Familial Hypercholesteremia With Left Main Ostial Disease in a Young Male
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
A 14-year-old boy presented to the emergency department with classical angina, described as retrosternal chest pain occurring with minimal exertion. He had been experiencing New York Heart Association (NYHA) Class II symptoms for the past year, which had progressed to NYHA Class III over the last 2 months.
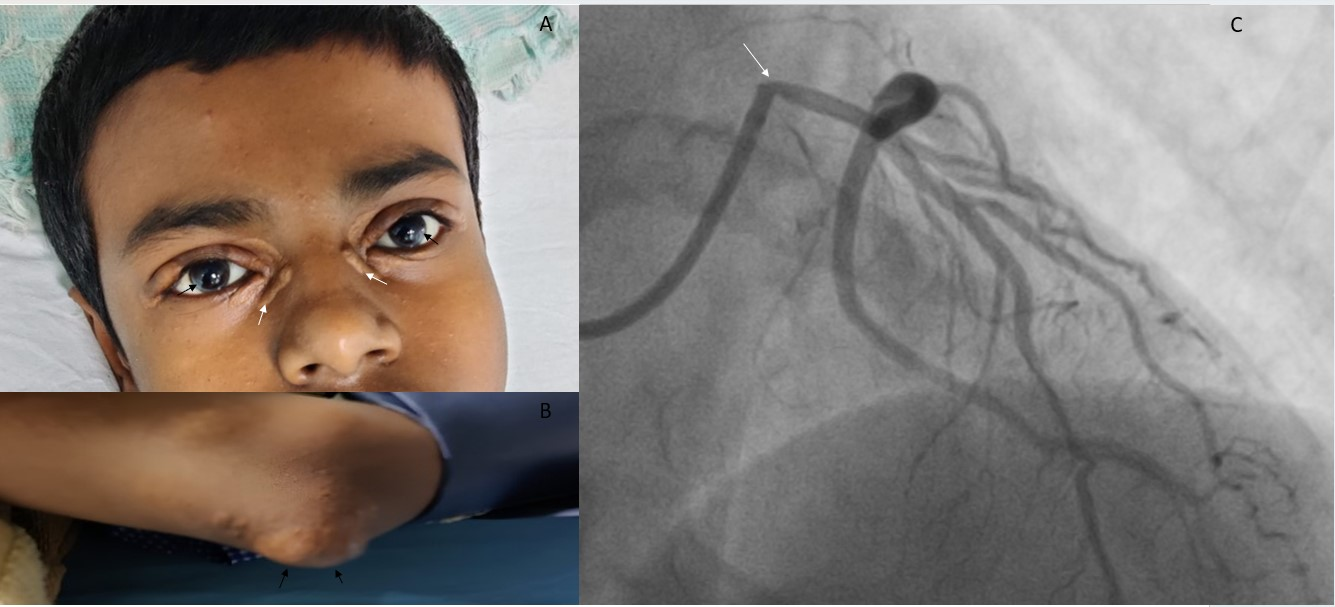
Upon examination, the patient had bilateral arcus juvenilis—a circumferential thin white ring within the corneal border (Figure A, black arrows). Facial inspection revealed multiple xanthelasmas around the eyes (Figure A, white arrows). In addition, a tendon xanthoma was noted over the olecranon process of the right elbow (Figure B, black arrows).
His total cholesterol level was 600 mg/dL (reference range: < 200 mg/dL), high-density lipoprotein was 30 mg/dL (reference range: 35-60 mg/dL), low-density lipoprotein (LDL) was 470 mg/dL (reference range: < 100 mg/dL), and triglycerides were 300 mg/dL (reference range: < 150 mg/dL). Genetic testing revealed a homozygous mutation in the LDL receptor gene. He was diagnosed with familial hypercholesteremia according to the Dutch Lipid Clinic Network criteria. Cascade screening was offered to his first-degree relatives.
Given the presence of typical anginal symptoms and confirmed familial hypercholesterolemia, coronary angiography was performed, which revealed tight ostial stenosis of the left main coronary artery (Figure C, white arrow). Ostial coronary involvement is a characteristic finding in patients with familial hypercholesterolemia.
Revascularization was advised; however, the patient's parents declined and opted for medical management. He was started on high-dose statins, ezetimibe, and evolocumab, in addition to aspirin and nitrates. He was doing well on regular follow-up during the first year posttreatment, with significant improvement in symptoms from NYHA Class III to NYHA Class II.
Affiliations and Disclosures
Krishna Prasad Akkineni, MD, DM1; Mohan Prasad Akkineni, MD2; Maithili Charan Gattu, MD3; Goutam Kintada, MD, DM4; Souvik Sardar, MD, DM4
From the 1Department of Cardiology, Krishna Heart and General Hospital, Jaipur, India; 2Department of Cardiology, Post Graduate Institute of Medical Education and Research, Chandigarh, India; 3Department of Emergency Medicine, All India Institute of Medical Sciences, New Delhi, India; 4Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication thereof, including photographs.
Address for correspondence: Krishna Prasad Akkineni, MD, DM, Room number 1, First Floor, Krishna Heart and General Hospital, Jaipur, India. Email: ramuchinnu92@gmail.com




















