient
populations. (Oxford Academic)
Prior to the procedure, a comprehensive evaluation by a multidisciplinary Heart Team is essential
to confirm anatomical suitability and to optimize peri-procedural management. This collaborative
approach ensures that all aspects of the patient’s condition are considered, leading to a tailored
and effective treatment plan.
Gemini
Final Decision: Urgent Transcatheter Mitral Valve Repair (TMVR)
Given the patient's critical condition with severe mitral regurgitation and cardiogenic shock, immediate TMVR is the most appropriate course of action.
PerplexityAI
In this scenario, considering the patient's high surgical risk due to age and comorbidities, the final decision would be to proceed with Transcatheter Edge-to-Edge Repair (TEER) using the MitraClip. This approach offers a minimally invasive option to address the torrential mitral regurgitation effectively while avoiding the risks associated with open-heart surgery.
MistralAI
Proceed with urgent percutaneous mitral valve repair using the MitraClip device, given the patient's high surgical risk and the need for immediate intervention to address the severe mitral regurgitation (MR) and cardiogenic shock.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER EIGHTEEN: Transcatheter treatment of multiple pathologies: a paradigmatic clinical case.
Premises:
84-year-old man, smoker, suffering from arterial hypertension, dyslipidaemia, bilateral significant carotid stenosis, chronic renal failure (stage IIIB), history of prostatic cancer treated with surgery, radiotherapy and chemotherapy. In medical history, previous hospitalization for multiple small spontaneous cerebral hemorrhages. For several months onset of worsening angina and dyspnea on exertion. At the cardiological evaluation, moderate-severe mitral insufficiency was found. The referring cardiologist had opted for an initially conservative strategy and recommended maximal medical therapy.
The patient came to our attention for a syncopal episode during an episode of atrial fibrillation (AF) with high ventricular response rate, without signs of acute myocardial ischemia in progress or previous necrosis on the ECG.
Blood tests: normal blood count, creatinine 1.90 mg/dl, high sensitivity troponin curve indicative of myocardial damage (134-207 ng/l).
Subsequent spontaneous restoration of sinus rhythm during clinical observation.
Echocardiography: severe mitral insufficiency due to flail of the posterior leaflet with rupture of the chordae tendineae. The left ventricle was enlarged (end-diastolic diameter 68 mm, end-systolic diameter 44 ml, end-diastolic volume 155 ml, end-systolic volume 74 ml). Hypokinesia of the mid tract of the inferior wall with preserved ejection fraction (60%). Estimated systolic pulmonary artery pressure 43 mmHg. A transesophageal echocardiogram was performed and confirmed severe mitral insufficiency with flail of the P2 segment towards P3 and rupture of at least two first-order chordae tendineae, non-dilated mitral valve ring.
The patient underwent coronary angiography after prophylaxis for allergy to iodinated contrast medium. Severe three-vessel coronary artery disease was found. The case was submitted to collegial discussion in the Heart Team and, in consideration of the multiple comorbidities and the angiographic picture, a possible cardiac surgery strategy for correction of the valvulopathy and myocardial revascularization was excluded. The mitral valve anatomy was reassessed and it was found suitable for a possible percutaneous plastic procedure with the Mitra Clip system. At the same time, based on the coronary anatomy, multivessel coronary revascularization with coronary angioplasty (PCI) was indicated. In light of the need to continue anticoagulant therapy (CHA2DS2-VASc = 4) and possible dual antiplatelet therapy (DAPT) in case of PCI with stent implantation, the patient underwent neurological evaluation. In view of the high risk of bleeding (HAS-BLED = 4) and the positive history of spontaneous cerebral hemorrhage, the following considerations were made: a) the risk of bleeding from triple antithrombotic therapy (anticoagulant plus DAPT) would have been excessive; b) dual antithrombotic therapy (anticoagulant plus single antiplatelet), in addition to exposing the patient to a very high risk of bleeding, would have presented a dubious protective coverage against stent thrombosis due to the high anatomical complexity of the PCI procedure and the number of stents that may be necessary; c) treatment with simple DAPT would not have offered sufficient protection against cardioembolic stroke.
How would you manage this scenario? What would you do?
ANSWERS
ChatGPT
Default configuration
Given the complexities of this patient's case, the final decision would be as follows:
Proceed with the MitraClip Procedure: This is the priority to address the severe mitral insufficiency and improve the patient's symptoms, which is critical given his worsening angina and dyspnea.
Post-MitraClip Management:
After successfully placing the MitraClip, initiate anticoagulation therapy with a direct oral anticoagulant, considering the patient's renal function.
Single antiplatelet therapy (e.g., clopidogrel) would be started to minimize bleeding risk while providing adequate protection against thromboembolic events.
Coronary Revascularization (PCI): If the patient remains stable and there are no complications from the MitraClip procedure, proceed with PCI for multivessel coronary artery disease, using a careful approach to minimize the risk of bleeding and considering the complexity of the intervention.
Close Monitoring: Ensure rigorous monitoring for any complications post-procedure and adjust anticoagulant therapy as needed based on the patient's renal function and clinical status.
