One- Versus Two-Stent Stenting Strategies in Coronary Bifurcation Lesions
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
Abstract
Objectives. Additional studies are needed on the follow-up outcomes of 1- vs 2-stent techniques in bifurcation percutaneous coronary interventions (PCI).
Methods. The authors examined the angiographic and procedural characteristics, and outcomes of 1306 bifurcation PCIs (1139 patients) performed at 6 centers between 2014 and 2024 from the PROGRESS-BIFURCATION registry.
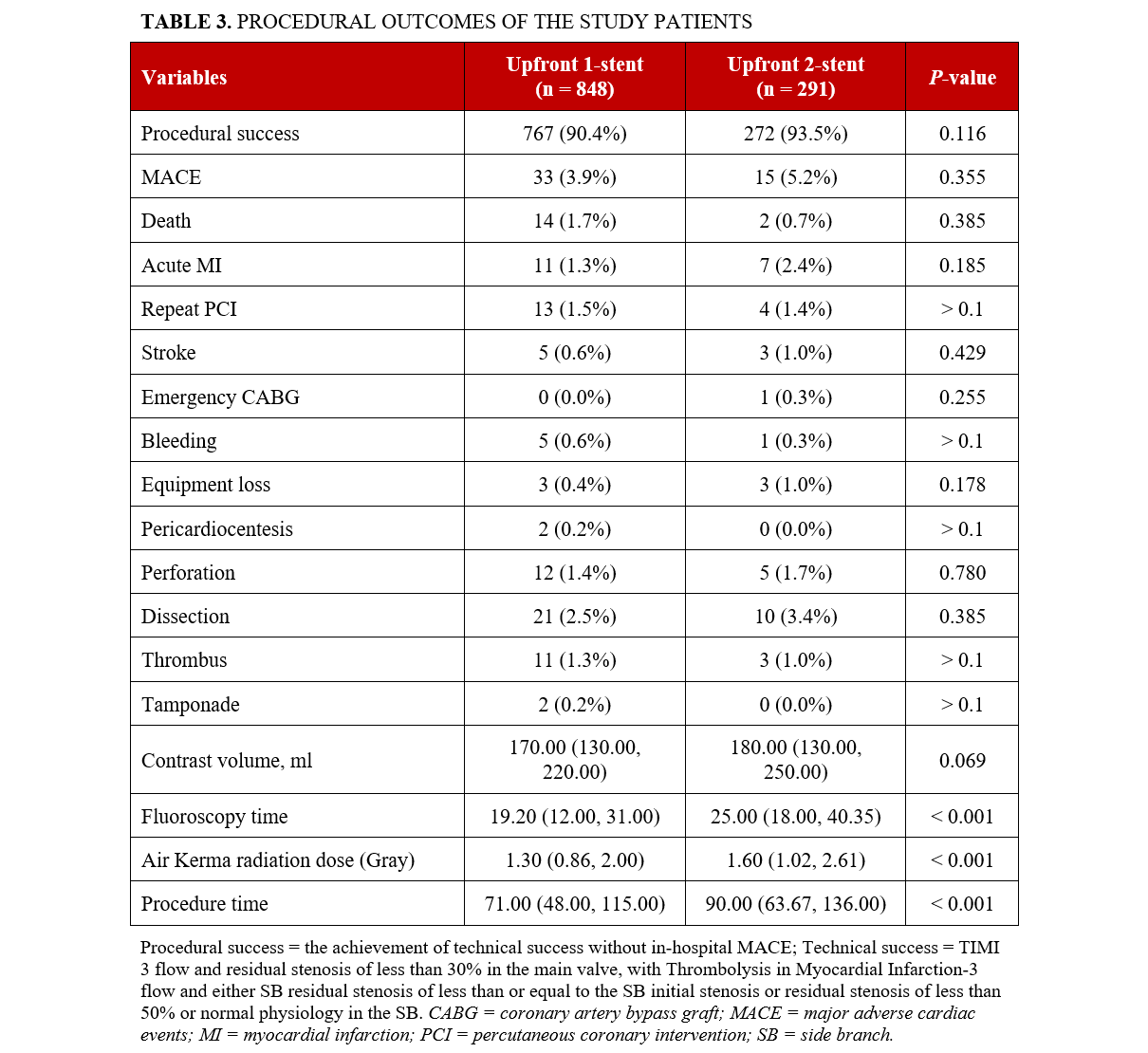
Results. Upfront 1-stent PCI (96.2% provisional stenting, 2% mini crush with 1 stent, 1.7% side branch [SB] stent only) was used in 75.5% of lesions; upfront 2-stent PCI was used in 24.5% (48.1% double kissing crush, 16.9% culotte, 35% other). Patients treated with an upfront 2-stent strategy were older (68 ± 12 vs 66 ± 12 years; P = .011) and more likely to have dyslipidemia (82.7% vs 76.0%; P = .019) and a history of heart failure (27.6% vs 20.3%; P = .011). An upfront 2-stent strategy was more common in left main bifurcations and lesions with moderate/severe calcification or larger SB diameter. Upfront 2-stent strategies required longer procedure and fluoroscopy times and higher patient radiation dose but similar contrast volume. Two-stent strategies were associated with higher technical success (98.4% vs 94.4%; P = .003), but similar procedural success (93.5% vs 90.4%; P = .116) and in-hospital major adverse cardiac events (MACE) (5.2% vs 3.9%; P = .355) compared with 1-stent strategies. Follow-up data was available for 783 patients. During a median follow-up of 1095 days, patients treated with an upfront 2-stent strategy had similar incidence of MACE, target vessel revascularization, myocardial infarction, and all-cause mortality (adjusted hazard ratio for mortality, 0.99; 95% CI, 0.61-1.62; P = .98).
