Expanding the Role of Interventional Cardiology: Covered Stent Rescue of Carotid Blowout Syndrome Secondary to Nasopharyngeal Carcinoma
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2026. doi:10.25270/jic/25.00362. Epub January 6, 2026.
Carotid blowout syndrome (CBS) is a catastrophic complication that most commonly occurs after surgical or radiotherapeutic treatment of head and neck malignancies. Mortality rates remain high, and early endovascular intervention is essential. Surgical repair is frequently limited by fibrosis, necrosis, and distorted anatomy. Covered stent implantation offers a rapid and effective minimally invasive option. Here, we present a case of CBS secondary to nasopharyngeal carcinoma successfully treated by an interventional cardiology team.
A 59-year-old man with diabetes mellitus and a history of nasopharyngeal carcinoma—treated with surgical resection, chemoradiotherapy, and tracheostomy—presented with recurrent syncope, fluctuating blood pressure, and persistent anemia. He reported intermittent bleeding around the tracheostomy site for several weeks.
On examination, he was pale, tachycardic (108 bpm), and mildly hypotensive (95/60 mm Hg), with continuous oozing around the tracheostomy. Laboratory findings showed a hemoglobin level of 7.2 g/dL, with other parameters stable. Contrast-enhanced neck CT demonstrated a necrotic infiltrative mass invading the left internal carotid artery and disrupting the arterial wall.
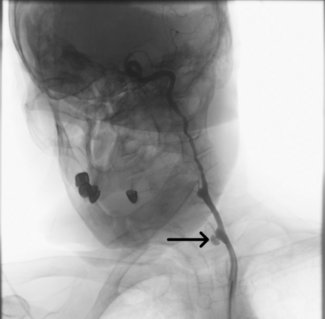
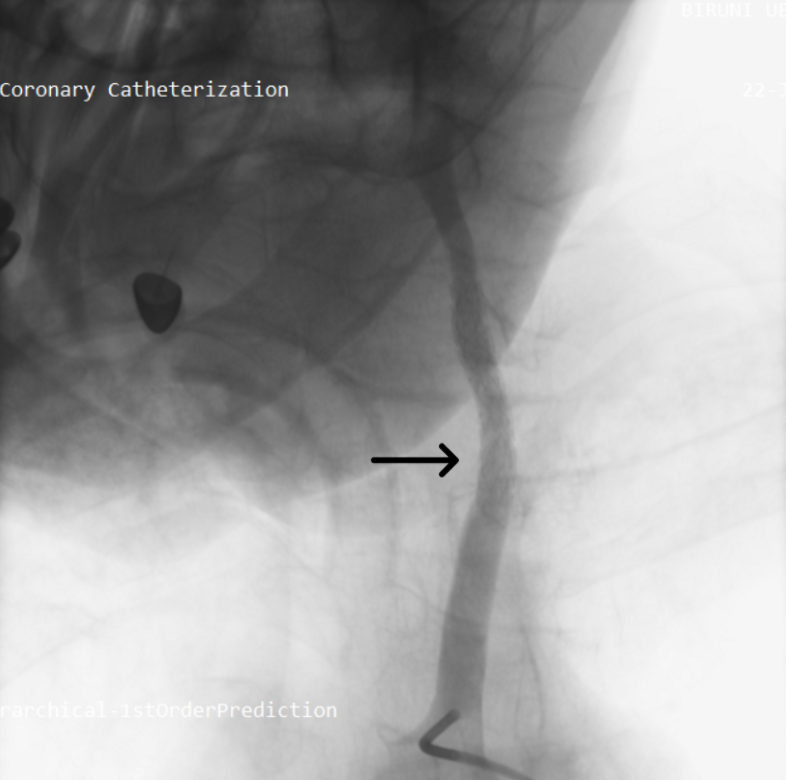
Given the hemodynamic instability, recurrent syncope, and imaging findings suggestive of carotid destruction, a multidisciplinary team involving cardiology, neurology, and oncology recommended urgent digital subtraction angiography (DSA) with therapeutic intent. Right femoral access was obtained, and a 6F Judkins Right 4.0 guiding catheter was advanced into the left common carotid artery. An Amplatz Super Stiff Guidewire (Boston Scientific) was positioned across the lesion, followed by placement of a 6F long sheath to ensure procedural support. DSA revealed active contrast extravasation at the site of tumoral invasion (Figure 1, Video 1).