Regular Follow-Up: Schedule follow-up appointments to monitor the patient's heart function, manage medications, and reassess risks.
In conclusion, the best course of action is to proceed with the MitraClip placement first, followed by careful planning for PCI while managing anticoagulation and monitoring closely for any adverse events.
Interrogation after upload of ESC guidelines (ESC valvular heart diseases 2021 and supplementary data, ESC 2023 CCS, ESC 2024 atrial fibrillation)
Given the patient's high bleeding risk (HAS-BLED = 4), prior history of cerebral hemorrhage, severe multivessel coronary disease, and symptomatic mitral valve pathology, a balanced approach prioritizing safety and efficacy is essential. Here’s a step-by-step management strategy:
Percutaneous Mitral Valve Repair with MitraClip: Since the patient is symptomatic with severe mitral regurgitation, proceed with the MitraClip procedure, as it’s feasible given the mitral valve anatomy. This intervention should improve symptoms and reduce volume overload.
Coronary Revascularization Strategy: Given severe three-vessel coronary artery disease, perform PCI selectively in high-risk lesions using the minimum necessary stents to reduce the requirement for prolonged dual antiplatelet therapy (DAPT).
Antithrombotic Management:
Left Atrial Appendage Occlusion (LAAO): Given the need for anticoagulation and the elevated bleeding risk, consider LAAO to manage the cardioembolic stroke risk due to atrial fibrillation (AF).
Post-PCI and Post-MitraClip Antithrombotic Therapy: Opt for dual antithrombotic therapy (DOAC plus a single antiplatelet agent) if LAAO is performed. If LAAO is not feasible, carefully balance DAPT duration to minimize bleeding risk while providing adequate protection against stent thrombosis(atrial fibrillation).
Frequent Monitoring and Follow-Up: Closely monitor renal function, bleeding signs, and cardiac status to promptly address any emerging complications, especially given the complex clinical background.
This approach aims to optimize symptom management and reduce both thromboembolic and bleeding risks in this high-risk patient.
Interrogation to ChatGPT browser
Given these factors, I would proceed with a staged, minimally invasive approach:
Percutaneous Mitral Valve Repair with MitraClip:
First, perform the MitraClip procedure to reduce mitral regurgitation. This is crucial to address the patient's worsening symptoms, prevent further left ventricular remodeling, and minimize the risk of future heart failure exacerbations.
MitraClip is appropriate here because it avoids the risk of open-heart surgery, which is contraindicated due to the patient's comorbidities.
Coronary Revascularization Strategy:
Percutaneous Coronary Intervention (PCI) is indicated, but considering the bleeding risks, a careful approach to minimize stent use and potentially avoid drug-eluting stents (DES) in favor of bare-metal stents (BMS) or drug-coated balloons, if feasible, should be discussed.
If PCI is necessary, using the least complex stenting approach with the fewest number of stents may reduce the need for prolonged dual antiplatelet therapy (DAPT).
Antithrombotic Strategy:
After PCI, considering the patient's bleeding risk and cerebral hemorrhage history, dual antithrombotic therapy (a single antiplatelet plus anticoagulant) may be optimal.
This approach could involve oral anticoagulation with a direct oral anticoagulant (DOAC) (e.g., apixaban or dabigatran at an adjusted dose suitable for renal function) plus single antiplatelet therapy (likely clopidogrel) instead of full DAPT to balance bleeding and thrombotic risks.
Duration of dual therapy should be minimized (e.g., 1–3 months), with a subsequent transition to anticoagulation monotherapy if the clinical team deems it safe based on follow-up.
Close Monitoring and Follow-Up:
Regular follow-up with echocardiography and clinical assessments will be essential post-MitraClip to evaluate mitral regurgitation reduction and ventricular function.
Blood monitoring will also be needed to adjust anticoagulant dosing as necessary, particularly in light of the patient’s renal function and elevated bleeding risk.
Final Decision
Primary Intervention: Perform the MitraClip procedure first to address mitral regurgitation.
Secondary Intervention: PCI for coronary revascularization, with a focus on minimizing stent use and adopting a simple dual antithrombotic regimen (anticoagulant plus single antiplatelet).
Antithrombotic Plan: Dual therapy for the shortest possible period post-PCI, transitioning to anticoagulation monotherapy based on bleeding and thrombotic risk reassessment.
This approach aims to optimize symptomatic and survival benefits while carefully balancing the high risks associated with anticoagulation and antiplatelet therapy.
Gemini
Given the complex scenario and high-risk factors, I would recommend a multidisciplinary team approach to develop a personalized treatment plan. This would involve careful consideration of the patient's comorbidities, risk factors, and preferences.
Here's a possible approach, building on the previous analysis:
Percutaneous Interventions:
MitraClip Procedure: Given the patient's age, comorbidities, and the suitability of the mitral valve anatomy, a percutaneous mitral valve repair using the MitraClip system could be considered as the first-line treatment for mitral regurgitation. This minimally invasive procedure offers a lower risk profile compared to open-heart surgery.
Multivessel PCI: To address the significant coronary artery disease, a multivessel PCI with drug-eluting stents could be performed to improve myocardial perfusion and reduce the risk of future cardiac events.
