Transcatheter Closure of Ruptured Sinus of Valsalva Aneurysm Using a Ventricular Septal Defect Occluder
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
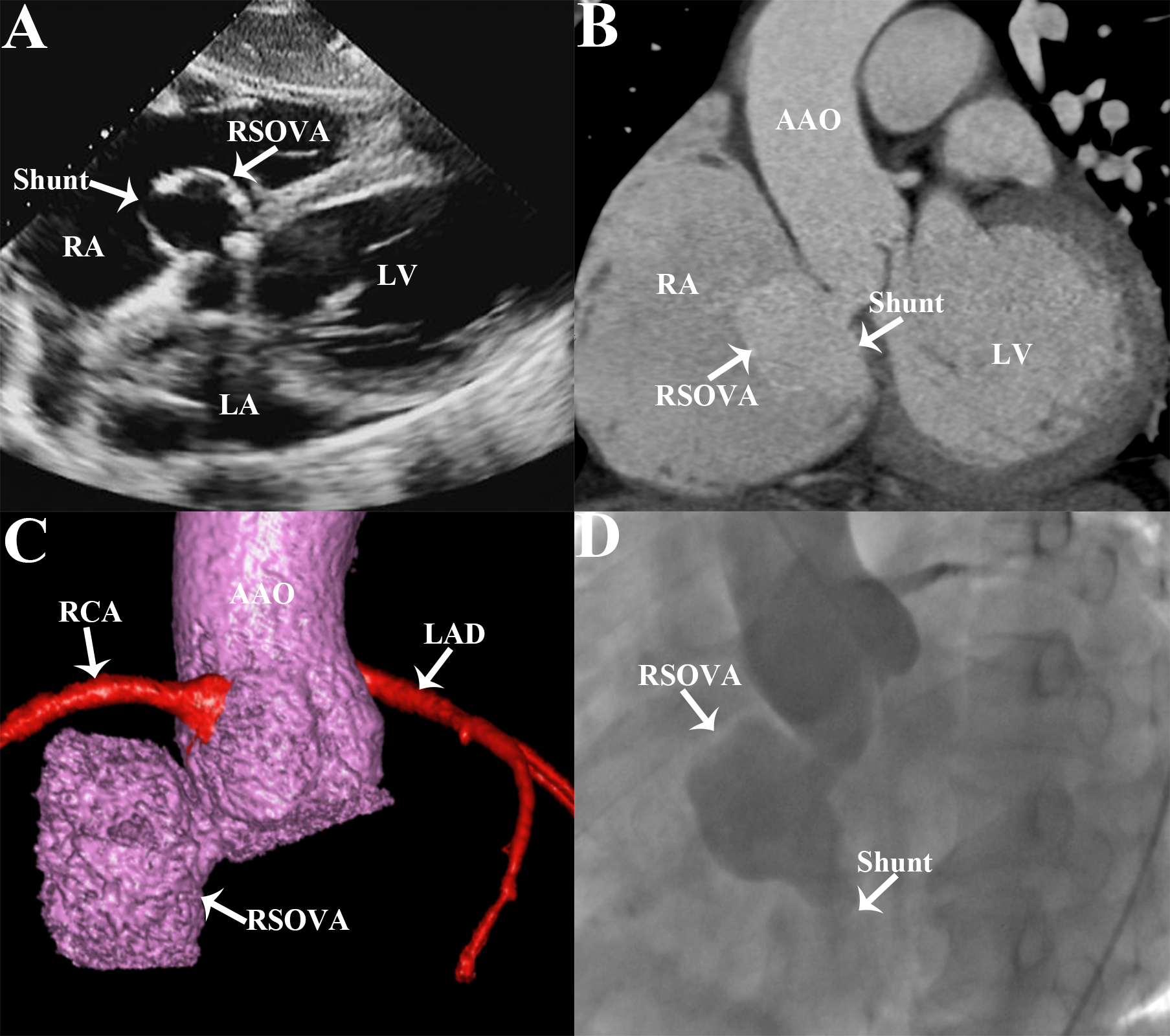
A 50-year-old man presented with chest tightness and shortness of breath after activity for 1 month. Cardiac auscultation revealed a continuous murmur in the fourth intercostal space at the right edge of the sternum. Electrocardiogram showed atrial fibrillation and delayed intraventricular conduction. Transthoracic echocardiography revealed a 32 x 31-mm sinus of Valsalva aneurysm (SOVA) arising from the non-coronary sinus that had ruptured into the right atrium (RA), leading to the formation of an aorto-right atrial shunt (Figure A), with associated mild to moderate aortic valvar regurgitation and mild mitral valve insufficiency. Cardiac computed tomographic angiography (CTA) showed the non-coronary SOVA ruptured into the RA (Figure B and C). Aortic root angiography confirmed a non-coronary SOVA rupturing into the RA with a diameter of approximately 12 mm (Figure D, Video 1).
The patient underwent transcatheter closure of the ruptured non-coronary SOVA with a 24-mm SQFDQ-II Ventricular Septal Defect Occluder (Shanghai Shape Memory Alloy Co, Ltd.). The postoperative aortic root angiography demonstrated a good device position and shape with no substantial residual shunting (Video 2). The patient was successfully discharged 3 days after the operation.
SOVA is a rare cardiovascular anomaly and may be either congenital or acquired. It is characterized by abnormal dilatation of the aortic root owing to a weak elastic lamina at the intersection of the annulus fibrosus and the aortic media.1 It is usually asymptomatic unless it compresses adjacent structures, develop thrombosis, or ruptures. A ruptured SOVA can lead to rapid hemodynamic deterioration and often requires emergency treatment.2 Multimodality imaging technology, such as transesophageal echocardiography and cardiac CTA, can help provide more extensive details of the aneurysm and its adjacent structures, especially in those considered for surgical or transcatheter closure.3 Compared with traditional surgical procedures, transcatheter interventional therapy, as a minimally invasive approach, provides a broader treatment for these diseases and prevents morbidity and mortality.
Affiliations and Disclosures
Leizhi Ku, MD1; Yuhang Wang, MD1; Zheng Liu, MD1; Xiaojing Ma, PhD2
From the Departments of 1Radiology and 2Echocardiography, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology, Wuhan, P.R. China.
Dr Ku and Dr Wang contributed equally to the article.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Funding: This work is funded by the Wuhan Clinical Medical Research Center for Cardiovascular Imaging (CMRC202307).
Consent statement: The authors confirm that informed consent was obtained from the patient for the procedures described in this manuscript.
Address for correspondence: Xiaojing Ma, PhD, Department of Echocardiography, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology. No.753 Jinghan Road, Hankou District, Wuhan 430022, P.R. China. Email: klz1534292102@163.com
References
1. English K. Diagnosis and treatment options for sinus of Valsalva aneurysms: a narrative review. World J Cardiol. 2025;17(6):102722. doi:10.4330/wjc.v17.i6.102722
2. Agrawal G, Agarwal M, Chintala K. Transcatheter closure of ruptured sinus of Valsalva aneurysm in a pregnant woman. J Cardiol Cases. 2015;12(6):183-187. doi:10.1016/j.jccase.2015.08.001
3. Barforoshi S, Sheker C, Ullal AV, Manubolu V, Budoff MJ, Roy SK. Ruptured Sinus of Valsalva aneurysm diagnosed on coronary computed tomography angiography in a patient with trisomy 13 syndrome. Tex Heart Inst J. 2023;50(3):e228022. doi:10.14503/THIJ-22-8022




















