Extensive Coronary Artery Vasospasm Due to Exercise and Cold Exposure
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
We present an interesting and rare example of the similarity of coronary vasospasm developing after intense exercise to severe atherosclerotic stenosis to draw attention to the possible consequences of misdiagnosis.
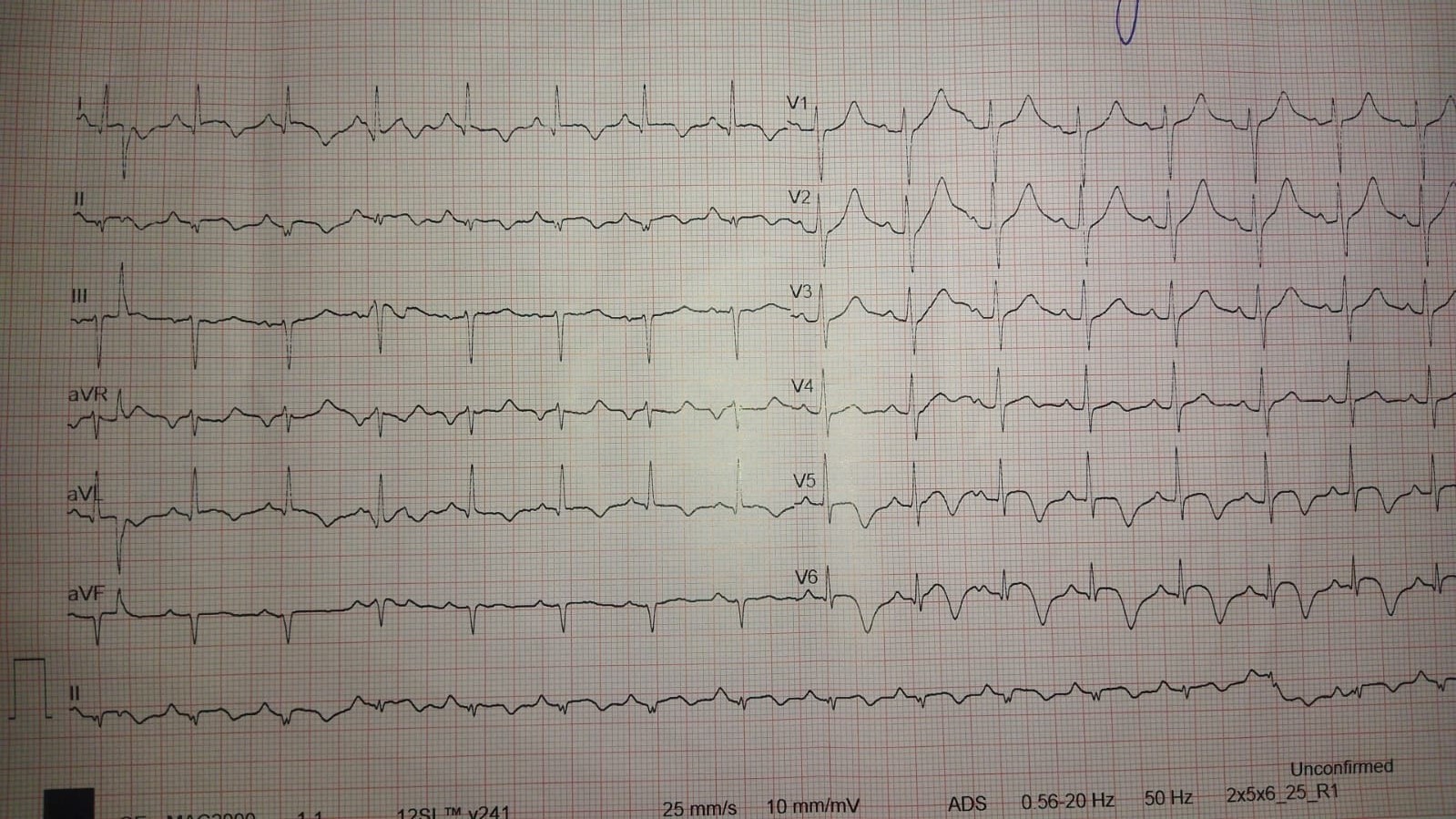
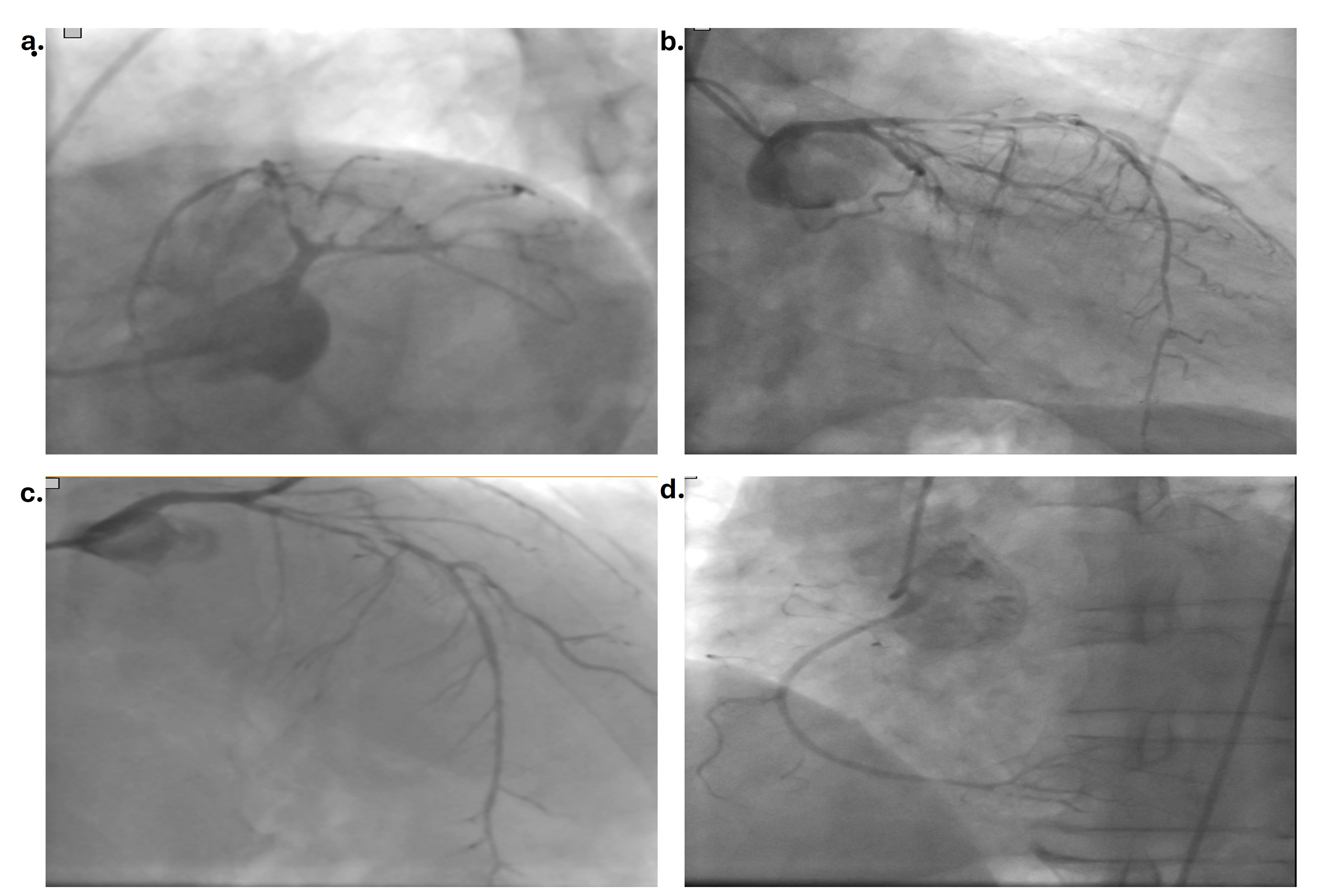
A 48-year-old man was admitted to the emergency department with chest pain after intense exercise in cold weather. There was no risk factor other than a history of hypertension. There was no history of smoking, alcohol, drug or substance use. Physical examination was normal. Electrocardiography (ECG) showed T inversion in the anterior, lateral and inferior leads with sinus rhythm (Figure 1). There were no abnormalities in the blood values other than elevated cardiac troponin I (cTnI 1100 ng/mL). Echocardiography revealed an ejection fraction of 42% and inferior, posterior, and lateral wall hypokinesis. Diagnostic coronary angiography revealed a 90% diffuse long stenosis in the proximal left anterior descending artery (LAD), subtotal stenosis in the mid-circumflex artery (Cx), and 99% stenosis in the first obtuse marginal artery and the normal right coronary artery (Figure 2, Video 1).