Anticoagulation Strategy:
Direct Oral Anticoagulants (DOACs): Given the patient's history of atrial fibrillation and the risk of stroke, a DOAC such as apixaban or rivaroxaban could be considered for stroke prevention.
Risk Assessment: A thorough assessment of the patient's bleeding risk using tools like HAS-BLED is crucial to determine the appropriate anticoagulant therapy and dosage.
Close Monitoring: Close monitoring of the patient's anticoagulation status, renal function, and bleeding risk is essential.
Antiplatelet Therapy:
Short-Term DAPT: A short duration of dual antiplatelet therapy (DAPT) may be considered after PCI to reduce the risk of stent thrombosis. However, this should be carefully balanced with the risk of bleeding.
Single Antiplatelet Therapy: After the initial DAPT period, the patient may be transitioned to single antiplatelet therapy for a longer duration.
Multidisciplinary Team Approach:
Heart Team: A multidisciplinary team, including cardiologists, cardiac surgeons, interventional cardiologists, and neurologists, should be involved in decision-making.
Shared Decision-Making: The patient and their family should be involved in the decision-making process, taking into account the risks and benefits of different treatment options.
Additional Considerations:
Close Monitoring: Close monitoring of the patient's clinical status, cardiac function, and renal function is essential.
Risk Factor Modification: Aggressive risk factor modification, including blood pressure control, lipid-lowering therapy, and smoking cessation, is crucial.
Palliative Care: In some cases, palliative care may be an important component of the treatment plan.
It is important to note that this is a complex case, and the optimal treatment strategy may vary depending on the individual patient's circumstances. A multidisciplinary team approach is essential to ensure the best possible outcome.
PerplexityAI
Final Decision
1. MitraClip Procedure
Rationale: The MitraClip offers a minimally invasive option to address the severe mitral regurgitation, which is contributing to the patient’s worsening symptoms of dyspnea and angina. Given the patient's high surgical risk due to age and comorbidities, this approach is appropriate.
2. Percutaneous Coronary Intervention (PCI)
Rationale: The presence of significant three-vessel coronary artery disease necessitates revascularization to improve myocardial perfusion and alleviate angina. PCI can be performed concurrently with the MitraClip procedure, optimizing the patient's overall cardiac function.
3. Antithrombotic Strategy
Anticoagulation: Initiate anticoagulation therapy (e.g., apixaban or rivaroxaban) tailored to the patient's atrial fibrillation.
Antiplatelet Therapy: Use a single antiplatelet agent (e.g., clopidogrel) alongside anticoagulation, considering the high bleeding risk due to the patient's history of cerebral hemorrhage. Continuous monitoring for any signs of bleeding or thromboembolic events will be essential.
4. Multidisciplinary Team Approach
Ensure that a multidisciplinary team, including cardiologists, neurologists, and possibly geriatric specialists, is involved in pre-procedural planning and post-procedural care to manage potential complications effectively.
5. Informed Consent
Discuss all risks, benefits, and alternatives with the patient and family members to ensure informed consent is obtained prior to proceeding with the interventions.
Conclusion
By opting for this combined approach, we aim to address both critical cardiac issues while minimizing surgical risks associated with traditional open-heart surgery. Continuous follow-up will be crucial to monitor recovery and adjust treatment as necessary, ensuring optimal outcomes for this high-risk patient.
MistralAI
Perform the MitraClip procedure.
Proceed with the first stage of PCI, targeting the most critical lesions, during the same hospitalization.
Initiate a short course of DAPT (1-3 months).
After the initial DAPT phase, start combination therapy with a DOAC and clopidogrel for up to 12 months.
Perform the second stage of PCI (if needed) after the initial DAPT phase, ideally within the 12-month combination therapy window.
Continue regular follow-ups and monitoring as outlined above.
This final decision considers the patient's complex clinical scenario, balancing the risks and benefits of interventions, and prioritizing treatments based on clinical status and comorbidities. The Heart Team should continually review and adjust the treatment plan as needed during follow-ups.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER NINETEEN: Double valvular regurgitation.
Premises:
76-year-old patient with arterial hypertension. Familiarity for non-specified connective tissue pathologies. Good general condition, athletic. For about 4 months, progressive decline in exercise tolerance and onset of dyspnoea for mild-moderate efforts.
ECG: sinus rhythm with frequent supraventricular extrasystoles, ventricular repolarization within limits.
Echocardiogram: EF 55%, dilated left ventricle (59 mm), moderate aortic insufficiency and severe mitral insufficiency. Dilation of the aortic root and ascending aorta (45 mm and 49 mm).
Transoesophageal echocardiogram: the transthoracic echocardiogram findings were confirmed, P3-A3 flail with second-order chordae tendineae rupture, MVA> 4 cm2, posterior leaflet > 10 mm, flail width < 15 mm.
Coronary-TC was negative for significant stenoses on coronary arteries.
Medical therapy with beta blockers and diuretics was started.
The patient was seen again after three months. Worsening of mitral insufficiency with three jets of insufficiency and dilation of the left atrium.
