Inadvertent Hepatic Vein Puncture During Emergent Pericardiocentesis
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2026. doi:10.25270/jic/25.00391. Epub January 6, 2026.
A 46-year-old man with inferior wall myocardial infarction with complete heart block underwent primary percutaneous coronary intervention to the right coronary artery with temporary pacing. Twelve hours later, he developed sudden-onset dyspnea with a blood pressure of 70/50 mm Hg and a heart rate of 120 beats per minute. Echocardiogram showed massive pericardial effusion with right ventricular (RV) collapse.
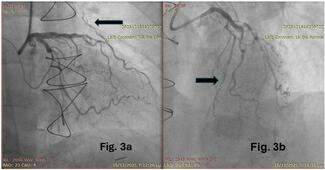
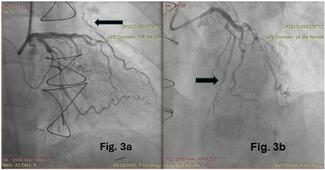
As lead-induced RV perforation causing tamponade was suspected, echocardiography-guided bedside pericardiocentesis was attempted via a 6F sheath. However, there was no hemodynamic improvement despite aspiration and autotransfusion. Contrast injection into the sheath showed opacification of a hepatic vein with trauma to the small branches (Figure A; Video). Another sheath was inserted under fluoroscopic guidance, through which 200 mL of hemorrhagic fluid was aspirated via pigtail (after confirming position with contrast) with hemodynamic improvement. The cardiothoracic surgery team advised computed tomography of the chest and abdomen, which showed the ectopic sheath lying in the hepatic parenchyma (Figure B and C). We switched to single antiplatelet with repeated pigtail drainage and output reducing over next 2 days. Under surgical backup, the ectopic sheath was removed with hourly abdominal girth and lactate monitoring. Subsequently, the temporary pacemaker lead was removed after 72 hours; the pigtail was removed 48 hours later. The patient was stable at discharge with no fluid re-accumulation.
It may be difficult to see the needle trajectory in the ultrasound during emergency bedside pericardiocentesis; henceforth, in doubtful cases, it is advisable to check the needle position with agitated saline before dilating the tract.
Affiliations and Disclosures
Neha Chopra, MD, DM1; Sourabh Agstam, MD, DM, MRCP2; Devesh Kumar, MD, DM, MRCP1; Surbhit Bhadauria, MD1; Anwar Hussain Ansari, MD, DM1
From the 1Department of Cardiology, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India; 2Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication, including photographs.
Address for correspondence: Devesh Kumar, MD, DM, MRCP, Department of Cardiology, 7th Floor, Super Speciality Vlock, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi 110029, India. Email: devesh2.DK@gmail.com