Blocked: A Curious Case of Recurrent Syncope Following Coronary Intervention
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00281. Epub October 3, 2025.
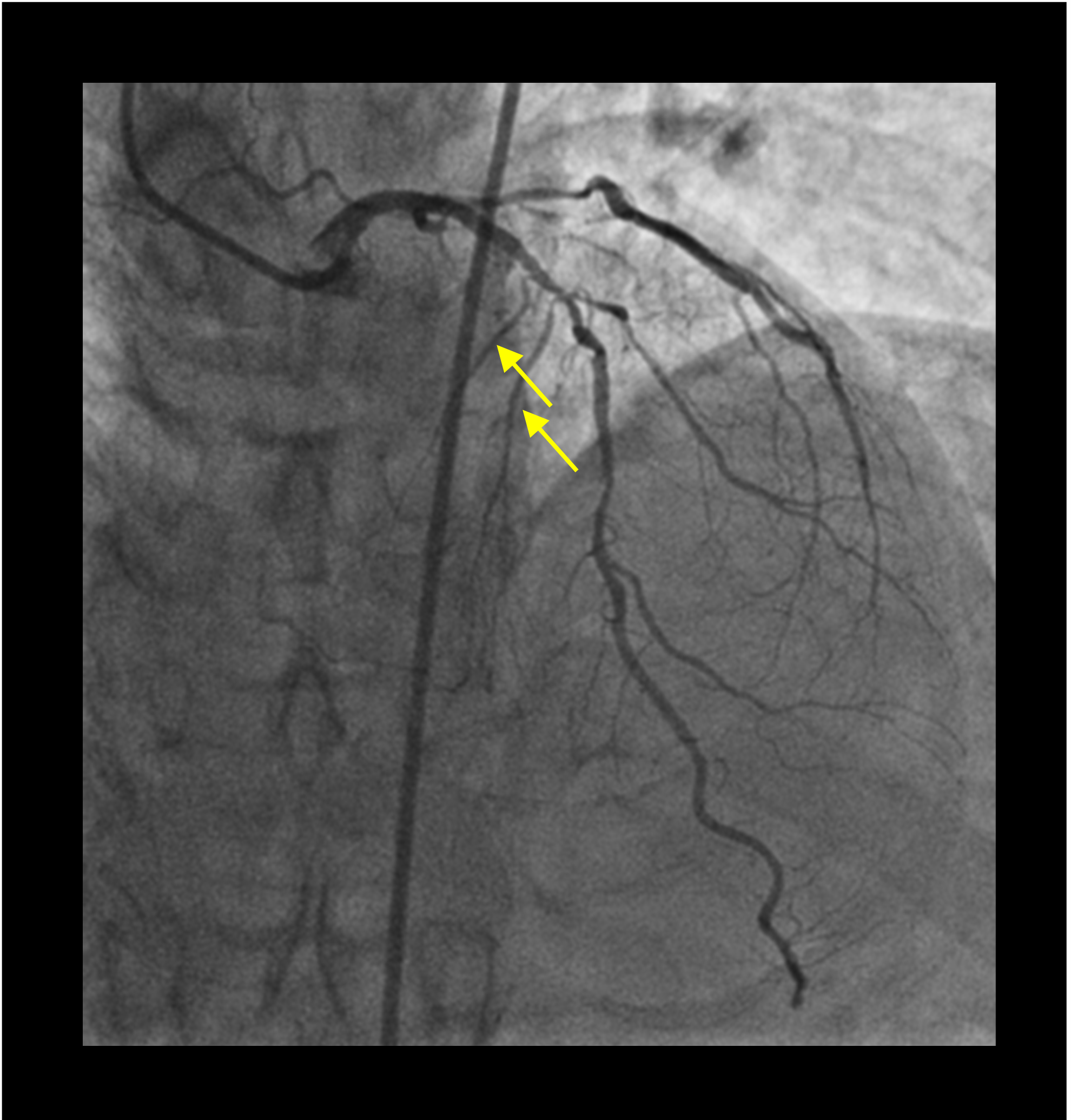
A 58-year-old man with a prior history of poorly controlled type 2 diabetes mellitus presented with a high-risk non-ST elevation myocardial infarction. Transthoracic echocardiography demonstrated a left ventricular ejection fraction of 51% with hypokinesia of the basal anteroseptal and anterior wall. An urgent coronary angiogram demonstrated diffuse calcific disease of the proximal to mid-segment of the left anterior descending (LAD) artery, with a bifurcation lesion at the level of the first diagonal branch (Medina 1,1,1). The left circumflex artery appeared chronically occluded, and a dominant right coronary artery (RCA) had tandem, tubular, angiographically significant lesions (Figure 1).
