Percutaneous Removal of Pulmonary Intravascular Foreign Bodies in Children
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
Abstract
Objectives. This retrospective study aims to evaluate the safety and efficacy of percutaneous removal of pulmonary intravascular foreign bodies in children.
Methods. This single-center, retrospective study analyzed cases of pulmonary intravascular foreign body removal in children over a 13-year peiod.
Results. There were a total of 9 children, with a mean age of 8.6 years. The most common foreign bodies were catheter fragments (n = 7). The success rate of foreign body retrieval was 100%, with only 1 case of transient arrhythmia as a complication.
Conclusions. Preliminary findings suggest that percutaneous retrieval is a safe and effective method for removing pulmonary intravascular foreign bodies in children.
Introduction
The increased number of endovascular therapies and placement of central venous catheters in children has led to an associated increase in the incidence of embolized foreign bodies. In the absence of penetrating trauma, foreign bodies in the pulmonary circulation are almost always iatrogenic.1 Catheter fragments are the most common embolized intravascular foreign bodies and can be potentially life-threatening.2-4 One study reported an incidence of catheter embolization of 0.67% in a single tertiary care hospital over 6 years.5 Major complications of embolized fragments include pulmonary abscess, infection, arrhythmias, thrombosis, atrial perforation, and sudden death.6 Percutaneous retrieval is the treatment of choice for removing intravascular embolized catheter fragments, with surgical management being the second-line treatment.7,8
Embolization of the foreign body into the pulmonary circulation is rare but can result in significant morbidity. Most of the existing literature is based on adult studies, and there is a considerable gap in the literature regarding this complication in the pediatric population. Percutaneous technique and procedural variables for removing intravascular foreign bodies differ in children, with varying risks of complications.9 Our study aimed to specifically investigate the safety and efficacy of percutaneous pulmonary intravascular foreign body removal in the pediatric population.
Methods
In this single-center retrospective study, patients under 18 years of age who underwent pulmonary intravascular foreign body removal in a pediatric tertiary care hospital over a 13-year period were identified. Foreign bodies restricted to the heart and peripheral venous circulation were excluded. Demographic (age, gender), diagnostic (type, cause, and site of foreign body; presenting symptoms), and procedural (diagnostic imaging, guidance imaging, prophylactic antibiotics, retrieval access site, type and size of the catheter, guidewire, sheath size, retrieval device, hemostasis, outcome) data were collected. The cause of foreign bodies was divided into 3 types: catheter fracture (spontaneous or during attempted removal), spontaneous catheter disconnection, and embolization (coils or embolic material). Descriptive analyses were conducted using Statistical Package for the Social Sciences IBM version 29.0.0.0 (241).
This study was reviewed by the Institutional Review Board (IRB) and determined to qualify for exemption under 45 CFR 46.104(d)(4)(iii) and a waiver of HIPAA authorization per 45 CFR 164.512(i)(2)(ii). Informed consent was obtained from the patients/parents for the studies and/or interventions described in the manuscript, and the IRB approved the waiver of consent to publish existing de-identified data and records.
