Successful Re-endovascular Intervention of Distal Stent Graft-Induced New Entry With Endoleak After Thoracic Endovascular Aortic Repair
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
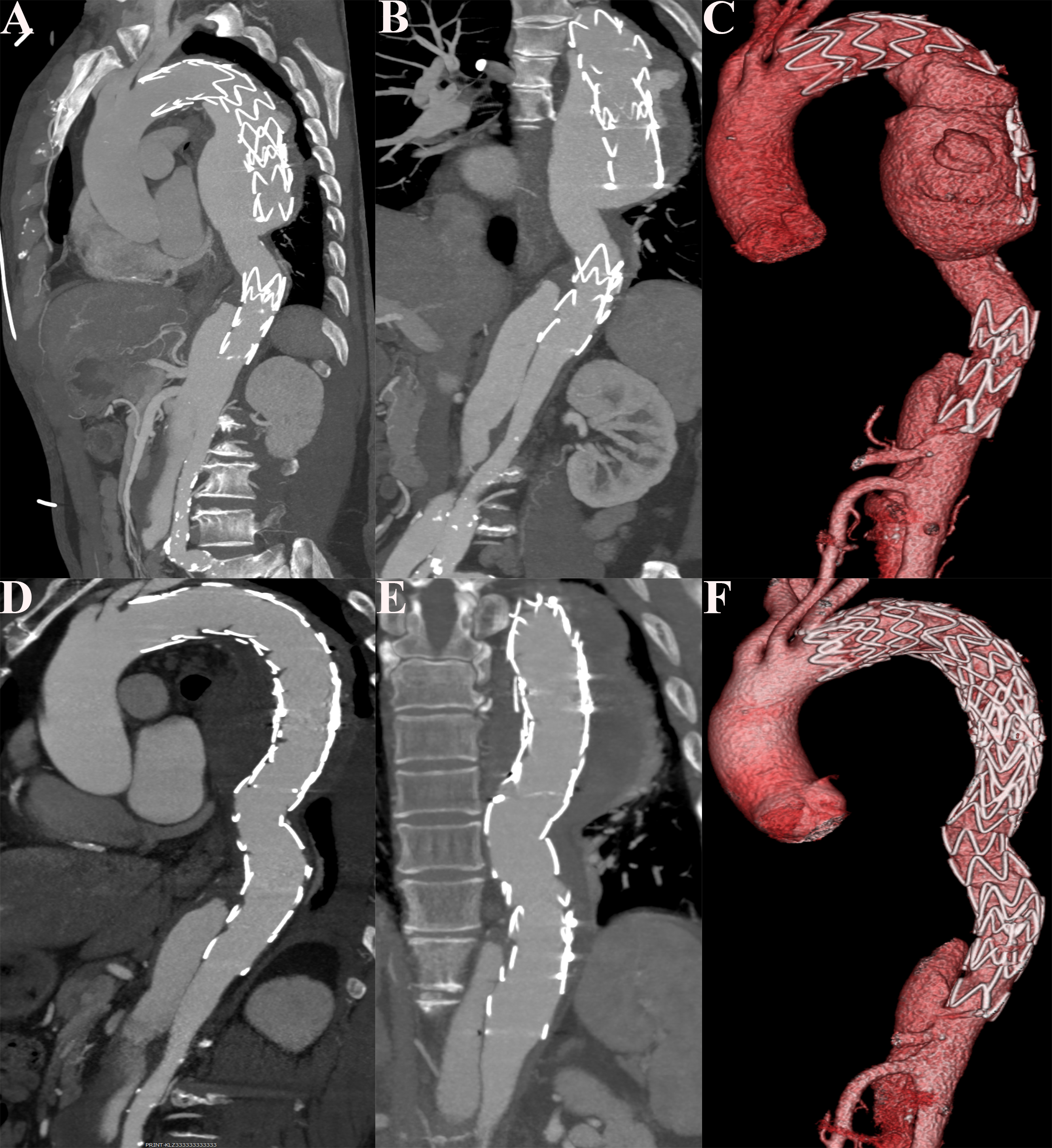
A 67-year-old man was referred to our hospital because of stent leakage after thoracic endovascular aortic repair (TEVAR) for type B aortic dissections (TBAD) 6 years ago. Computed tomographic angiography (CTA) revealed distal stent graft-induced new entry (dSINE) with endoleak (Figure A-C). Subsequently, the aortic angiography confirmed the dSINE and endoleak (Video 1).
