Unusual Thrombus Formation on the Eustachian Valve During Transcatheter Atrial Septal Defect Closure
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
A 64-year-old woman was referred for percutaneous closure of an atrial septal defect (ASD). The patient had a prior suspected episode of subacute myocardial ischemia, characterized by chest pain and electrocardiographic changes, albeit with normal coronary angiography. Cardiac magnetic resonance imaging revealed a right ventricular volume of 133 mL/m², without other structural abnormalities. The patient had no prior recorded history of arrhythmias but had systemic hypertension and atrial enlargement.
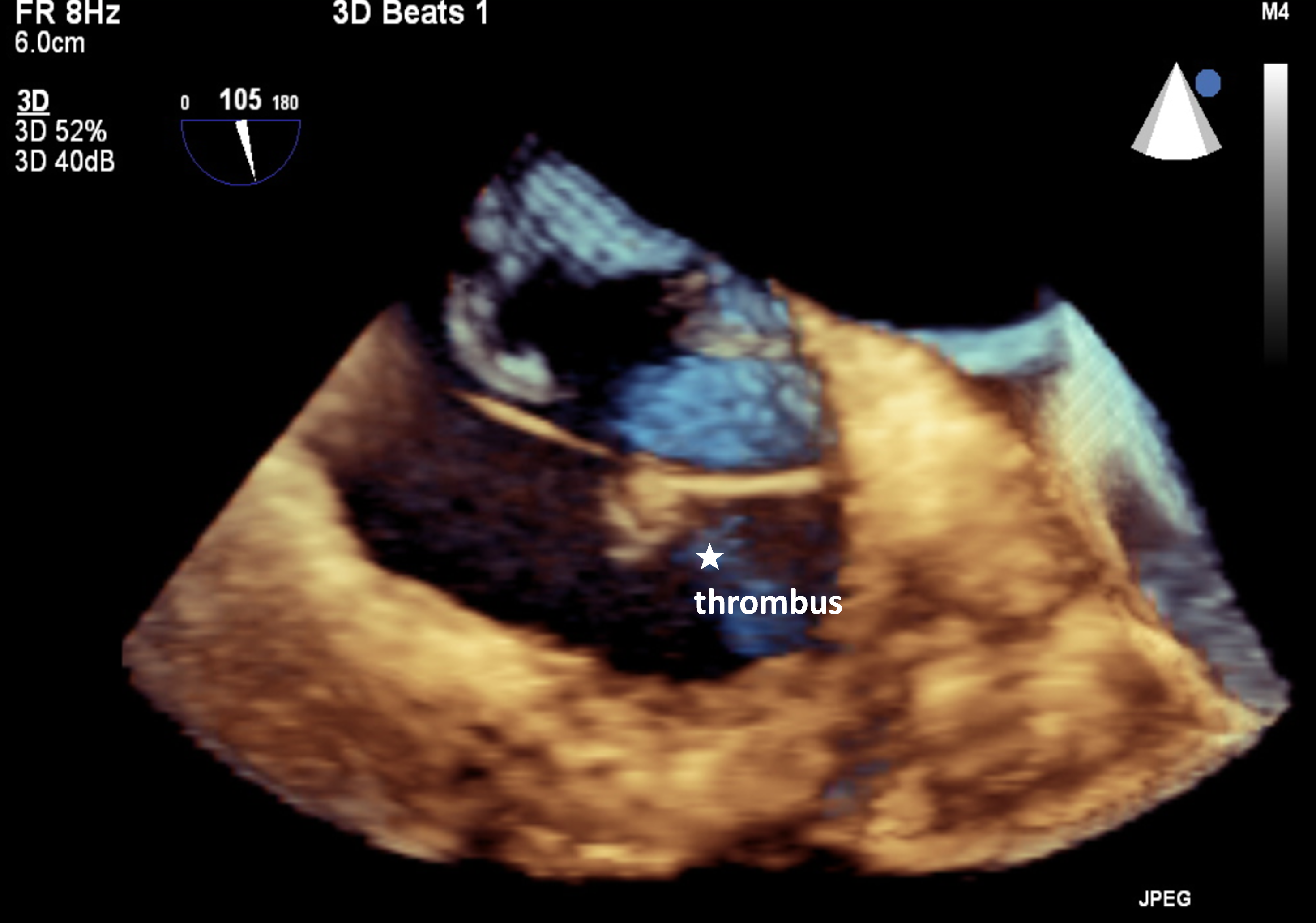
At the beginning of the procedure, the patient received unfractionated heparin and achieved an appropriate activated clotting time of 220 seconds. During right heart catheterization, the patient developed acute onset atrial fibrillation. As the catheter was advanced through the ASD, thrombotic material was suspected on 2-dimensional transesophageal echocardiography (TEE). Three-dimensional TEE confirmed the presence of a large thrombus attached to the Eustachian valve (Figure, Videos 1-3).
The procedure was discontinued, and therapeutic anticoagulation therapy was initiated with intravenous heparin. The patient was then administered 10 mg of intravenous propranolol and reverted to sinus rhythm 15 minutes later. Anticoagulation was continued with enoxaparin and warfarin on the ward. Follow-up transthoracic echocardiography performed the following day revealed complete resolution of the thrombus.
A complete thrombophilia screen was conducted, which revealed homozygous mutations for the angiotensin-converting enzyme gene and plasminogen activator inhibitor-1. Given the patient’s unusual site of thrombus formation, the decision was made to proceed with thoracoscopic ASD closure and surgical removal of the Eustachian valve. The procedure was carried out uneventfully and the patient was discharged on oral anticoagulants.

Affiliations and Disclosures
Styliani Mavrommati, MUDr1; Argyrios Krommydas, MD, MSc2; Iliona Malaspinas, PhD1; Fotios Mitropoulos, PhD3; Aphrodite Tzifa, PhD1
From the 1Pediatric Cardiology and Adult Congenital Heart Disease Department, Mitera Hospital, Athens, Greece; 2Adult Cardiology Department, Mitera Hospital, Athens, Greece; 3Department of Adult and Congenital Cardiac Surgery, Mitera Hospital, Athens, Greece.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention(s) described in the manuscript and for the publication thereof, including any and all images.
Data availability statement: The data that support the findings of this study are available on request from the corresponding author (A.T.).
Address for correspondence: Aphrodite Tzifa, PhD, Pediatric Cardiology and Adult Congenital Heart Disease Department, Mitera Hospital, 6 Erythrou Stavrou Street, Marousi 151 23, Greece. Email: atzifa@icloud.com




















