Opening the Way! Fenestration of a Malpositioned Ostial Right Coronary Artery Stent
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
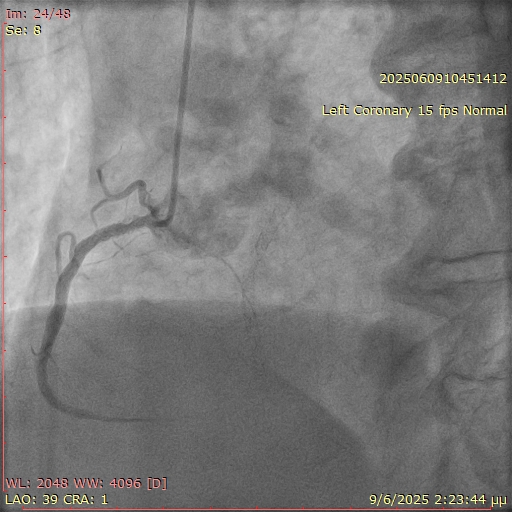
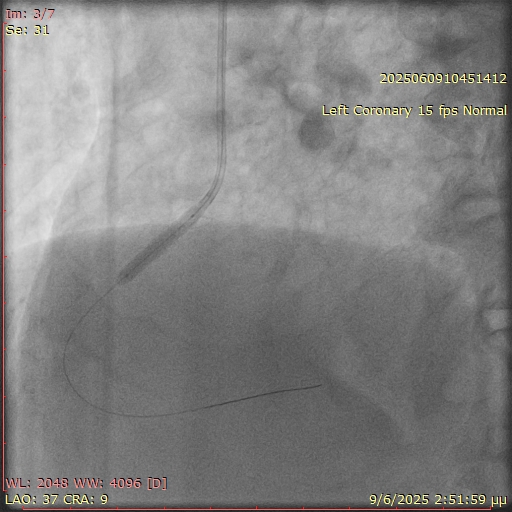
A 67-year-old man with a history of coronary artery disease and prior percutaneous coronary interventions (PCI) of the left anterior descending artery and the right coronary artery (RCA) presented with stable angina. During diagnostic coronary angiography, selective engagement of the RCA using a 5F Judkins right (JR) 4 catheter proved challenging (Figure 1). However, angiographic signs suggested significant restenosis at the ostium and proximal RCA. PCI was initiated using a 6F JR 4 guiding catheter; operators employed the "floating wire" technique, maintaining the wire at the catheter tip until ostial engagement was achieved. After several attempts, the wire was successfully advanced distally into the RCA.
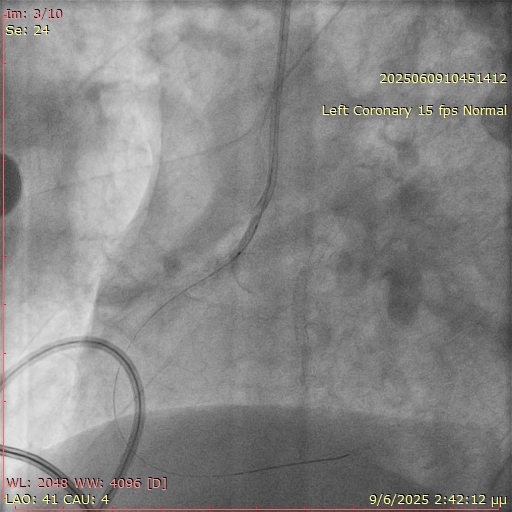
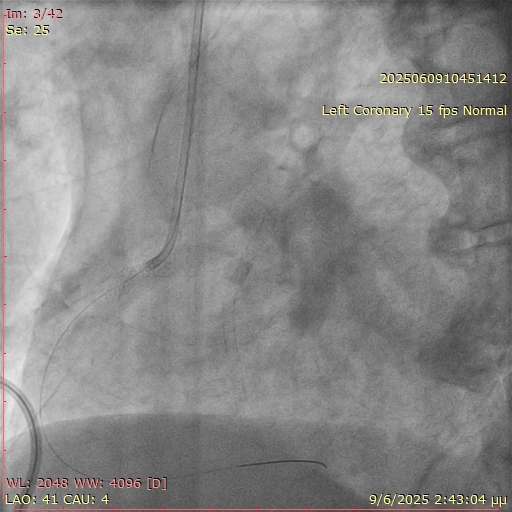
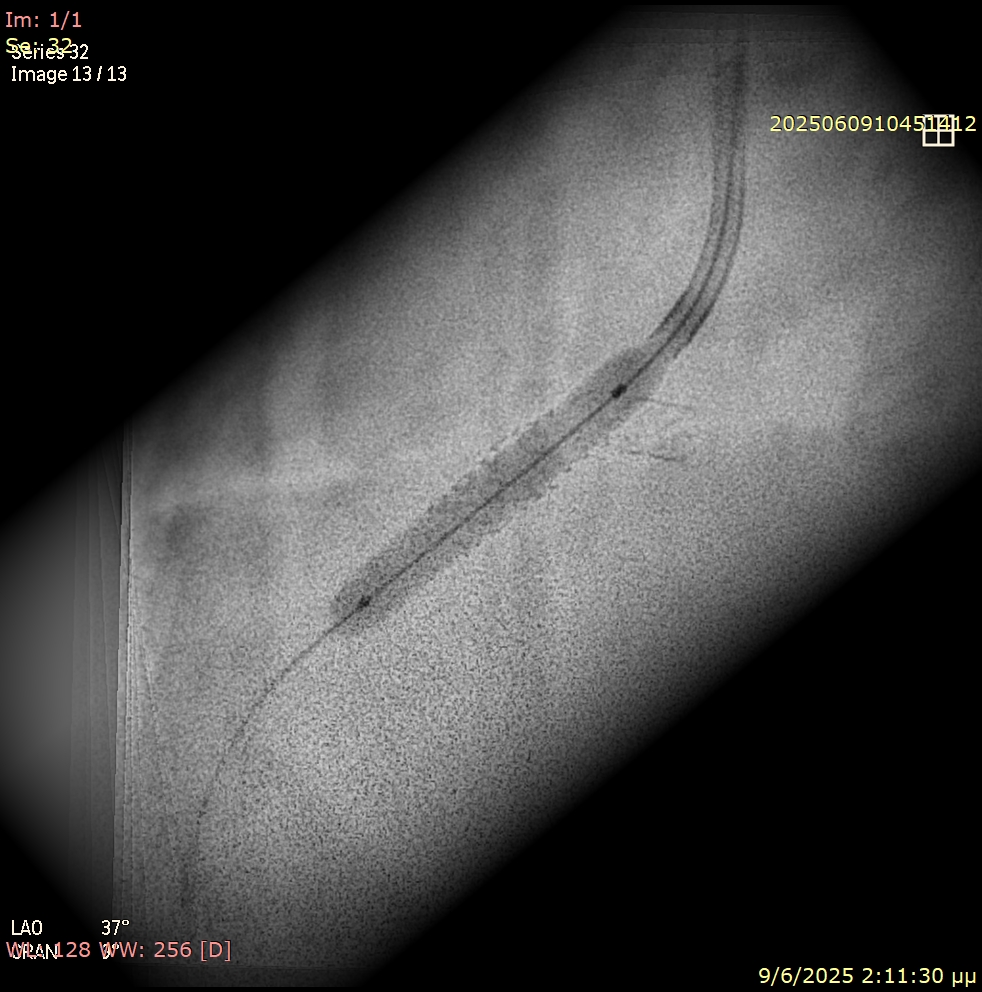
Unexpected resistance was encountered while attempting to deliver balloons across the ostial segment (Figure 2). Suspecting an underlying issue, the angiographic projection was modified to a more cranial view. This revealed that a significant portion of the prior stent was protruding into the aorta, obstructing device passage (Figure 3).
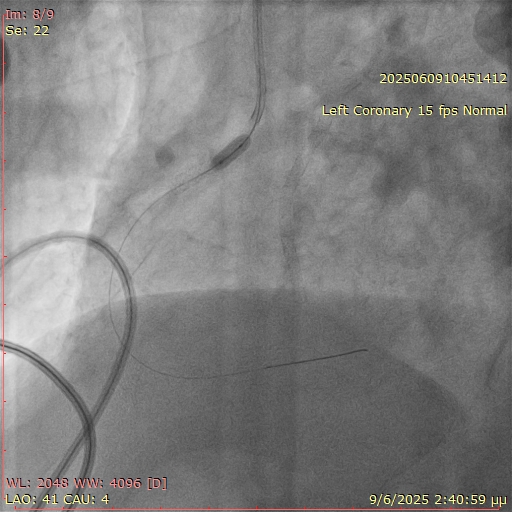
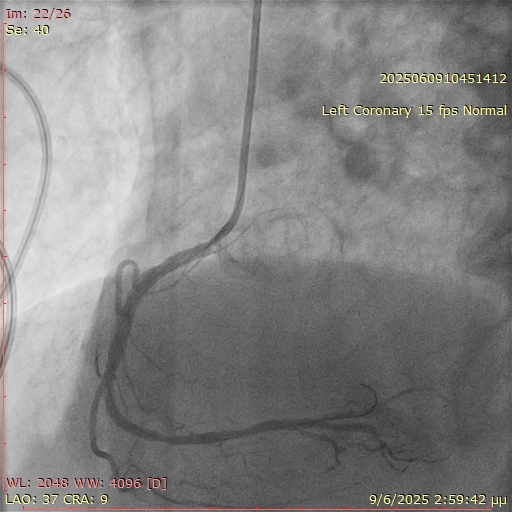