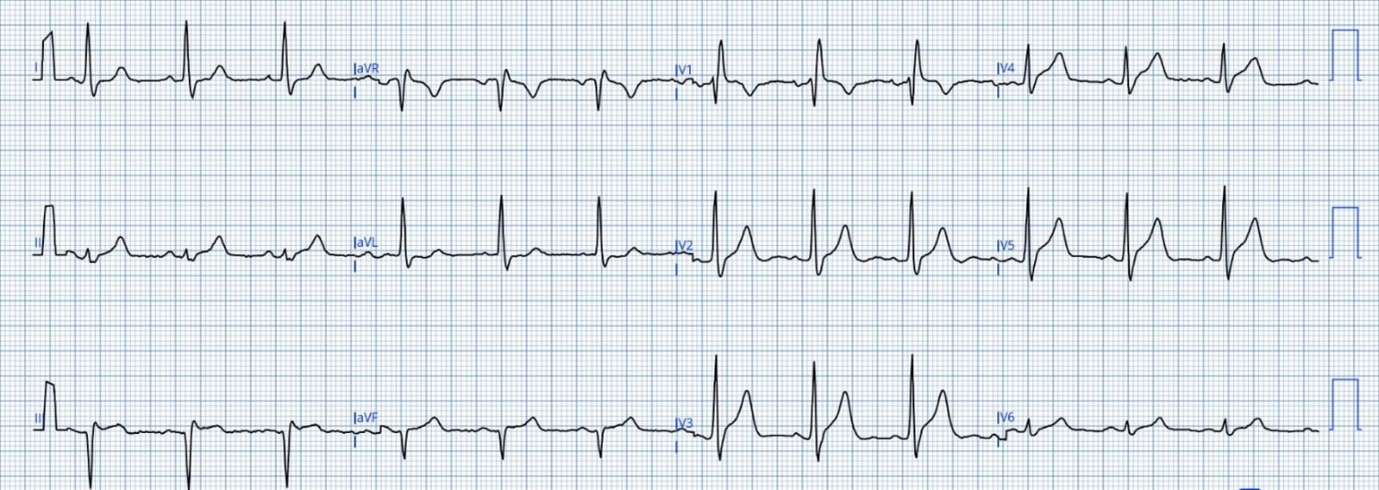
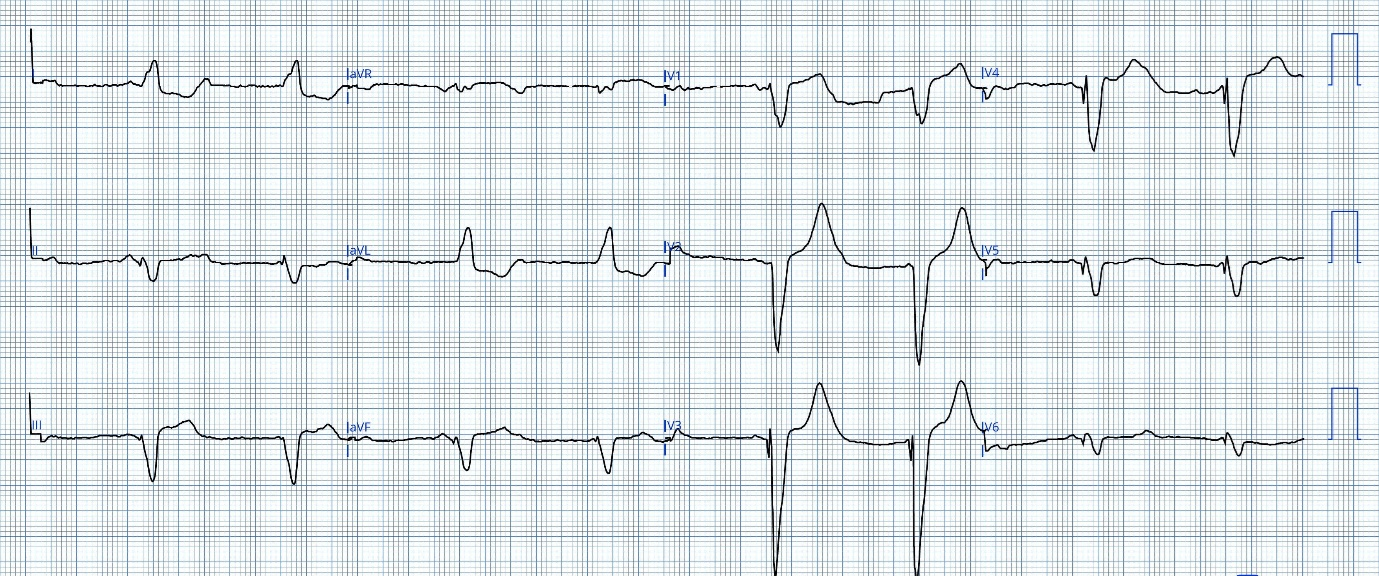
Following a multidisciplinary discussion, it was decided to proceed with multivessel percutaneous coronary intervention. The patient underwent successful intervention of the LAD following calcium modification with rotablation involving the placement of 3 second-generation drug-eluting stents. Routine postprocedural electrocardiography showed a sinus rhythm with evidence of new onset bifascicular block (Figure 2A and B). On postoperative day 2, the patient developed recurrent episodes of syncope at rest; telemetry during these episodes showed complete heart block. Repeat coronary angiography showed patent stents with occlusion of the first and second septal perforators (Figure 3) manifesting as complete heart block by infra-Hisian ischemia. In cases of infra-Hisian ischemia, the major septal perforator courses along the interventricular septum towards its right side and arborizes prior to the moderator band supplying the infra nodal conduction system.1 Occlusion of these septal perforators due to atherosclerosis,2 thrombosis following alcohol septal ablation,3 and injury during aortic valve surgery is associated with development of infra-Hisian conduction blocks.