Technique
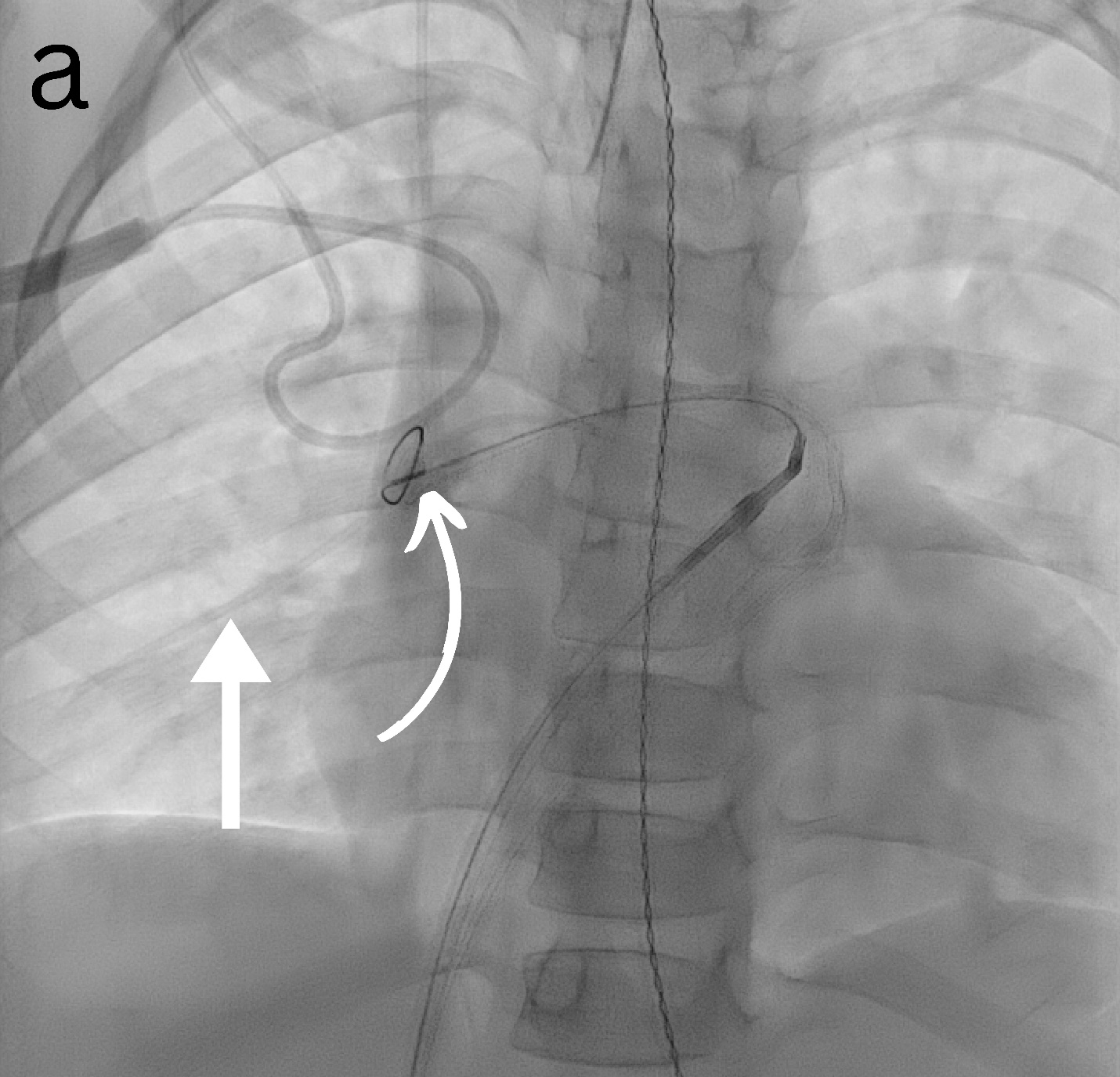
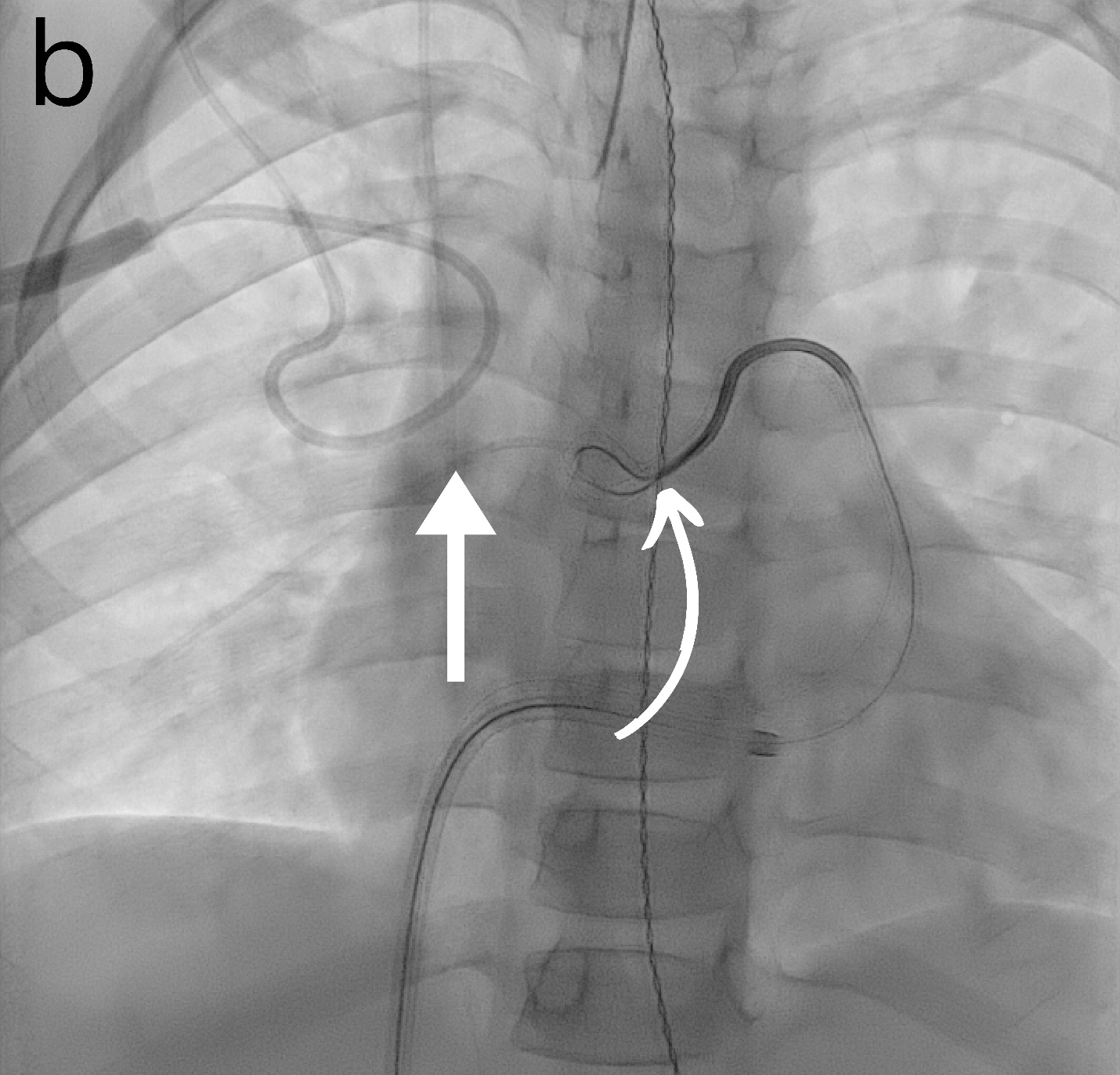
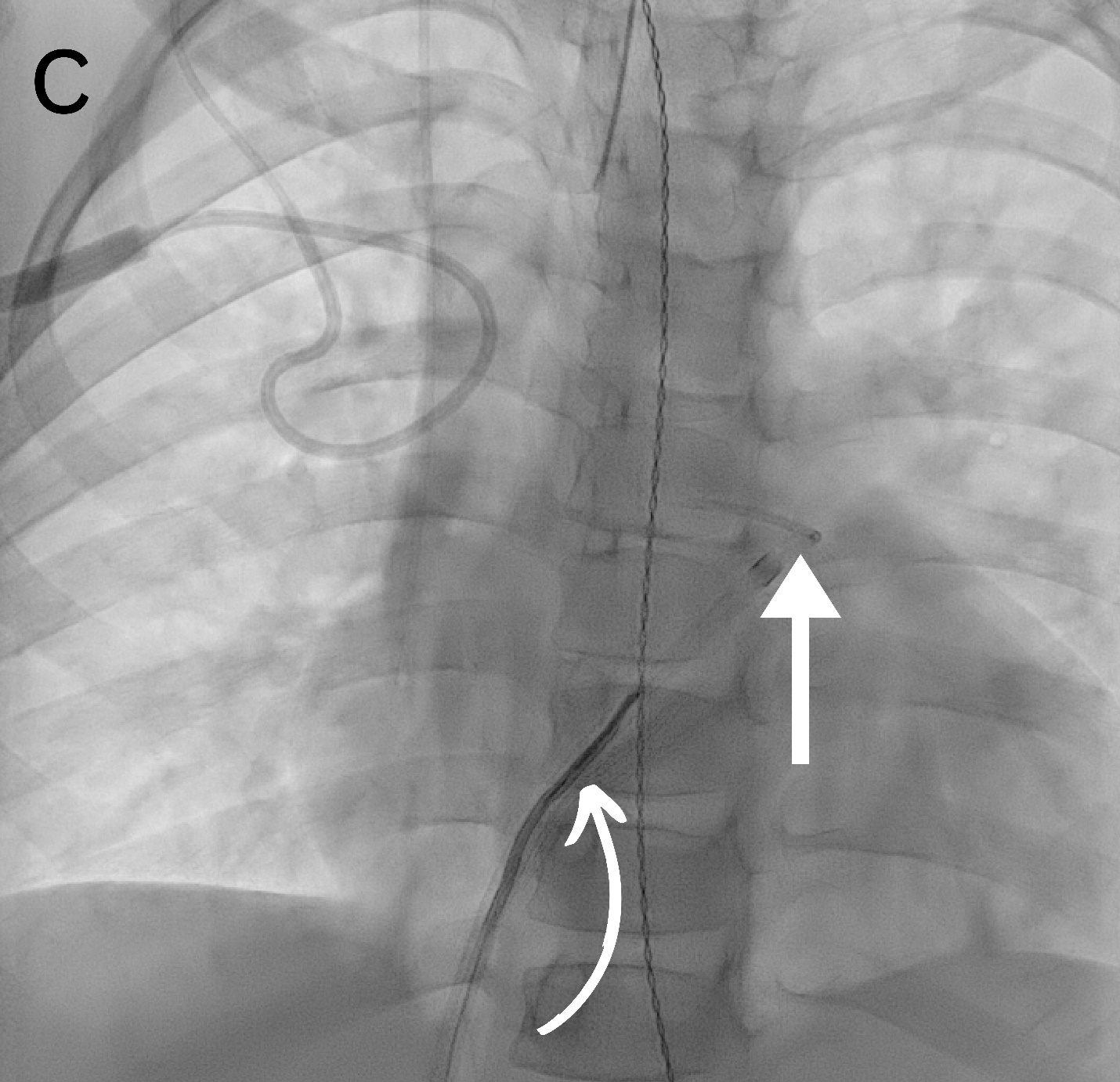
All the procedures were performed under general anesthesia. No prophylactic antibiotics were used for any procedures. Vascular access was obtained through the femoral veins. Ultrasound and fluoroscopy were the guidance modalities used in all (Figure). The retrieval sheath size ranged from 4 to 14 French (Fr). Various angled and reverse-angled catheters were used to reach the embolization site, with sizes ranging from 4 to 6 Fr. A snare was used to retrieve the foreign body in 8 cases, while a combination of snare, aspiration catheter, and suction device was used in 1 case. A single-loop snare device was used in all patients but one, in which a combination of single and tri-loop snare devices was used. The loop sizes of snare devices ranged from 6 to 25 mm. Hemostasis was achieved by compression in all cases. Heparin was not used for any of the cases.