Conclusions. Upfront 1- vs 2-stent bifurcation PCI was associated with similar procedural success and follow-up outcomes during a median follow-up of 3 years.
Introduction
Approximately 20% of percutaneous coronary interventions (PCI) involve a bifurcation.1-3 Bifurcation PCI can be complex and has been associated with worse clinical outcomes compared with PCI of non-bifurcated lesions.1-3 Whereas provisional stenting is accepted as the preferred PCI strategy for most bifurcations, 2-stent strategies are performed in a significant subset.4,5 We compared upfront single vs 2-stent strategies in a large, multicenter bifurcation PCI registry.
Methods
We examined the angiographic characteristics, procedural characteristics, and outcomes of 1306 bifurcation PCIs (1139 patients) performed at 6 centers between 2014 and 2024 that were included in the Prospective Global Registry for the Study of Bifurcation Lesion Interventions (PROGRESS-BIFURCATION, ClinicalTrials.gov Identifier: NCT05100992). The Research Electronic Data Capture (REDCap) hosted at the Minneapolis Heart Institute Foundation was used to capture and manage anonymized data. The study was approved by the institutional review board of the participating centers.
The primary endpoint of the study was the incidence of follow-up outcomes: major adverse cardiac events (MACE), target vessel revascularization (TVR), myocardial infarction (MI), and all-cause mortality. Secondary endpoints were technical and procedural success. Follow-ups were conducted through medical record review.
Bifurcation lesions were defined as coronary artery stenoses adjacent to and/or involving the origin of a significant side branch (SB).6 When SB stenting was attempted, technical success was defined as achievement of Thrombolysis in Myocardial Infarction (TIMI)-3 flow and a residual stenosis of less than 30% in both the main vessel (MV) and the SB. If there was no attempt to stent the SB, technical success was defined as achievement of TIMI-3 flow in the MV and either an SB residual stenosis of less than or equal to the initial SB stenosis or a residual SB stenosis of less than 50% or normal SB physiology alongside TIMI-3 flow. Procedural success was defined as the achievement of technical success without in-hospital MACE. In-hospital MACE was defined as the composite of death, MI, stroke, urgent repeat of TVR via either PCI or coronary artery bypass graft (CABG) surgery because of recurring symptoms, and tamponade necessitating either surgical intervention or pericardiocentesis prior to discharge. MI was defined as type 4a MI using the Third Universal Definition of Myocardial Infarction. Acute kidney injury (AKI) was diagnosed as an increase in creatinine of greater than or equal to 0.3 mg/dL or more than 1.5 times the baseline creatinine within 48 hours post-procedure.