Using progressive balloon dilatation (non-compliant 3.0 x 15 mm, 3.5 x 15 mm, and 4.0 x 15 mm) followed by a 3.5 x 10-mm scoring balloon (Figure 4), we successfully fenestrated the stent strut. To avoid placing a second metal layer at the ostium and prevent double stenting, we concluded the procedure with a 3.5 x 20-mm paclitaxel-coated balloon (Figures 5 and 6, Video). The final result was good, with Thrombolysis in Myocardial Infarction-III flow (Figure 7). Dual antiplatelet therapy (DAPT) with aspirin 100 mg once daily and clopidogrel once daily was prescribed to the patient. Given the low bleeding risk based on the PRECISE-DAPT score and the assumption that forming a fenestration at the upper part of the stent would place the patient at high ischemic risk, we decided to continue the duration of DAPT beyond 1 year.
The patient remained asymptomatic at the 3-month follow-up, demonstrating that selective fenestration combined with drug-coated balloon therapy can be an effective and elegant solution in complex ostial stent malpositions.
Affiliations and Disclosures
Konstantinos Filippou, MD; Konstantinos Manousopoulos, MD, PhD; Panagiotis Varelas, MD; Dimitrios Karelas, MD; Ioannis Papadopoulos, MD; Ioannis Tsiafoutis, MD, PhD
From the Hemodynamic Laboratory, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, Athens, Greece.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication of thereof, including any and all images.
Address for correspondence: Konstantinos Filippou, MD, Hemodynamic Department, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, 11145 Nikolaidou Street, Athens 11526, Greece. Email: filippakos.kos@gmail.com




