Results
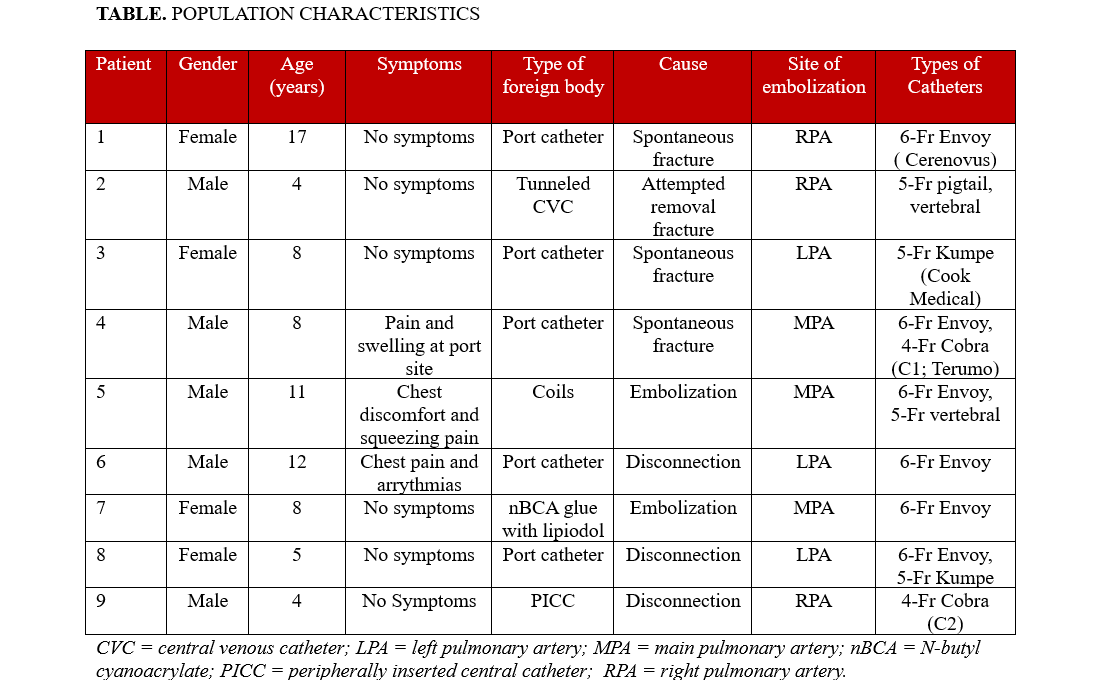
Nine patients with a mean age of 8.56 years (SD = ± 4.25 years; range, 4-17 years) were included (Table). There were 5 male and 4 female patients. We observed an equal number of cases with embolized foreign bodies in the main, left, and right pulmonary arteries (3 cases each). Foreign bodies were present for 1 day from the day of identification in 6 patients, while 3 patients had foreign bodies in place for 2, 14, and 27 days, respectively. The most common type of foreign body was a port catheter (55.6%, n = 5), followed by a central line, a peripherally inserted central catheter (PICC), coils, and N-butyl cyanoacrylate (n-BCA) glue with Lipiodol (1 case each). All (n = 5) port catheters were initially placed in the subclavian vein. Of these 5 port catheters, 4 dysfunctioned after an average of 3.2 years (SD = 1.3; range, 1.2-4.2), while 1 dysfunctioned 15 days after placement. Catheter fracture was the most common (77.8%, n=7) cause of foreign body. Most (n = 5) catheters fractured spontaneously, while 2 fractured during attempted removal. The foreign body was identified using a plain radiograph in most cases (66.7%, n = 6), followed by fluoroscopy and angiography during the procedure (11.1%, n = 1 each). The foreign bodies were successfully retrieved in all cases. In the case of the embolized coils, a femoral cutdown was also required to remove the coil mass safely.
In one of our cases, n-BCA glue mixed with Lipiodol embolized from the iliac veins to the pulmonary arteries. Stable access was established via 10- and 12-Fr Check-Flo sheaths (Cook Medical) inserted through the popliteal and femoral veins to prevent further migration. Negative pressure aspiration was initially employed to remove the glue from the femoral and iliac veins. For fragments that had traveled to the pulmonary arteries, gooseneck snares were utilized to carefully retrieve the embolized material. An aspiration catheter (Penumbra, Inc.) was employed for more resistant fragments, enabling precise and focused suction directly within the pulmonary arteries. This combination of techniques ensured the effective and safe removal of the foreign body. The estimated blood loss was 300 mL. There were no immediate complications except transient arrhythmias during 1 procedure while maneuvering the catheter across the right atrium, which resolved independently.