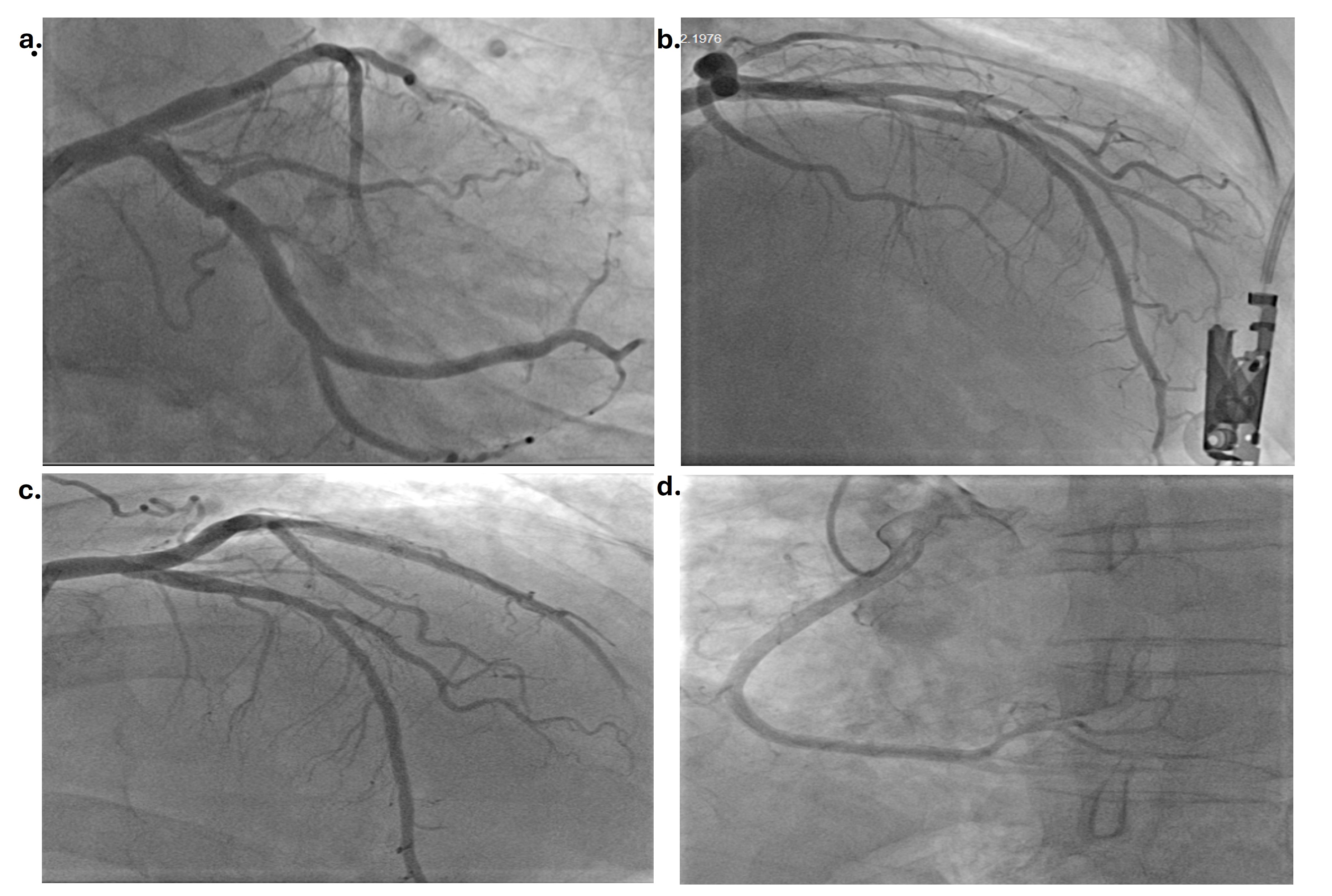
The patient was offered bypass surgery at another hospital and, after he refused, was admitted to our hospital. The patient received intravenous nitrate therapy for 4 to 6 hours after coronary angiography. He was also receiving atorvastatin, acetylsalicylic acid, metoprolol, perindopril, and enoxaparin therapy. The patient again did not accept bypass surgery; however, 48 hours later, he agreed to undergo coronary angiography for percutaneous intervention. Coronary angiography showed no critical stenosis in the LAD or Cx. There was only plaque in the LAD, and medical follow-up was planned (Figure 3) (Video 2). His cTnI value increased to 3600 ng/mL and dropped to 1000 ng/mL before discharge. There was no change in the ECG (Video 3). The patient was questioned again about drug or substance use, but he stated that he had not used anything. The blood or urine tests were not performed for substance use. The patient was discharged with atorvastatin, acetylsalicylic acid, clopidogrel, amlodipine, perindopril, and nebivolol therapy.
Coronary artery vasospasm is described as temporary increased contractile tonus with vagal withdrawal and sympathetic activity fluctuation, resulting in chest pain. Patients may be admitted with anginal pain with dynamic ECG changes, but rarely with ST-segment elevation or non-ST-segment elevation myocardial infarction, malign ventricular arrhythmias, or sudden cardiac death. Diagnosis can be made based on the anginal chest pain response to nitrates or calcium channel blockers, ST-segment and T-wave changes on ECG, and angiographic evidence of coronary vasospasm. Different stimulant agents such as hyperventilation, cold