Aortic Stent Migration and Aneurysmal Rupture After Thoracic Endovascular Aortic Repair
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
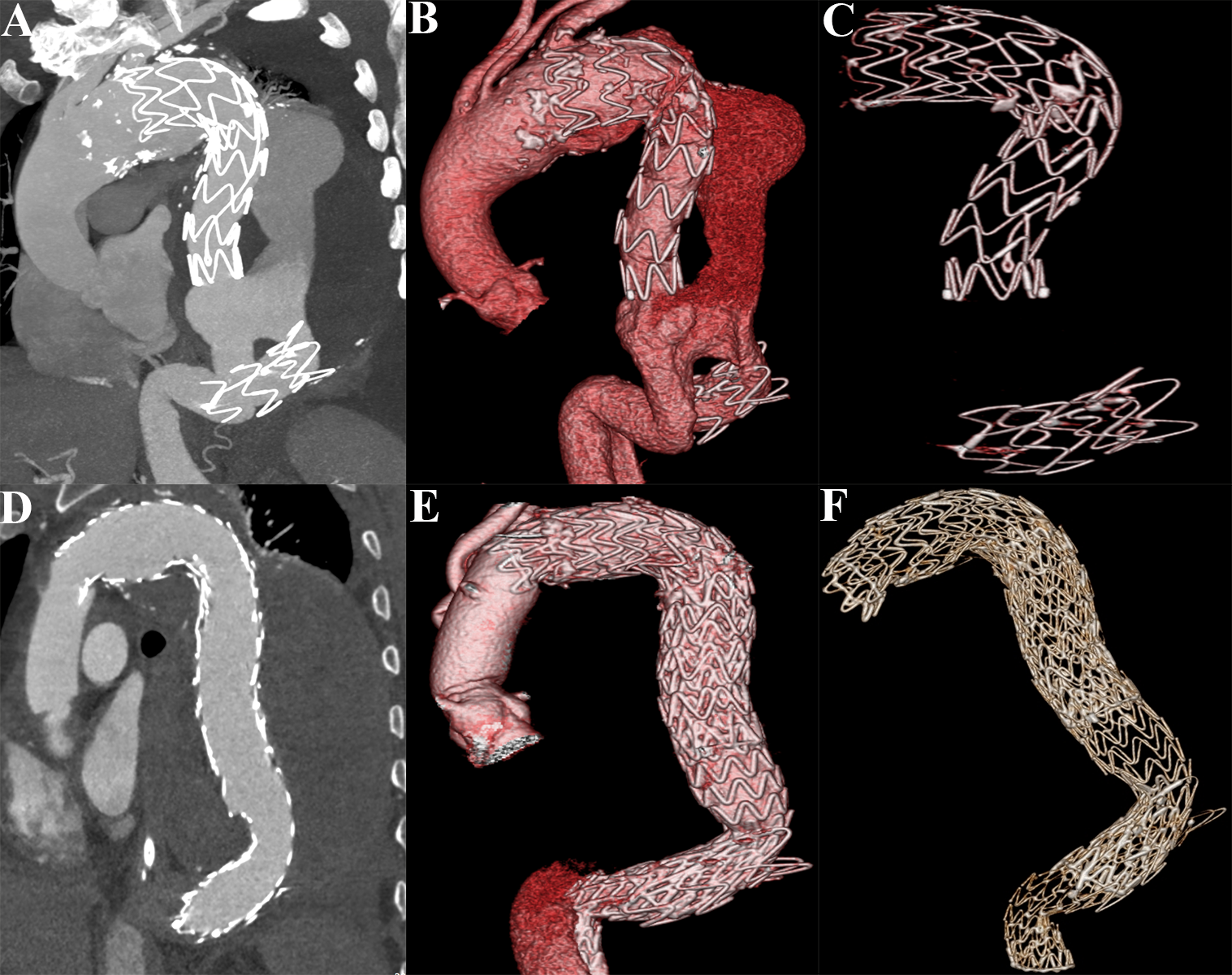
A 62-year-old man presented with chest tightness for half a month. He had a medical history of thoracic endovascular aortic repair (TEVAR) for aortic aneurysm 3 years prior. Computed tomography angiography (CTA) suggested distal aortic stent graft displacement with a massive endoleak and aneurysmal rupture (Figure A-C).
The patient initially underwent surgical debranching and subsequently underwent TEVAR using one 26 x 26 x 10-mm endograft and two 34 x 34 x 20-mm endografts (W.L. Gore & Associates) (Video). The postoperative CTA suggested that the aneurysmal rupture was thromboembolized entirely, with a small amount of type Ib endoleak (Figure D-F). The patient had an uneventful recovery and was discharged 5 days after the postoperative endovascular therapy. The patient's endoleak was stable during the postoperative follow-up at 6 months, and the aneurysmal sac did not grow significantly.
Potential complications of endovascular stent placement include endoleaks, stent migration, pseudoaneurysms, dissection, aortic perforation, kinking, thrombosis, and coverage of vital branch vessels.1 Stent graft migration is relatively uncommon, but is the most severe complication after TEVAR. It is related to type I or III leakage, which may result in aneurysmal growth, rupture, and re-intervention.2 The risk factors or indications of stent graft displacement during TEVAR include aortic elongation, proximal fixed length, and thoracic aortic aneurysm.3 The radiologist must not only detect pathologic abnormalities in the thoracic aorta, but also provide the referring clinician with the essential pre- and post-procedure information to identify appropriate clinical treatment.1
Affiliations and Disclosures
Leizhi Ku, MD1; Shengpeng Guo, MD1; Ming Qi, MD2
From the Departments of 1Radiology and 2Cardiac Surgery, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology, Hankou District, Wuhan, P.R. China.
Dr Ku and Dr Guo contributed equally to the article.
Disclosures: The authors have no conflicts of interest to declare
Funding: This work was funded by the Wuhan Clinical Medical Research Center for Cardiovascular Imaging (CMRC202307).
Consent statement: The authors confirm that informed consent was obtained from the patient for the procedures described in this manuscript.
Address for correspondence: Ming Qi, MD, Department of Cardiac Surgery, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology, No.753 Jinghan Road, Hankou District, Wuhan, P.R. China, 430022. Email: klz13657254286@126.com
References
1. Bean MJ, Johnson PT, Roseborough GS, Black JH, Fishman EK. Thoracic aortic stent-grafts: utility of multidetector CT for pre- and postprocedure evaluation. Radiographics. 2008;28(7):1835-1851. doi:10.1148/rg.287085055
2. Kamada K, Shingaki M, Nakanishi K, Ishikawa K, Koya A, Morishita K. Stent graft migration due to structural failure nine months after thoracic endovascular aortic repair using Valiant Navion. EJVES Vasc Forum. 2023;60:77-80. doi:10.1016/j.ejvsvf.2023.10.002
3. Greenberg RK, Turc A, Haulon S, et al. Stent-graft migration: a reappraisal of analysis methods and proposed revised definition. J Endovasc Ther. 2004;11(4):353-363. doi:10.1583/03-1142R.1




