Discussion
The increased use of long-term central venous catheters in children and endovascular procedures has led to more intravascular foreign bodies. In their retrospective studies of PICCs in children, Chow et al reported a fracture and embolization rate of 6.7 per 1000.7 There was a significant association with the duration of catheter placement, with a mean of 93 days at the time of fracture. However, in the study of all central vein catheters in children by Cahill et al, the median duration was only 27 days. Neither study found an association between catheter size and fracture rate. In children, there is also an increased risk of fracture due to stretching of the catheter during growth.10 In addition to spontaneous fractures, catheter breakage can be seen during attempted removal.11
Prior studies have demonstrated an association between the site of vascular access and the rate of fracture.12 In particular, compression of the catheter between the clavicle and the first rib can result in pinch-off syndrome.12
The final location of the embolized fragment is based on many factors, including the access site, the size of the catheter, and flow rates.9 Embolization of the foreign body into the pulmonary arterial circulation is rare but can be associated with significant morbidity, including thrombosis and hemorrhage,6 and should be removed as soon as possible. Our study demonstrates that percutaneous pulmonary intravascular foreign body retrieval via a transcatheter approach can be safe and effective.
In most cases, ultrasound-guided puncture of the femoral vein and placement of a sheath provide the most secure method of access. The size of the sheath is determined by the diameter of the foreign body and should be sufficient to allow complete retrieval. In most cases, the retained catheter can be removed using a loop snare advanced over an angled catheter. Particular care should be taken when maneuvering through the right side of the heart. Hemostasis can be obtained by manual compression, and no prophylactic antibiotics are required.
We demonstrated that percutaneous removal of pulmonary intravascular foreign bodies in pediatric patients is highly effective, with a 100% success rate. Cahill et al13 reported a similar efficacy of 89.5% for percutaneous removal of intravascular foreign bodies in children, although these findings were not limited to pulmonary vasculature. Previous studies assessing the efficacy of intravascular foreign body retrieval in all anatomic locations have reported success rates of between 71% and 100%.13-18
In line with adult studies,19 we observed a very low complication rate. Apart from transient arrhythmias in 1 patient during the procedure, no complications were noted in any of the cases, affirming the procedure's safety in pediatric patients.
Limitations
This study does have some limitations. Since it is retrospective in design and has a relatively small sample size from a single center, it could potentially affect the generalizability of our results. Moreover, the absence of long-term follow-up limits our understanding of potential delayed complications and long-term outcomes. A prospective study with a larger sample size and long-term follow-up would be required to assess these further.
Conclusions
Percutaneous retrieval appears to be a safe and effective method of removing intra-pulmonary intravascular foreign bodies in children.
Affiliations and Disclosures
Usama Anwar, MBBS; Raja Shaikh, MBBS; Ahmad I. Alomari, MD; Horacio M. Padua, MD; Kyung R. Kim, MD; Mohammad Amarneh, MD; Gulraiz Chaudry, MBChB
From the Division of Pediatric Interventional Radiology, Boston Children’s Hospital and Harvard Medical School, Boston, Massachusetts.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Gulraiz Chaudry, MBChB, MRCP, FRCR, FSIR, Division of Interventional Radiology, Boston Children’s Hospital and Harvard Medical School, 300 Longwood Avenue, Boston, MA 02115, USA. Email: gulraiz.chaudry@childrens.harvard.edu
References
- Ciarrocchi AP, Parisi AM, Campisi A, et al. A strange case of foreign body embolism in the right lower pulmonary artery. Gen Thorac Cardiovasc Surg. 2021;69(5):894-896. doi:10.1007/s11748-020-01570-5
- De Backer A, Vanhulle A, Otten J, Deconinck P. Totally implantable central venous access devices in pediatric oncology—our experience in 46 patients. Eur J Pediatr Surg. 1993;3(2):101-106. doi:10.1055/s-2008-1063521
- Myint H, McGregor J, Edwards R, Lucie NP. Spontaneous fracture of the outlet catheter of a totally implanted catheter system (Port-A-Cath). Int J Artif Organs. 1994;17(9):505-507.
