Ruptured Intra-Aortic Balloon Pump Balloon Entrapment Successfully Removed Percutaneously Without Vascular Repair
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00357. Epub November 21, 2025.
An 83-year-old man was admitted with non-ST-segment elevation myocardial infarction (NSTEMI) and cardiogenic shock. Echocardiography revealed a left ventricular ejection fraction of 35%. His medical history included diabetic kidney disease, and a prior NSTEMI 3 years earlier, for which he underwent percutaneous coronary intervention (PCI) with deployment of 2 drug-eluting stents in the right coronary artery (RCA).
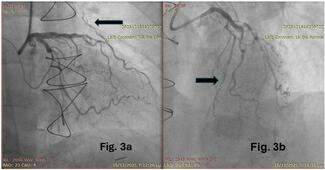
Urgent coronary angiography demonstrated 99% in-stent restenosis in the RCA. PCI was successfully performed using a 3.0-mm drug-coated balloon (DCB), yielding a satisfactory result (Figure 1). Despite this, the patient remained hypotensive, with a systolic blood pressure (SBP) of 80 mm Hg on inotrope support. An 8F Arrow (Teleflex) intra-aortic balloon pump (IABP) was inserted via the left common femoral artery, providing good augmentation. The patient stabilized, with his SBP rising to 110 mm Hg, allowing gradual weaning of inotropes.
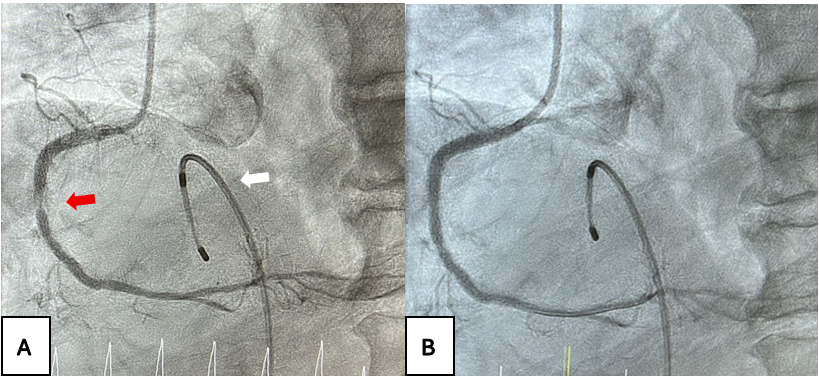
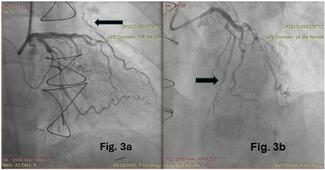
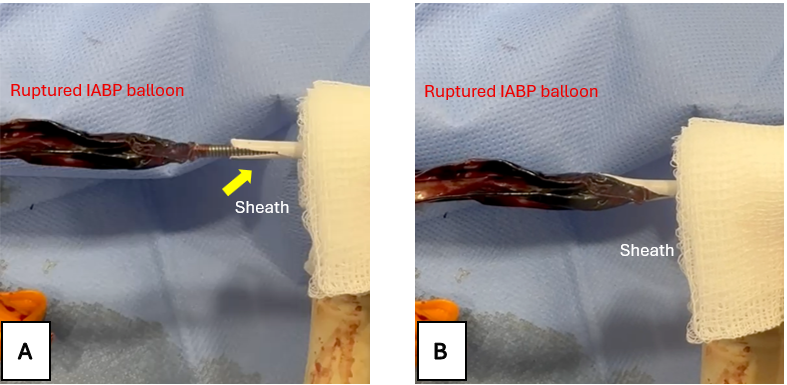
Four hours later, the IABP alarm sounded because of failure to inflate, raising suspicion of balloon rupture attributable to aortic calcification. Emergency IABP removal was planned. A long wire (0.025-inch × 175-cm J-wire) was inserted through the IABP lumen. Standard balloon aspiration was attempted prior to removal, but resistance was encountered when withdrawing the IABP from the arteriotomy site. Clot formation within the balloon likely caused bulging, preventing extraction (Figure 2A).
To address this, the 8F sheath was withdrawn over the wire, and its tip was cut 1 cm longitudinally to create a flared end. The flared sheath was then carefully readvanced into the femoral artery lumen via the arteriotomy. This maneuver smoothed out the bulging IABP balloon, enabling complete removal of the system (Figures 2B and 3). Given the anticipated arteriotomy size exceeding 8F post-removal, a 14F MANTA vascular closure device (Teleflex) was deployed, successfully closing the wound. The vascular surgery team remained on standby throughout for potential open surgical bailout in case percutaneous removal failed.
This case demonstrates how flaring the sheath tip can smooth out a bulging, stuck, ruptured IABP balloon, facilitating successful percutaneous removal and negating the need for surgical intervention.
Affiliations and Disclosures
Kwok-Ho Yau, MBBS1; Tin Wah Christopher Lau, MBBS1; Justin Ka-Ho Wong, MBBS1; Samuel Tsoon-Wuan Lo, MBBS2; Kin-Lam Tsui, MBBS, FACC1
From the 1Cardiology Team, Department of Medicine, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR; 2Vascular Team, Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient(s) for the study and/or intervention(s) described in the manuscript and for the publication of their data/thereof, including any and all images.
Address for correspondence: Kwok-Ho Yau, MBBS, 3 Lok Man Road, Chai Wan, Hong Kong. Email: jason200200200@hotmail.com