pressor test, acetylcholine, and ergonovine have been shown to provoke coronary spasm on the coronary angiography. The positive response is defined as an at least 50% luminal obstruction at the coronary artery; this is reversed with intracoronary nitroglycerin. Coronary vasospasm may occur in up to 60% of cases with atherosclerotic stenosis without normal coronary arteries. The first line therapies are addressing the risk factors and lifestyle modifications such as quitting smoking, and avoiding triggering factors such as cold, exercise, or some medications.
It is important that coronary vasospasm be considered, especially in cases with long diffuse and smooth-walled stenoses, and angiographic images should be repeated after intracoronary nitroglycerin. Any evidence of thrombus, recent plaque rupture, or erosion should be clarified with different imaging modalities, especially intravascular ultrasound.
Affiliations and Disclosures
Murat Akçay, MD; Muhammed Cemallioglu, MD; Esra Temiz Lafci, MD
From the Department of Cardiology, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey.
Disclosures: The authors report no financial relationshps or conflicts of interest regarding the content herein.
Consent statement: Written informed consent was obtained from the patient for publication of this case report.
Artificial intelligence (AI) statement: The authors did not use any AI-assisted technologies (such as large language models, chatbots, or image creators) in the production of submitted work.
Address for correspondence: Murat Akçay, MD, Department of Cardology, Ondokuz Mays University, 55270 Atakum, Samsun, Turkey. Email: drmuratakcay@hotmail.com




