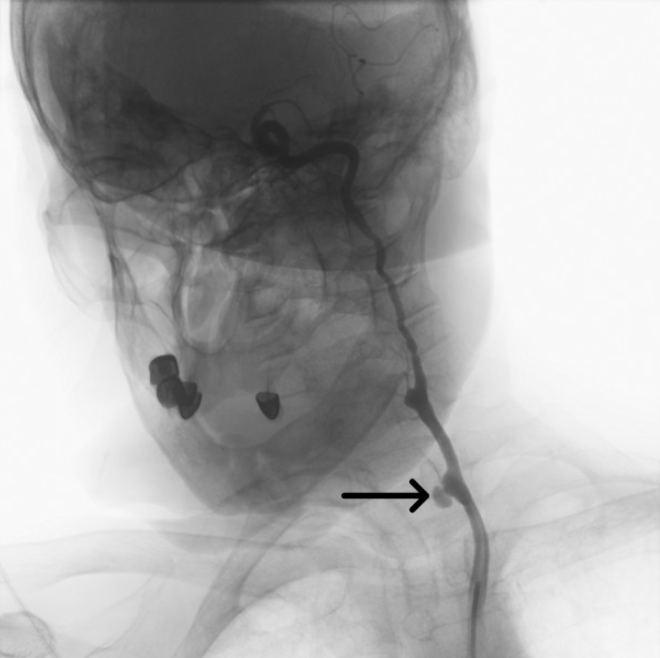
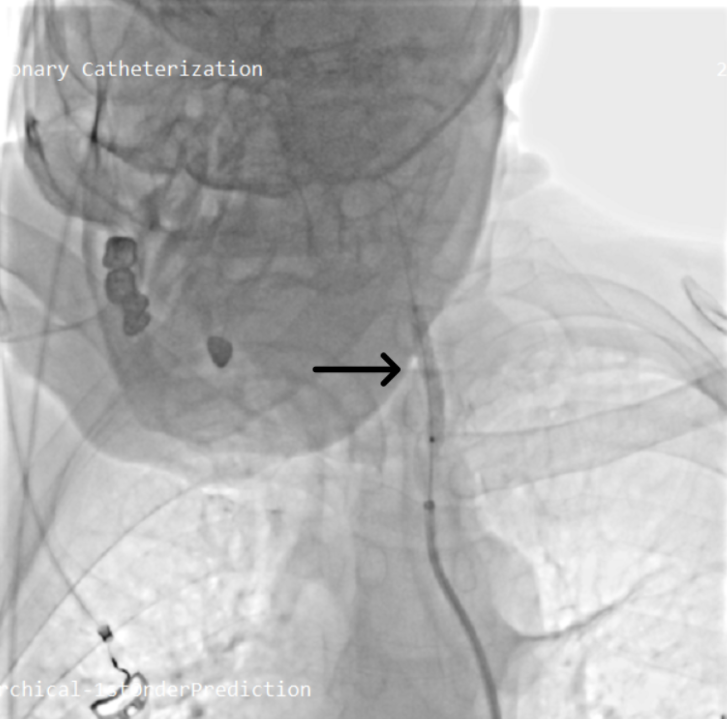
The bleeding segment was selectively wired. A 5 × 40-mm covered stent graft was deployed across the ruptured segment (Figure 2, Video 2); initial deployment was complicated by proximal slippage but hemostasis was ultimately achieved. The stent was then post-dilated with a 7 × 20-mm balloon to optimize apposition (Figure 3, Video 3). Final angiography confirmed complete sealing of the rupture and restoration of antegrade carotid flow (Figure 4, Videos 4 and 5).