- Woodhouse JB, Uberoi R. Techniques for intravascular foreign body retrieval. Cardiovasc Intervent Radiol. 2013;36(4):888-897. doi:10.1007/s00270-012-0488-8
- Chow LM, Friedman JN, Macarthur C, et al. Peripherally inserted central catheter (PICC) fracture and embolization in the pediatric population. J Pediatr. 2003;142(2):141-144. doi:10.1067/mpd.2003.67
- Surov A, Wienke A, Carter JM, et al. Intravascular embolization of venous catheter—causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr. 2009;33(6):677-685. doi:10.1177/0148607109335121
- Motta Leal Filho JM, Carnevale FC, Nasser F, et al. Endovascular techniques and procedures, methods for removal of intravascular foreign bodies. Rev Bras Cir Cardiovasc. 2010;25(2):202-208. doi:10.1590/s0102-76382010000200012
- Tutar E, Aypar E, Atalay S, Yavuz G, Doğu F. Percutaneous transcatheter retrieval of intracardiac central venous catheter fragments in two infants using Amplatz Goose Neck snare. Turk J Pediatr. 2009;51(5):519-523.
- Pazinato LV, Leite TFO, Bortolini E, Pereira OI, Nomura CH, Motta-Leal-Filho JMD. Percutaneous retrieval of intravascular foreign body in children: a case series and review. Acta Radiol. 2022;63(5):684-691. doi:10.1177/02841851211006904
- Wang SC, Tsai CH, Hou CP, et al. Dislodgement of port-A catheters in pediatric oncology patients: 11 years of experience. World J Surg Oncol. 2013;11(1):191. doi:10.1186/1477-7819-11-191
- Duman D, Aykan HH, Ertuğrul İ, et al. Percutaneous transcatheter retrieval of central venous port fragments in pediatric patients: a single-center experience from the pediatric cardiology department. J Pediatr Hematol Oncol. 2023;45(8):e959-e965. doi:10.1097/mph.0000000000002761
- Cho JB, Park IY, Sung KY, Baek JM, Lee JH, Lee DS. Pinch-off syndrome. J Korean Surg Soc. 2013;85(3):139-144. doi:10.4174/jkss.2013.85.3.139
- Cahill AM, Ballah D, Hernandez P, Fontalvo L. Percutaneous retrieval of intravascular venous foreign bodies in children. Pediatr Radiol. 2012;42(1):24-31. doi:10.1007/s00247-011-2150-z
- Wang PC, Liang HL, Wu TH, et al. Percutaneous retrieval of dislodged central venous port catheter: experience of 25 patients in a single institute. Acta Radiol. 2009;50(1):15-20. doi:10.1080/02841850802524493
- Li Y, Chen J, Li Z, et al. Successful percutaneous transvenous retrieval of intravascular fractured port catheter: a single center experience. J Cardiothorac Surg. 2020;15(1):101. doi:10.1186/s13019-020-01131-0
- Bonvini RF, Rastan A, Sixt S, et al. Percutaneous retrieval of intravascular and intracardiac foreign bodies with a dedicated three-dimensional snare: a 3-year single center experience. Catheter Cardiovasc Interv. 2009;74(6):939-945. doi:10.1002/ccd.22074
- Thomas J, Sinclair-Smith B, Bloomfield D, Davachi A. Non-surgical retrieval of a broken segment of steel spring guide from the right atrium and inferior vena cava. Circulation. 1964;30:106-108. doi:10.1161/01.cir.30.1.106
- Iyisoy A, Kursaklioglu H, Celik T, Ors F, Yuksel UC, Demirkol S. Coronary stent embolization into right common femoral artery - the role of computed tomography angiography. Clin Cardiol. 2009;32(7):E9. doi:10.1002/clc.20094
- Leite TFO, Pazinato LV, Bortolini E, Pereira OI, Nomura CH, Filho JMDML. Endovascular removal of intravascular foreign bodies: a single-center experience and literature review. Ann Vasc Surg. 2022;82:362-376. doi:10.1016/j.avsg.2021.12.003





