How would you manage this scenario? what would you do?
Medical theraphy was already on top. what would you do in the end? take a final decision
ANSWERS
ChatGPT
Default configuration
In this scenario, where medical therapy (beta-blockers, diuretics) has been optimized but the patient's condition has continued to worsen (e.g., increasing severity of mitral regurgitation, dilation of the left atrium, and declining exercise tolerance), the final decision should focus on the necessity of surgical intervention. Given the severity of the valvular pathology and the symptoms, here's the final management plan:
Surgical Intervention:
Mitral Valve Surgery: The patient has severe mitral regurgitation due to a flail leaflet with chordal rupture, which is causing significant symptoms (dyspnea, decline in exercise tolerance) and left ventricular dilation. Surgical repair is the preferred option due to better long-term outcomes compared to replacement, provided that the valve is amenable to repair (which is typically the case with a flail leaflet if other features of the valve allow for it).
Indication: Severe mitral regurgitation with symptoms (dyspnea, exercise intolerance), worsening over time.
Procedure: Mitral valve repair should be attempted if possible. This might involve techniques such as leaflet re-suspension, chordal replacement, or annuloplasty. If the valve cannot be repaired, then mitral valve replacement with a bioprosthetic valve should be considered, given the patient’s age and likely better outcomes with a bioprosthetic valve in this elderly patient.
Aortic Root and Ascending Aorta Surgery: The patient has aortic root dilation (45 mm) and ascending aorta dilation (49 mm). While the aorta is not yet at the threshold for surgery (usually >50 mm or rapidly growing), there is a concern given the patient's connective tissue disorder (even if unspecified), which could predispose to further aortic dilation or rupture. Therefore, it is prudent to involve a cardiac surgeon in evaluating the aorta as well:
Aortic surgery could be prophylactic in nature if the aortic dilation continues to increase or if there are signs of progressive aortic insufficiency. If the patient undergoes mitral valve surgery, the aorta should also be closely monitored during this period for any signs of worsening dilation or risk of dissection, especially given the risk associated with the connective tissue disorder.
Conclusion and Final Decision:
Given the progressive nature of the mitral regurgitation, the presence of severe MR, symptoms, and structural damage (flail leaflet, ruptured chordae, left ventricular dilation, and left atrial enlargement), the most appropriate course of action at this point is to refer for mitral valve surgery. This should be done urgently, as continued progressive MR can lead to worsening heart failure, arrhythmias, and ultimately worse outcomes. Surgical intervention (either repair or replacement) is the best option to halt further decline and improve the patient’s quality of life.
Plan:
Refer for surgical consultation as soon as possible for:
Mitral valve surgery (repair if feasible; otherwise, replacement).
Consideration of aortic root/ascending aorta surgery depending on progression and surgeon’s assessment.
Continue medical management perioperatively (beta-blockers, diuretics, heart failure agents as necessary) until surgery can be performed.
Ultimately, surgical intervention is the only definitive solution to address the severe mitral regurgitation and the structural changes that are contributing to the patient's worsening symptoms and decline in exercise tolerance.
Interrogation after upload of guidelines (ESC 2021 valvular heart disease) and supplementary data
In managing a 76-year-old patient with severe mitral regurgitation, moderate aortic insufficiency, and a worsening condition despite medical therapy, the guidelines on valvular heart disease by ESC/EACTS provide a few key recommendations that apply here:
Indications for Surgical Intervention:
For primary severe mitral regurgitation with symptoms or progressive LV dilation, surgical intervention is recommended, especially given the presence of worsening regurgitation and left atrial enlargement. The guidelines strongly suggest that early surgery should be considered in asymptomatic patients when a repair is feasible and durable, ideally performed at an experienced center(valvulopatie eng).
Criteria for Surgery in Asymptomatic Patients:
Surgery should be considered in asymptomatic patients with preserved LV function but presenting with factors like secondary atrial fibrillation or pulmonary hypertension. Although your patient is not asymptomatic, their decline in exercise tolerance and progressive symptoms further reinforce the recommendation for surgical assessment, especially if the patient has good surgical candidacy(valvulopatie eng).
Heart Team Assessment:
A Heart Team evaluation is essential to weigh the risks and benefits and decide the best treatment course, whether valve repair or replacement, possibly with combined management for both mitral and aortic issues given the aortic root dilation. The team should consider patient-specific factors like age, physical condition, and comorbidities to determine the optimal intervention(valvulopatie eng).
Given these considerations, early mitral valve surgery would likely be the next step, ideally aiming for a repair if the anatomy permits. The Heart Team could also evaluate whether combined intervention for the aortic dilation is needed.
Interrogation to ChatGPT browser
Given the patient’s progressive symptoms and the echocardiographic findings of severe mitral regurgitation (MR) due to P3-A3 flail, moderate aortic insufficiency, and dilation of the aortic root and ascending aorta, surgical intervention is warranted. The recommended approach is a combined procedure involving mitral valve repair and aortic root replacement.
Mitral Valve Repair:
• Indication: Severe MR with symptomatic progression and evidence of left atrial dilation.