The Medina classification was used as described by Medina et al.7 Follow-up MACE was defined as the composite of death, MI, stroke, urgent repeat of TVR via either PCI or CABG because of recurring symptoms, and tamponade necessitating either surgical intervention or pericardiocentesis after discharge from the hospital. Follow-up TVR was defined as any repeat PCI or surgical bypass of the target vessel, and non-target vessel revascularization (NTVR) was defined as any repeat PCI or surgical bypass of a non-target vessel. Repeat PCI or surgical bypass of the target lesion for restenosis or other complications were defined as follow-up target lesion revascularization (TLR). Heart failure was defined as physician documentation or report of any of the following clinical symptoms of heart failure described as: unusual dyspnea on light exertion, recurrent dyspnea occurring in the supine position, fluid retention; or the description of rales, jugular venous distention, pulmonary edema on physical exam, or pulmonary edema on chest x-ray. A low ejection fraction alone, without clinical evidence of heart failure did not qualify as heart failure.8 A bifurcation lesion was considered complex using the DEFINITION criteria.9
Statistical methods
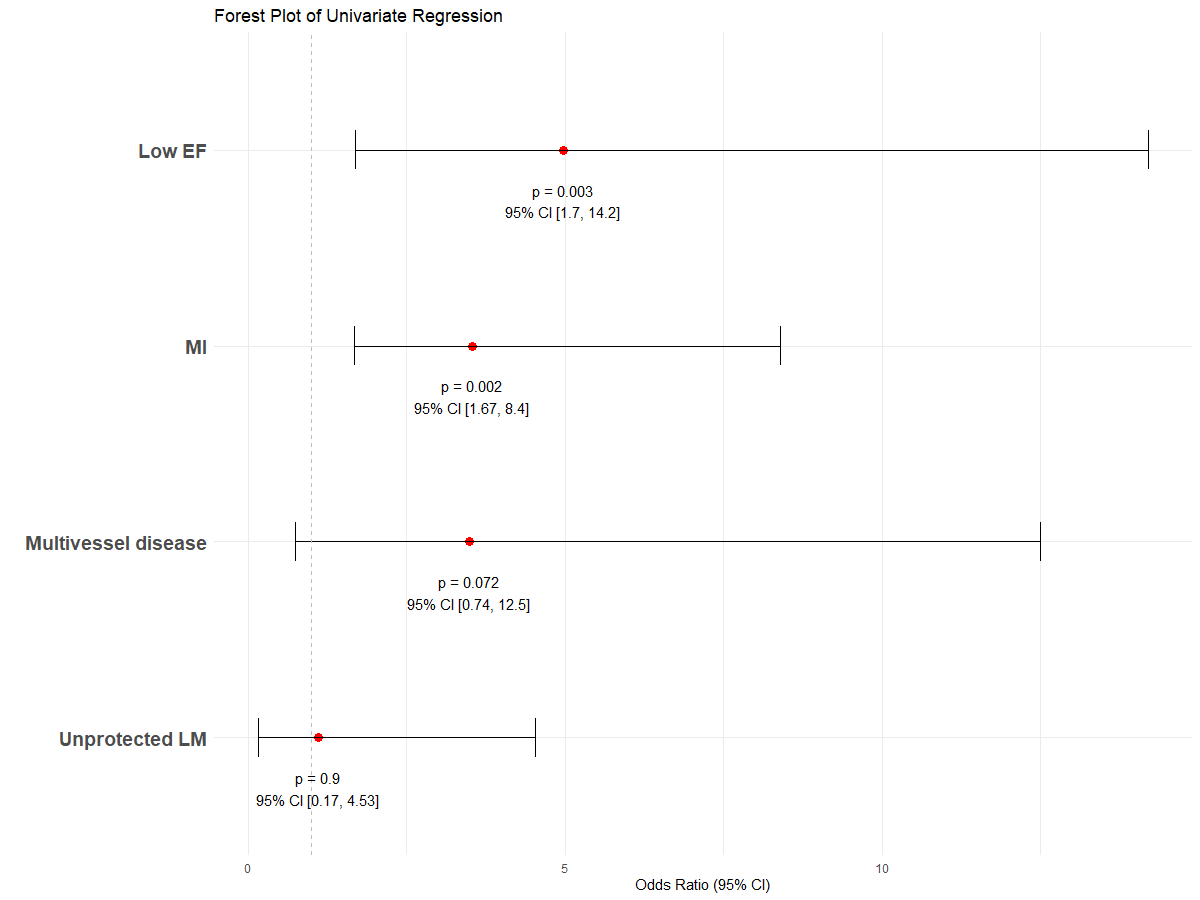
Categorical variables were presented as percentages and compared using Pearson’s chi-square test. Continuous variables were described as mean ± SD for normally distributed data or median with IQR for non-normally distributed data. Normally distributed data were analyzed using the independent-sample