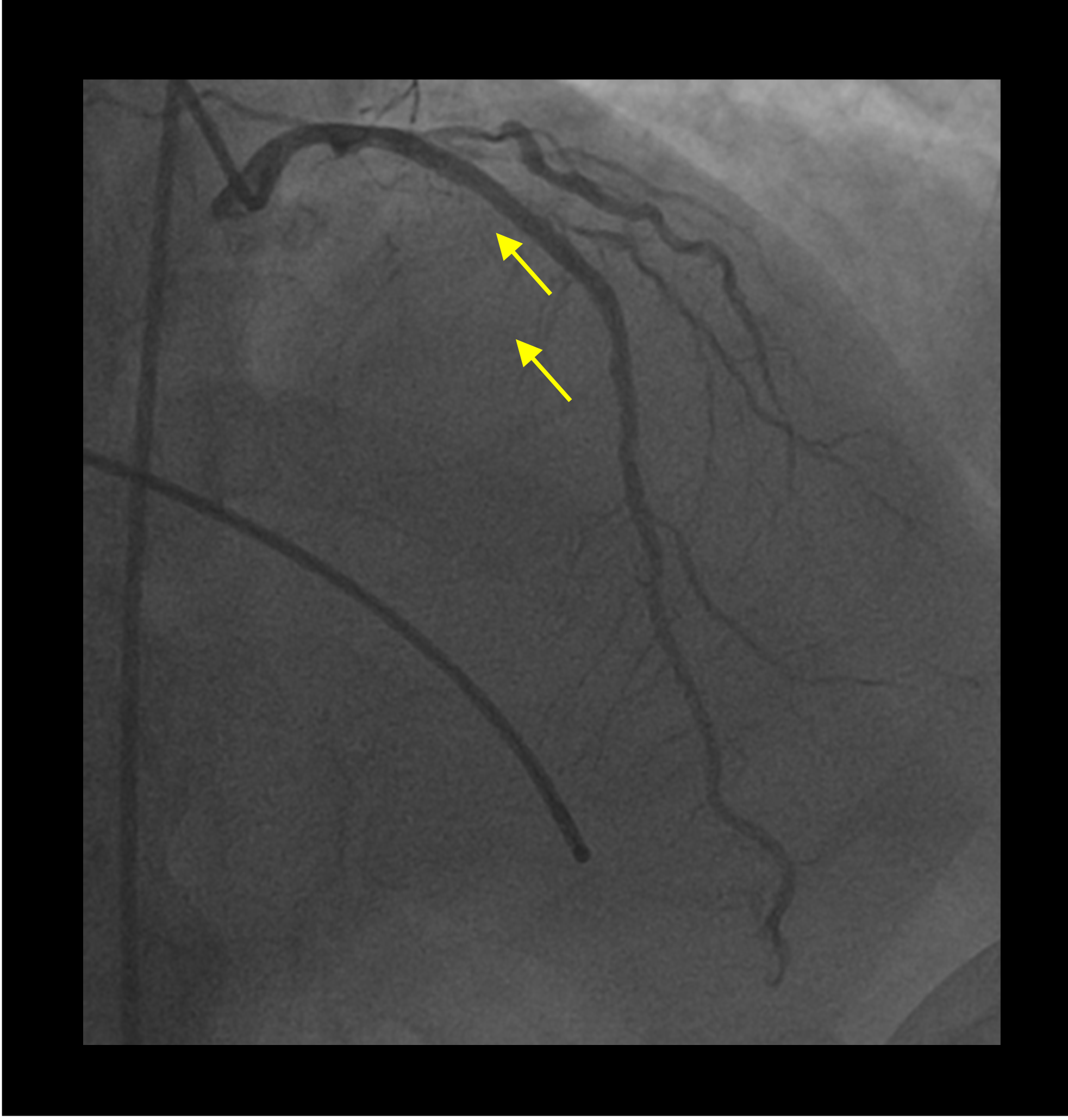
Ischemic injury of the infra-Hisian conduction system following coronary intervention is infrequently reported,4 as extensive anastomosis between the anterior and inferior septal perforators usually precludes extensive septal ischemia. Our patient developed alternating bundle branch block followed by complete heart block secondary to microvascular and macrovascular occlusion during calcium modification and stent deployment. In this case, the significant RCA and LAD obstruction lead to a tenuous balance that was disrupted following intervention.
The patient was monitored for spontaneous resolution with backup temporary transvenous pacing (Figure 2C). Coronary intervention to the occluded septal would have been technically challenging and carried the risk of main vessel stent distortion. We thus proceeded with a dual-chamber permanent pacemaker implantation for persisting complete heart block.
Affiliations and Disclosures
Shivam Goel, MBBS, MD; Nayani Makkar, MBBS, MD, DM; Satyavir Yadav, MBBS, MD, DM
From the Department of Cardiology, All India Institute of Medical Sciences, New Delhi, India.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient(s) for the study and/or intervention(s) described in the manuscript and for the publication of their data/thereof, including any and all images.
Address for correspondence: Satyavir Yadav, MBBS, MD, DM, Department of Cardiology, All India Institute of Medical Sciences, Ansari Nagar (East), New Delhi 110029, India. Email: drsatyaviryadav87@gmail.com
References
- Kim SD. Anatomy of the septal perforating arteries of the heart. Anat Cell Biol. 2019;52(3):236-241. doi:10.5115/acb.18.175
- Chahine J, Thapa B, Gajulapalli RD, Kadri AN, Maroo A. An interesting case of atherosclerotic occlusion of the first septal perforator in a physically young and fit individual causing complete heart block. Cureus. 2019;11(1):e3983. doi:10.7759/cureus.3983
- Lawrenz T, Lieder F, Bartelsmeier M, et al. Predictors of complete heart block after transcoronary ablation of septal hypertrophy: results of a prospective electrophysiological investigation in 172 patients with hypertrophic obstructive cardiomyopathy. J Am Coll Cardiol. 2007;49(24):2356-2363. doi:10.1016/j.jacc.2007.02.056
- Sadiq MA, Azman W, Abidin IZ. Irreversible delayed complete heart block secondary to jailed first septal perforator following PCI of the left anterior descending coronary artery. J Invasive Cardiol. 2012;24(1):E13-E1 5.




