• Procedure: Mitral valve repair is preferred over replacement due to better preservation of ventricular function and lower long-term morbidity. Techniques may include leaflet resection, chordal replacement, and annuloplasty. (Oxford Academic)
Aortic Root Replacement:
• Indication: Moderate aortic insufficiency with aortic root dilation measuring 45 mm
and ascending aorta dilation at 49 mm.
• Procedure: A valve-sparing aortic root replacement, such as the David procedure,
is recommended to preserve the native aortic valve while replacing the dilated aortic root. This approach has shown favorable outcomes in managing aortic root pathology. (Annals of Thoracic Surgery)
Combined Approach:
Performing both procedures concurrently addresses the patient’s complex pathology in a single surgical session, reducing overall risk and recovery time. This strategy has been demonstrated to be safe and effective, with excellent long-term valve durability. (Annals of Thoracic Surgery Short
Reports). In the end, given the patient’s symptomatic status, worsening mitral regurgitation, and structural changes to the heart, I would proceed with referral for surgery as the final decision.
Final Decision
Surgical Intervention:
Mitral Valve Repair (or replacement if repair is not feasible), as the mitral regurgitation is severe and progressing.
Aortic Valve Replacement (AVR), due to the moderate aortic insufficiency combined with aortic root dilation.
Consider Aortic Root Replacement if further imaging or surgical evaluation suggests that the root dilation poses an additional risk for progression.
Preoperative Management:
Continue current medical therapy with beta blockers and diuretics to manage symptoms and support hemodynamic stability until the surgery date.
This approach prioritizes a surgical solution to address both valves, aiming to resolve the root causes of the patient’s symptoms and prevent further deterioration.
Gemini
Given the patient's worsening condition and the limitations of medical therapy, surgical intervention appears to be the most appropriate course of action. The specific surgical approach would depend on several factors, including:
Valve Repair vs. Replacement: For the mitral valve, repair may be considered if feasible, especially in younger patients. However, given the severity of the valve disease and the patient's age, valve replacement might be the more appropriate option.
Aortic Valve Repair vs. Replacement: Aortic valve replacement is typically the preferred approach for aortic valve disease.
Timing of Surgery: The timing of surgery should be carefully considered, balancing the risks and benefits of immediate versus deferred surgery. Factors such as symptom severity, hemodynamic instability, and the risk of sudden cardiac death should be taken into account.
The patient's age, comorbidities, and overall health status are important factors to consider when making the final decision. A multidisciplinary team approach involving cardiologists, cardiothoracic surgeons, and other specialists can help optimize patient care.
PerplexityAI
In this scenario, where medical therapy has been optimized and the patient continues to experience worsening mitral insufficiency and symptoms, the final decision should focus on surgical intervention. Here's how to proceed:
Surgical Intervention
Mitral Valve Repair: Given the patient's severe mitral regurgitation due to chordae tendineae rupture and the presence of a flail leaflet, mitral valve repair should be prioritized if feasible. Repair techniques such as annuloplasty or leaflet resection are generally preferred over replacement because they preserve the patient's own valve structure, leading to better long-term outcomes and lower complication rates.
Consideration for Replacement: If the mitral valve is deemed irreparable during surgical evaluation, or if there are significant anatomical challenges, mitral valve replacement may be necessary. The choice between mechanical and biological prostheses will depend on the patient's age, lifestyle, and preferences regarding anticoagulation therapy.
Transcatheter Options: If the patient is at high surgical risk due to age or comorbidities, consider a minimally invasive approach such as transcatheter edge-to-edge repair (e.g., MitraClip) as an alternative to open-heart surgery. This can provide symptomatic relief with a shorter recovery time.
Preoperative Assessment
Multidisciplinary Team Evaluation: Involve a cardiothoracic surgeon experienced in valvular surgery for comprehensive assessment and planning. Ensure that all imaging studies (echocardiograms and possibly cardiac MRI) are reviewed to evaluate the severity of regurgitation and left ventricular function.
Optimize Patient Condition: Address any potential preoperative issues such as electrolyte imbalances or other medical conditions that could complicate surgery.
Postoperative Care
Monitoring: After surgery, the patient should be closely monitored in an intensive care setting for complications such as bleeding, infection, or arrhythmias.
Rehabilitation: Initiate a cardiac rehabilitation program post-discharge to aid recovery and improve functional capacity.
In conclusion, given the patient's deteriorating condition despite optimized medical therapy, surgical intervention—preferably mitral valve repair—should be pursued promptly to alleviate symptoms and prevent further cardiac deterioration.
MistralAI
Based on the information provided and the fact that medical therapy has been optimized, I would recommend proceeding with surgical intervention in this case. Here's the rationale behind this decision:
Severe Mitral Regurgitation (MR): The patient has severe MR with a flail leaflet and worsening symptoms despite optimal medical therapy. Mitral valve surgery is indicated in symptomatic patients with severe degenerative MR and suitable anatomy for repair.
Worsening MR and Left Atrial Dilation: The recent echocardiogram showed worsening MR with three jets of insufficiency and dilation of the left atrium, suggesting disease progression.
