Counterproductive Counterpulsation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
An 80-year-old woman with severe aortic stenosis, end-stage renal disease with a poorly functional left forearm arteriovenous fistula (flow 132-336 mL/min; normal 500-1500 mL/min), and a recently placed right internal jugular vein tunneled dialysis catheter presented with chest pain, shortness of breath, new left bundle branch block, and hypotension (87/51 mm Hg). Her labs were notable for a high-sensitivity troponin level greater than 60 000 ng/L, (normal: < 52 ng/L), a white blood cell count of 18 000 (normal: 4.00-11.00 x10(9)/L), and a lactate level of 3.0 (normal: 0.5-2.2 mmol/L).
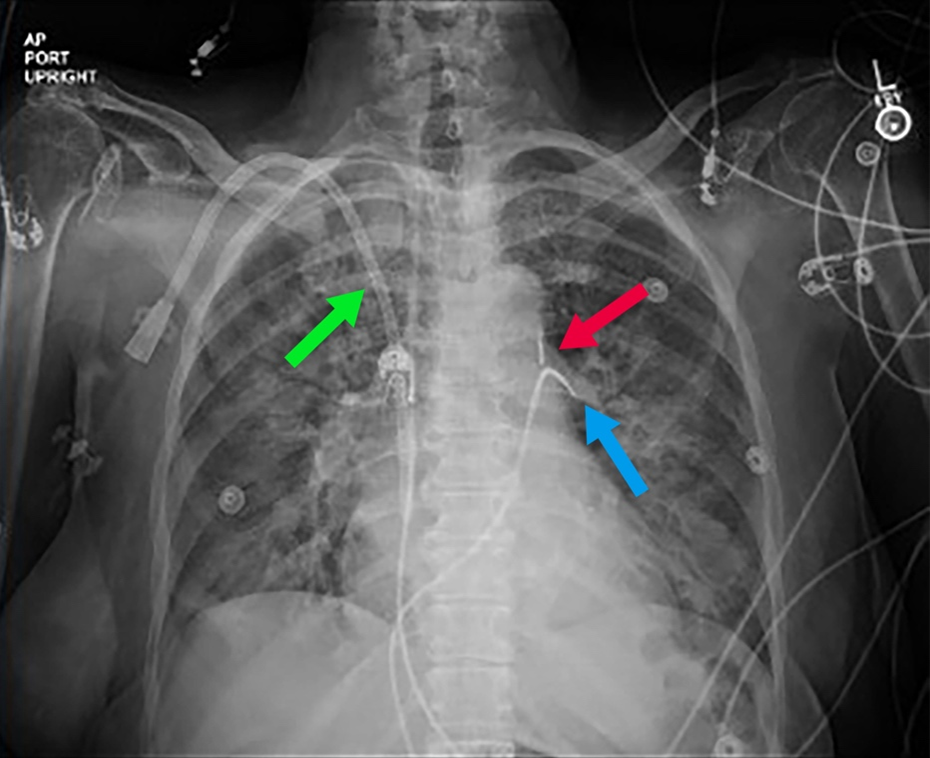
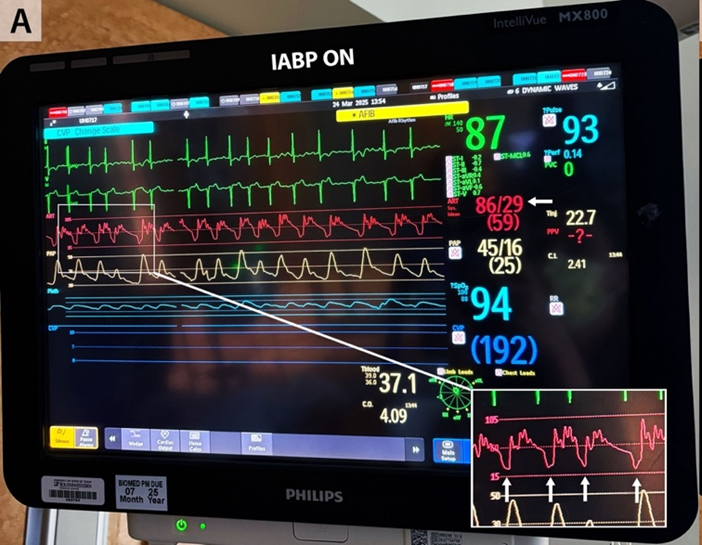
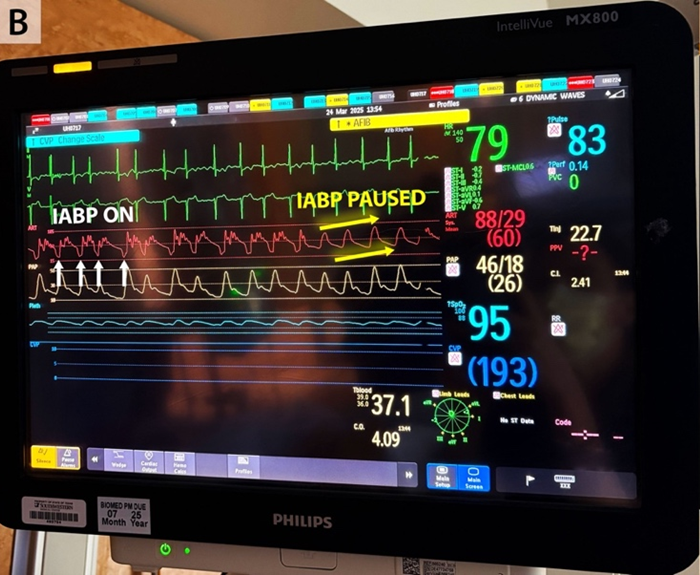
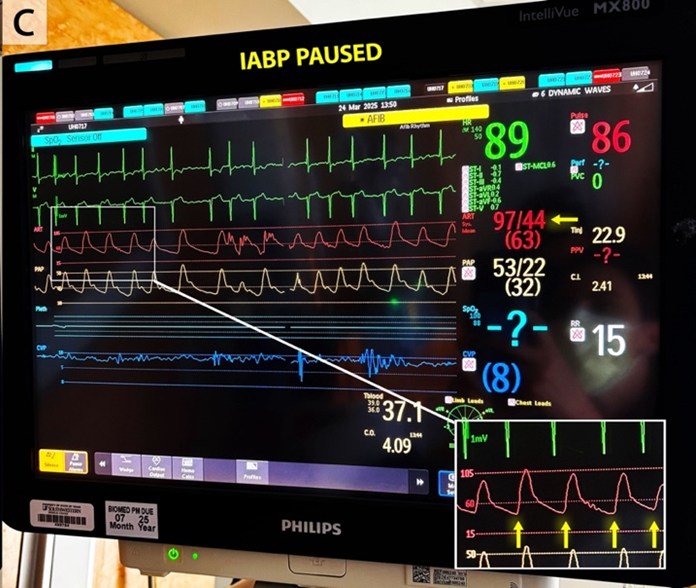
Urgent coronary angiography showed severe 3-vessel disease with 80% to 90% ostial left main and mid-left anterior descending stenosis. The left ventricular end-diastolic pressure was 20 mm Hg. A 40-cc intra-aortic balloon pump (IABP) was placed for hemodynamic support (Figure 1) and percutaneous coronary intervention was performed. Hypotension and vasopressor requirement persisted despite counterpulsation. The indirect Fick cardiac index was 3.6 L/min/m2 with a calculated systemic vascular resistance of 593 dyne-sec-cm-5. Close inspection of the arterial pressure tracing showed an unusually low assisted end-diastolic pressure of 29 mm Hg with substantial improvement when counterpulsation was paused (Figure 2). Echocardiography confirmed normal biventricular systolic function and excluded pericardial effusion and aortic regurgitation. Liver imaging and cortisol level were normal, and a bedside arteriovenous fistula occlusion test did not result in an increase in blood pressure.