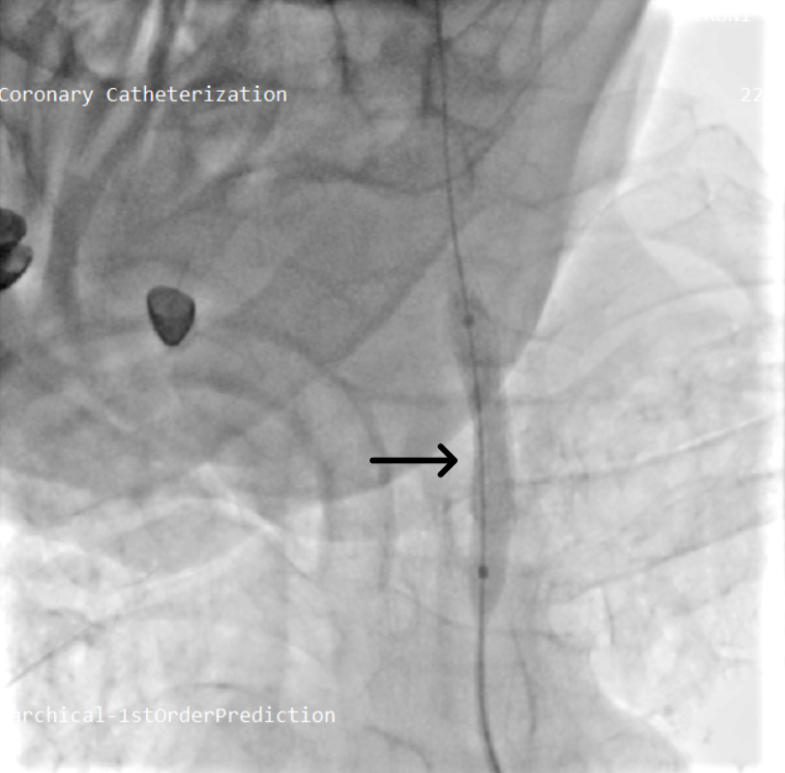
Antiplatelet management with aspirin and clopidogrel was initiated based on multidisciplinary consensus, and the patient was placed under close hemogram monitoring. Hemodynamic parameters stabilized promptly, and no further bleeding occurred.
At the 6-month follow-up, the patient was asymptomatic, with Doppler ultrasonography confirming full stent patency and preserved antegrade internal carotid artery flow.
Carotid blowout syndrome is a rare but life-threatening emergency in patients with head and neck cancer, particularly those who have undergone radiotherapy. Surgical repair is often technically prohibitive because of fibrosis, tissue fragility, and altered anatomy. Endovascular covered stent implantation provides immediate hemostasis while maintaining carotid patency, and multiple clinical series have demonstrated high technical success with favorable clinical outcomes.
Covered stents are especially advantageous in malignancy-related CBS, where the risks of rebleeding and reintervention are substantial. Our case adds to this evidence by demonstrating that successful treatment is feasible even in a previously irradiated carotid segment directly invaded by nasopharyngeal carcinoma—an environment where surgery is often unsafe or impossible. Additionally, the rapid and effective management achieved by an interventional cardiology team underscores the evolving role of cardiologists in handling urgent non-coronary vascular crises. This case illustrates how interventional cardiology can provide life-saving endovascular therapy in complex oncovascular emergencies previously considered outside its traditional scope.
In summary, carotid blowout syndrome requires immediate multidisciplinary action. Covered stent implantation can achieve rapid hemostasis while preserving carotid flow, even in previously irradiated, tumor-invaded segments. This case supports the expanding role of interventional cardiology in time-critical oncovascular emergencies.
Affiliations and Disclosures
Şevval Ilke Ebeoğlu, MD¹; Abdullah Ömer Ebeoğlu, MD²; İpek Aydın, MD¹; Ömer Doğan, MD¹; Okay Abacı, MD³
From the ¹Department of Cardiology, Istanbul University–Cerrahpaşa Institute of Cardiology, Istanbul, Turkey; ²Department of Cardiology, University of Health Sciences, Bağcılar Training and Research Hospital, Istanbul, Turkey; ³Department of Cardiology, Faculty of Medicine, Biruni University, Istanbul, Turkey.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Şevval Ilke Ebeoğlu, MD, Cardiology Institute, Department of Cardiology, Istanbul University–Cerrahpaşa, Istanbul 34098, Turkey. Email: ilkesevval@gmail.com