Concomitant Aortic Pathology: The patient also has moderate aortic insufficiency and dilation of the aortic root and ascending aorta. Addressing these issues surgically at the same time as the mitral valve repair could be beneficial to prevent future complications.
Good General Condition: The patient is 76 years old but has a good general condition and an athletic background, suggesting that they may tolerate surgery well and benefit from an improvement in quality of life post-surgery.
Low Surgical Risk: With optimal preoperative condition and a thorough preoperative evaluation, the surgical risk should be acceptable.
Final Decision:
Proceed with surgical intervention, with the following goals:
Mitral valve repair, as the valve anatomy appears suitable for repair (P3-A3 flail with second-order chordae tendineae rupture, posterior leaflet > 10 mm, flail width < 15 mm, MVA > 4 cm2).
Evaluate the aortic valve and consider repair or replacement if necessary.
Replace the aortic root and/or ascending aorta if indicated based on intraoperative findings and current guidelines.
The surgery should be performed by an experienced cardiac surgeon in a center with expertise in valvular heart disease and aortic surgery. The patient should be fully informed about the benefits and risks of the procedure, and their preferences should be taken into account in the final decision-making process. Close postoperative follow-up should be ensured to monitor the patient's recovery and optimize their outcome.
----------------------------------------------------------------------------------------------------------------------
CASE NUMBER TWENTY: A case of a patient with atrial fibrillation, thrombosis of left atrial appendage and previous stroke.
Premises:
66-year-old patient with permanent atrial fibrillation. TIA about 8 months ago. Two months after cerebral ischemic stroke. No other cardiovascular risk factors and important pathologies in past medical history. Patient assumed anticoagulant therapy with Apixaban 5 mg 1 cp x 2 per day for about 10 years.
ECG: atrial fibrillation at an average ventricular response of 80 BPM.
Echocardiogram: EF 60%, dilated left atrium and mild mitral insufficiency.
Transoesophageal echocardiogram: the findings of the transthoracic echocardiogram were confirmed; presence of a thrombotic formation of 8 x 9 mm inside the left atrial appendage.
Anticoagulant therapy was already optimized and TEE was repeated at two months of distance from the previous one. The previous results and the thrombus in the left atrial appendage were confirmed again.
Blood tests were performed previously, including thrombophilia panel. An hematologist was consulted but no conditions of blood disease was found.
How would you manage this scenario? What would you do?
ANSWERS
ChatGPT
Default configuration
Given the persistent thrombus in the left atrial appendage despite optimized anticoagulation with Apixaban and the patient's history of stroke, I would recommend the following:
Final Decision:
Refer for Left Atrial Appendage Occlusion (LAAO):
Given the high risk of further thromboembolic events, I would proceed with a referral to a cardiologist specializing in interventional procedures for evaluation and potential LAA occlusion. This is a viable option to reduce stroke risk in patients with atrial fibrillation who cannot maintain effective anticoagulation.
Continue Anticoagulation Until Procedure:
Continue Apixaban at the current dose until the LAAO is performed, monitoring the patient closely for any signs of complications.
Patient Education and Follow-Up:
Educate the patient about the procedure, its benefits, and risks, and ensure they understand the importance of adherence to their current anticoagulation regimen until the intervention.
Schedule regular follow-ups to monitor the patient's clinical status and manage any new symptoms. This approach balances the need to address the existing thrombus while minimizing the risk of future strokes.
Interrogation after upload of ESC guidelines and supplementary data
Given the patient's history of recurrent thromboembolic events despite optimized anticoagulation and the persistent thrombus in the left atrial appendage (LAA), a definitive approach combining treatment with safety is critical. Here’s a final course of action based on current evidence and guidelines:
Left Atrial Appendage Occlusion (LAAO): Proceed with percutaneous or surgical LAAO. This approach is suitable given the persistent thrombus despite anticoagulation and the significant risk of recurrent stroke. This step aligns with the ESC guidelines, which recommend LAAO in cases where anticoagulation alone does not mitigate thromboembolic risk(atrial fibrillation).
Switch in Anticoagulation (if LAAO is not immediately feasible): Transitioning from Apixaban to warfarin with close INR monitoring would be prudent if there’s a delay in scheduling LAAO. Some studies suggest that warfarin may offer superior protection in thrombus resolution in selected cases compared to DOACs, particularly when DOAC therapy has proven insufficient(atrial fibrillation).
Continued Monitoring: After LAAO, continue anticoagulation temporarily until confirmed closure of the LAA (if percutaneous) and assess the patient’s bleeding risk and thrombus resolution.
This combination approach prioritizes stroke prevention, given the high risk posed by the thrombus, while aiming to mitigate the limitations of anticoagulation alone in this patient.
Interrogation to ChatGPT browser
Given the persistence of the left atrial appendage (LAA) thrombus despite long-term optimized anticoagulation with apixaban and the patient's history of stroke, a final decision would likely involve:
Switching to Warfarin: Transitioning the patient to warfarin with a target INR of 2.5–3.5 would allow for closer monitoring and adjustments based on INR. Warfarin has sometimes shown effectiveness in managing LAA thrombi in patients where DOACs have not been sufficient.
