A Rare Cause of Cyanosis in a Structurally Normal Heart
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00237. Epub August 21, 2025.
A 24-year-old man presented with central cyanosis and dyspnea on exertion for the past 2 years. He had no history of epistaxis, melaena, neurological deficit, or congenital heart defect. He had grade 3 clubbing on examination; auscultation revealed a pulmonary vascular bruit.
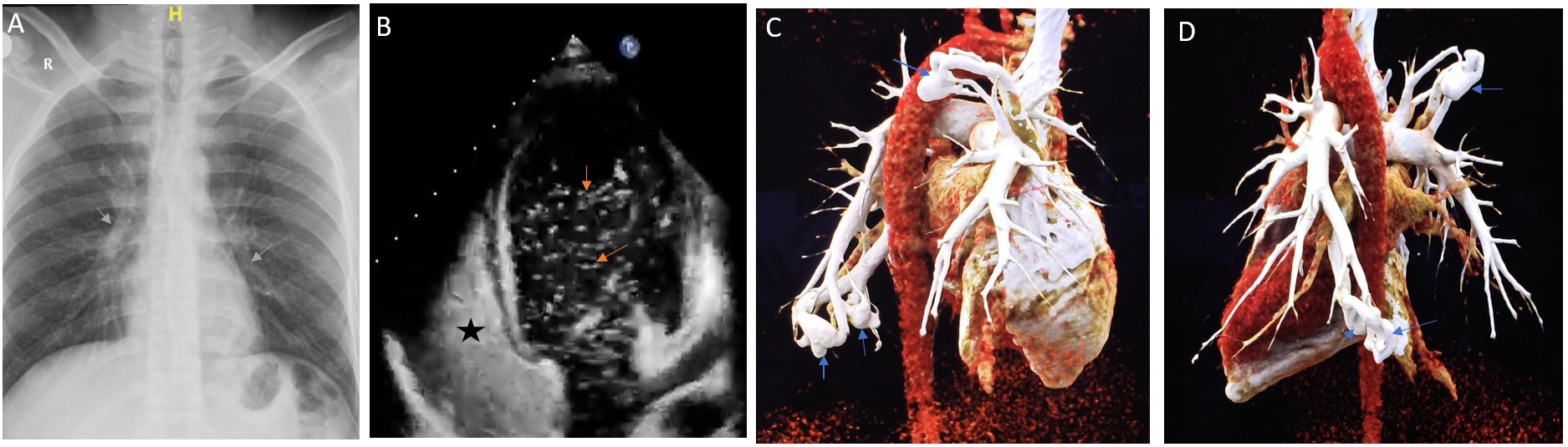
Chest x-ray revealed soft tissue masses in the right upper and left lower lung zones (Figure A, gray arrows). Transthoracic echocardiography revealed normal biventricular function with no shunt lesion. After 3 cardiac cycles, contrast saline echocardiography showed bubbles (Figure B, orange arrows) in the left-sided chambers, which raised suspicion of a pulmonary arteriovenous malformation (PAVM) (Figure B, the black asterisk represents dense bubble contrast in the right atrium [RA] and right ventricle [RV]; Video 1). Pulmonary computed tomography angiography with 3-dimensional reconstruction confirmed the presence of 3 PAVMs: 2 in the left lower lobe (19 x 15 mm and 7 x 5 mm) and 1 in the right upper lobe (20 x 15 mm) (Figure C and D, blue arrows). Genetic testing for hereditary hemorrhagic telangiectasia was negative.
Because the patient was symptomatic, and all 3 PAVMs were simple in morphology and amenable for device closure, we proceeded with coil embolization. An 8F right femoral venous access was taken. A 100-cm 7F multipurpose A1 guide catheter was used to enter the pulmonary artery over a Terumo guidewire by sequentially passing through the inferior vena cava, RA, RV, and pulmonary artery.
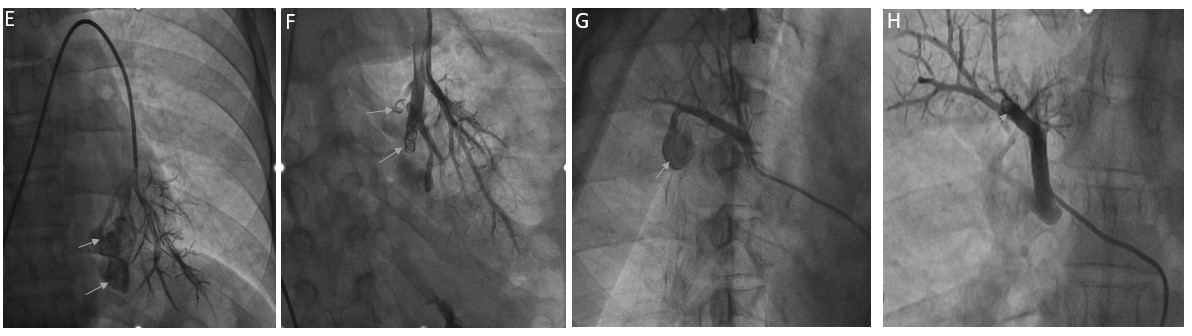
Invasive angiography delineated the PAVMs in the right upper lobe (Figure G; Video 2) and left lower lobe (Figure E; Video 3). The multipurpose catheter was used in combination with a 120-cm 5F Heartrail ST01 catheter (Terumo) as a mother-and-child technique to engage the PAVMs. Hydrogel-coated 0.018-inch pushable coils were used to occlude the PAVMs using the anchor technique. Five coils were used on the left side (Figure F, gray arrow) and 1 coil on the right side (Figure H, gray arrow), which led to complete occlusion of the PAVMs and improvement in saturation and symptoms (Videos 4 and 5).
As of 2 years post-procedure, the patient was doing well at regular follow-up with no recurrence.
Affiliations and Disclosures
Krishna Prasad Akkineni, MD, DM1; Souvik Sardar, MD, DM2; Goutam Kintada, MD, DM3; Devesh Kumar, MD, DM4; Aseem Basha, MD, DM5
From the 1Department of Cardiology, Apollo Hospitals, Hyderabad, India; 2Department of Cardiology, Manorama Hospitex, Kolkata, India; 3Department of Cardiology, Devender Reddy Super Specialty Hospital, Nirmal, India; 4Department of Cardiology, Safdarjung Hospital, Delhi, India; 5Department of Cardiology, AIIMS New Delhi, India.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication thereof, including photographs.
Address for correspondence: Aseem Basha, MD, DM, Department of Cardiology, All India Institute of Medical Sciences, New Delhi 110029, India. Email: draseembasha@gmail.com




