The patient underwent re-TEVAR with 2 Valiant thoracic stent grafts (Medtronic) measuring 32 x 28 x 150 mm and 36 x 36 x 200 mm. Postoperative CTA and aortic angiography confirmed a successful repair of the dSINE and endoleak (Figure D-F, Video 2). The postoperative course was uneventful, and he was discharged after 7 days. At the 12-month postoperative follow-up, no migration, deformation, or new endovascular leakage were observed.
TBAD is a threatening event that may lead to death from aortic rupture or multivisceral malperfusion in the acute phase and offers poor prognosis for long-term survivors. TEVAR has been accepted as a standard treatment option for complicated TBAD.1 However, this less invasive procedure requires long-term surveillance for its own set of potential complications, including endoleaks, dSINE, stent migration, pseudoaneurysms, dissection, aortic perforation, kinking, thrombosis, and coverage of vital branch vessels.2 The occurrence of dSINE represents a unique complication in this scenario and may lead to high rates of aortic-related adverse events and the need for secondary interventions.3 A type III aortic arch, excessive distal oversizing and mismatch ratio, and severe angulation have been associated with dSINE.4 The risk of proximal SINE may be reduced by careful technique, minimal oversizing, and the use of disease-specific stent grafts.5
Affiliations and Disclosures
Leizhi Ku, MD1; Di Huang, MD1; Xiaojing Ma, PhD2
From the Departments of 1Radiology and 2Echocardiography, Wuhan Asia Heart Hospital, Wuhan University of Science and Technology, Wuhan, P.R. China.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Funding: This work is funded by the Wuhan Clinical Medical Research Center for Cardiovascular Imaging (CMRC202307).
Consent statement: The authors confirm that informed consent was obtained from the patient for the procedures described in this manuscript.
Address for correspondence: Xiaojing Ma, PhD, Wuhan Asia Heart Hospital, Wuhan University of Science and Technology, No.753 Jinghan Road, Hankou District, Wuhan 430022, P.R. China. Email: klz1534292102@163.com; X: @klz13657254286
References
1. Lovato L, Cefarelli M, Gatta E, Di Eusanio M, Fattori R. Devices for thoracic endovascular aortic repair of type B aortic dissection: is there any chance for Marfan syndrome? Expert Rev Med Devices. 2020;17(7):683-696. doi:10.1080/17434440.2020.1782735
2. Hiatt MD, Rubin GD. Surveillance for endoleaks: how to detect all of them. Semin Vasc Surg. 2004;17(4):268-278. doi:10.1053/j.semvascsurg.2004.09.003
3. D'Oria M, Wanhainen A, Kolbel T, Yoon W, Mani K. Novel insights into thoracic endografts technology for prevention of distal stent-graft induced new entry (dSINE) following endovascular repair of type B aortic dissections: from bench to bedside. Expert Rev Med Devices. 2024;21(5):391-398. doi:10.1080/17434440.2024.2343824
4. Xiang D, Chai B, Gui Y, et al. Risk factors for distal stent graft-induced new entry after endovascular repair in uncomplicated type B aortic dissection. J Vasc Surg. 2023;77(1):37-45.e1. doi:10.1016/j.jvs.2022.08.032
5. Burdess A, Mani K, Tegler G, Wanhainen A. Stent-graft induced new entry tears after type B aortic dissection: how to treat and how to prevent? J Cardiovasc Surg (Torino). 2018;59(6):789-796. doi:10.23736/S0021-9509.18.10570-2




