Planning for LAA Occlusion: Concurrently, I would initiate an evaluation for left atrial appendage occlusion (using a device like the Watchman) as a longer-term solution. This procedure could prevent future thrombus formation and embolic risk by closing off the LAA, which is a common site of thrombus formation in atrial fibrillation.
Repeat Imaging in 1–3 Months: To confirm if warfarin is effective, I would plan a repeat TEE or cardiac CT to reassess the thrombus after initiating warfarin therapy. If the thrombus remains or if the patient has any complications with warfarin, I would expedite the LAA occlusion procedure.
Final Decision
Primary Action: Switch from apixaban to warfarin with close INR monitoring.
Definitive Intervention: Proceed with LAA occlusion if the thrombus persists or if INR control proves challenging. This approach balances the need for immediate thrombus management with a longer-term solution to prevent future thromboembolic events.
Gemini
Given the patient's history of atrial fibrillation, previous stroke, and persistent LAA thrombus despite optimized anticoagulation, I would strongly consider LAAC as a definitive treatment option.
Reasons for LAAC:
Persistent Thrombus: The thrombus has persisted despite optimal anticoagulation, indicating a high risk of thromboembolic events.
History of Stroke: The patient has a history of stroke, further emphasizing the need for aggressive prevention strategies.
Moderate Bleeding Risk: While the patient's bleeding risk should be carefully assessed, LAAC is generally considered a relatively safe procedure with a low risk of major bleeding complications.
Potential Benefits of LAAC:
Reduced Thromboembolic Risk: LAAC can significantly reduce the risk of stroke and other thromboembolic events by eliminating the source of thrombus formation.
Improved Quality of Life: By reducing the risk of future strokes, LAAC can improve the patient's quality of life and functional independence.
Potential Reduction in Anticoagulation: In some cases, LAAC may allow for a reduction in the intensity of anticoagulation therapy, further reducing the risk of bleeding complications.
Important Considerations:
Careful Patient Selection: It is crucial to carefully select patients who are suitable candidates for LAAC. Patients with significant comorbidities, high bleeding risk, or complex anatomy may not be ideal candidates.
Experienced Operator: LAAC should be performed by experienced operators to minimize the risk of complications.
Close Monitoring: Regular follow-up and monitoring are essential to assess the long-term efficacy and safety of LAAC.
Ultimately, the decision to proceed with LAAC should be made on an individual basis after careful consideration of the patient's specific circumstances and in consultation with a multidisciplinary team.
PerplexityAI
Final Decision:
1. Refer for Left Atrial Appendage Closure (LAAC)
Given the persistence of the thrombus in the LAA despite optimal anticoagulation with Apixaban, I would recommend referring the patient for Left Atrial Appendage Closure (LAAC). This intervention is particularly indicated due to:
The high risk of embolization associated with the existing thrombus.
The patient's history of stroke and TIA, which underscores the need for effective stroke prevention strategies.
The potential benefits of LAAC in reducing stroke risk without the ongoing need for anticoagulation, especially if there are concerns about adherence or efficacy of current therapy.
2. Continue Anticoagulation Until Procedure
While awaiting the LAAC procedure, I would continue the patient on Apixaban at the current dose (5 mg twice daily) to minimize the risk of thromboembolic events. Close monitoring for any signs of worsening symptoms or complications would be essential during this period.
3. Multidisciplinary Team Coordination
Coordinate with a multidisciplinary team including:
Electrophysiologist/Cardiologist: To assess and perform the LAAC procedure.
Hematologist: To ensure there are no underlying coagulation disorders that could complicate management.
Neurologist: For ongoing assessment of stroke risk and management.
4. Patient Education and Follow-Up
Educate the patient about:
The nature of their condition and the importance of the upcoming LAAC procedure.
Signs and symptoms of stroke to monitor closely.
The importance of adherence to medications until the procedure is performed.
5. Schedule Regular Follow-Up Appointments
Plan for regular follow-up appointments post-procedure to monitor recovery, assess for any complications, and adjust any ongoing medication needs based on the outcome of the LAAC.
Conclusion: In conclusion, referring for Left Atrial Appendage Closure is a decisive step in managing this patient’s high stroke risk due to persistent thrombus formation despite optimal anticoagulation therapy. This approach aims to provide effective long-term protection against stroke while addressing immediate risks associated with the existing thrombus.
MistralAI
Based on the provided information, here's a final decision on how to proceed with the patient's management:
Switch anticoagulant: Given the persistent left atrial appendage (LAA) thrombus despite optimal Apixaban therapy, I would switch the anticoagulant to low molecular weight heparin (LMWH), such as Enoxaparin, at therapeutic doses (e.g., 1 mg/kg twice daily), after consultation with a cardiologist and hematologist. This switch is based on some evidence suggesting that LMWH may be more effective in resolving intracardiac thrombi.
Follow-up imaging: I would schedule a follow-up transesophageal echocardiogram (TEE) in 3 months to assess the resolution of the LAA thrombus.