Empiric antibiotics were initiated. Subsequently, blood cultures returned positive for Staphylococcus aureus, and the dialysis catheter was removed. Because counterpulsation was hemodynamically counterproductive by worsening hypotension, the IABP was removed, and vasopressor requirements diminished. Further investigation into persistently positive blood cultures revealed likely septic thrombophlebitis involving the right-sided central veins (internal jugular, subclavian, superior vena cava) in addition to aortic root abscess, L1-L5 osteomyelitis with epidural phlegmon, and psoas muscle abscess.
This case underscores the importance of integrating all bedside data, including the IABP waveform, to accurately diagnose shock etiology and tailor management. Further, it highlights that in patients with septic shock, counterpulsation can be counterproductive from a hemodynamic standpoint possibly because of an underlying vasodilatory state, an observation that to our knowledge has not previously been reported.
Affiliations and Disclosures
Michelle Dimza, DO; Omowunmi Adedeji, MD; Mark H. Drazner, MD, MSc; Faris G. Araj, MD
From the Division of Cardiology, Department of Internal Medicine, The University of Texas Southwestern Medical Center, Dallas, Texas.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication thereof, including any and all images.
Address for correspondence: Faris G. Araj, MD, Professional Office Bldg. 2, Suite 600, 5939 Harry Hines Blvd, Dallas, TX 75390-9252, USA. Email: faris.araj@utsouthwestern.edu




