Plan for Left Atrial Appendage Occlusion (LAAO): If the thrombus persists despite LMWH therapy, I would proceed with planning for LAAO device implantation, such as Watchman or Amulet. This would involve:
Consulting with an interventional cardiologist or electrophysiologist experienced in LAAO procedures.
Discussing the risks and benefits of the procedure with the patient and their family.
Scheduling the procedure, if the patient and the healthcare team agree that it's the best course of action.
Continued monitoring and risk factor management: Regardless of the outcome of the LMWH therapy and LAAO procedure, I would continue to monitor the patient closely, ensure compliance with the anticoagulation regimen, and manage any potential new risk factors.
Final decision summary:
Switch Apixaban to Enoxaparin (LMWH) at therapeutic doses.
Schedule a follow-up TEE in 3 months.
If the thrombus persists, proceed with planning for LAAO device implantation.
Continue close monitoring and risk factor management.
This decision takes into account the patient's history, current treatment, and the persistent nature of the LAA thrombus. It is important to involve the patient and the multidisciplinary team in the decision-making process and to tailor the treatment plan to the patient's individual needs and preferences.
References
- Itelman E, Witberg G, Kornowski R. AI-assisted clinical decision making in interventional cardiology: the potential of commercially available large language models. JACC Cardiovasc Interv. 2024;17(15):1858-1860. doi:10.1016/j.jcin.2024.06.013
- Alexandrou M, Mahtani AU, Rempakos A, et al. Performance of ChatGPT on ACC/SCAI interventional cardiology certification simulation exam. JACC Cardiovasc Interv. 2024;17(10):1292-1293. doi:10.1016/j.jcin.2024.03.012
- Geneş M, Çelik M. Assessment of ChatGPT's compliance with ESC-acute coronary syndrome management guidelines at 30-day intervals. Life (Basel). 2024;14(10):1235. doi:10.3390/life14101235.
- Goh E, Gallo R, Hom J, et al. Large language model influence on diagnostic reasoning: a randomized clinical trial. JAMA Netw Open. 2024;7(10):e2440969. doi:10.1001/jamanetworkopen.2024.40969
- Gurbuz DC, Varis E. Is ChatGPT knowledgeable of acute coronary syndromes and pertinent European Society of Cardiology Guidelines? Minerva Cardiol Angiol. 2024;72(3):299-303. doi:10.23736/S2724-5683.24.06517-7
- Huwiler J, Oechslin L, Biaggi P, Tanner FC, Wyss CA. Experimental assessment of the performance of artificial intelligence in solving multiple-choice board exams in cardiology. Swiss Med Wkly. 2024;154:3547. doi:10.57187/s.3547
- Madaudo C, Parlati ALM, Di Lisi D, et al. Artificial intelligence in cardiology: a peek at the future and the role of ChatGPT in cardiology practice. J Cardiovasc Med (Hagerstown). 2024;25(11):766-771. doi:10.2459/JCM.0000000000001664
- Geneş M, Deveci B. A clinical evaluation of cardiovascular emergencies: a comparison of responses from ChatGPT, emergency physicians, and cardiologists. Diagnostics (Basel). 2024;14(23):2731. doi:10.3390/diagnostics14232731
- Sarraju A, Ouyang D, Itchhaporia D. The opportunities and challenges of large language models in cardiology. JACC Adv. 2023;2(7):100438. doi:10.1016/j.jacadv.2023.100438
- Pay L, Yumurtaş AÇ, Çetin T, Çınar T, Hayıroğlu Mİ. Comparative evaluation of Chatbot responses on coronary artery disease. Turk Kardiyol Dern Ars. 2025;53(1):35-43. doi:10.5543/tkda.2024.78131
- Salihu A, Meier D, Noirclerc N, et al. A study of ChatGPT in facilitating heart team decisions on severe aortic stenosis. EuroIntervention. 2024;20(8):e496-e503. doi:10.4244/EIJ-D-23-00643
- Wu X, Huang Y, He Q. A large language model improves clinicians' diagnostic performance in complex critical illness cases. Crit Care. 2025;29(1):230. doi:10.1186/s13054-025-05468-7
- Novak A, Rode F, Lisičić A, et al. The pulse of artificial intelligence in cardiology: a comprehensive evaluation of state-of-the-art large language models for potential use in clinical cardiology. medRxiv. Preprint posted August 8, 2023. doi:10.1101/2023.08.08.23293689
- Pierri MD, Galeazzi M, D’Alessio S, et al. Evaluating large language models in cardiology: a comparative study of ChatGPT, Claude, and Gemini. Hearts. 2025;6(3):19. doi:10.3390/hearts6030019
- Masanneck L, Meuth SG, Pawlitzki M. Evaluating base and retrieval augmented LLMs with document or online support for evidence based neurology. NPJ Digit Med. 2025;8(1):137. doi:10.1038/s41746-025-01536-y
- Ozmen BB, Mathur P. Evidence-based artificial intelligence: implementing retrieval-augmented generation models to enhance clinical decision support in plastic surgery. J Plast Reconstr Aesthet Surg. 2025;104:414-416. doi:10.1016/j.bjps.2025.03.053