t-test; non-parametric data were analyzed using the Mann-Whitney U-test. Univariable logistic regression analysis was initially used to evaluate the effect of different stenting strategies on bifurcation PCI for technical success and periprocedural or in-hospital MACE. Variables found to be associated with outcomes at a significance level of P less than 0.10 were included in the multivariable models. Kaplan-Meier survival analysis was used to calculate the incidence of follow-up events, which were compared using the log-rank test and mixed effects Cox proportional hazard ratios (HR). All statistical analyses were performed using R Statistical Software, version 4.4.0 (R Foundation for Statistical Computing). A P-value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
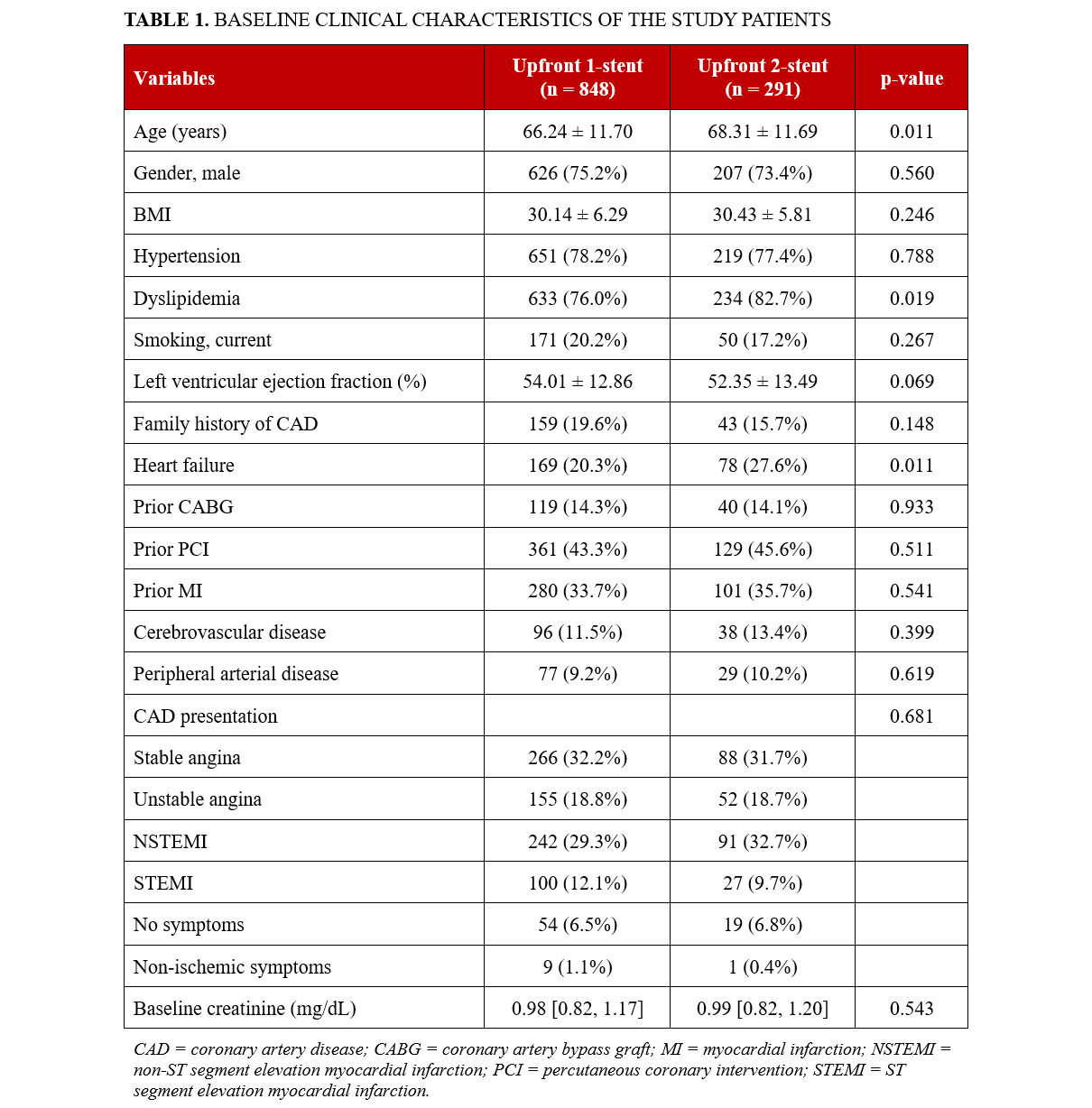
Between 2014 and 2024, upfront 1-stent strategies were used in 986 out of 1306 bifurcations (75.5%), and upfront 2-stent strategies were used in the remaining 24.5% (320). Provisional stenting was used in 96.2% (949) of upfront 1-stent strategies and SB-only stenting in the remaining 3.8% (37): 1.7% (17) SB stenting without crushing and 2% (20) SB stenting followed by MV balloon inflation crushing the protruding segment of the SB stent (mini crush). Double kissing (DK) crush was used in 48.1% (154) of upfront 2-stent strategies, culotte in 16.9% (54), and other techniques in 35% (112). Patients who underwent upfront 3-stent strategies were older, more likely to have dyslipidemia, and more likely to have heart failure (Table 1).
Angiographic characteristics
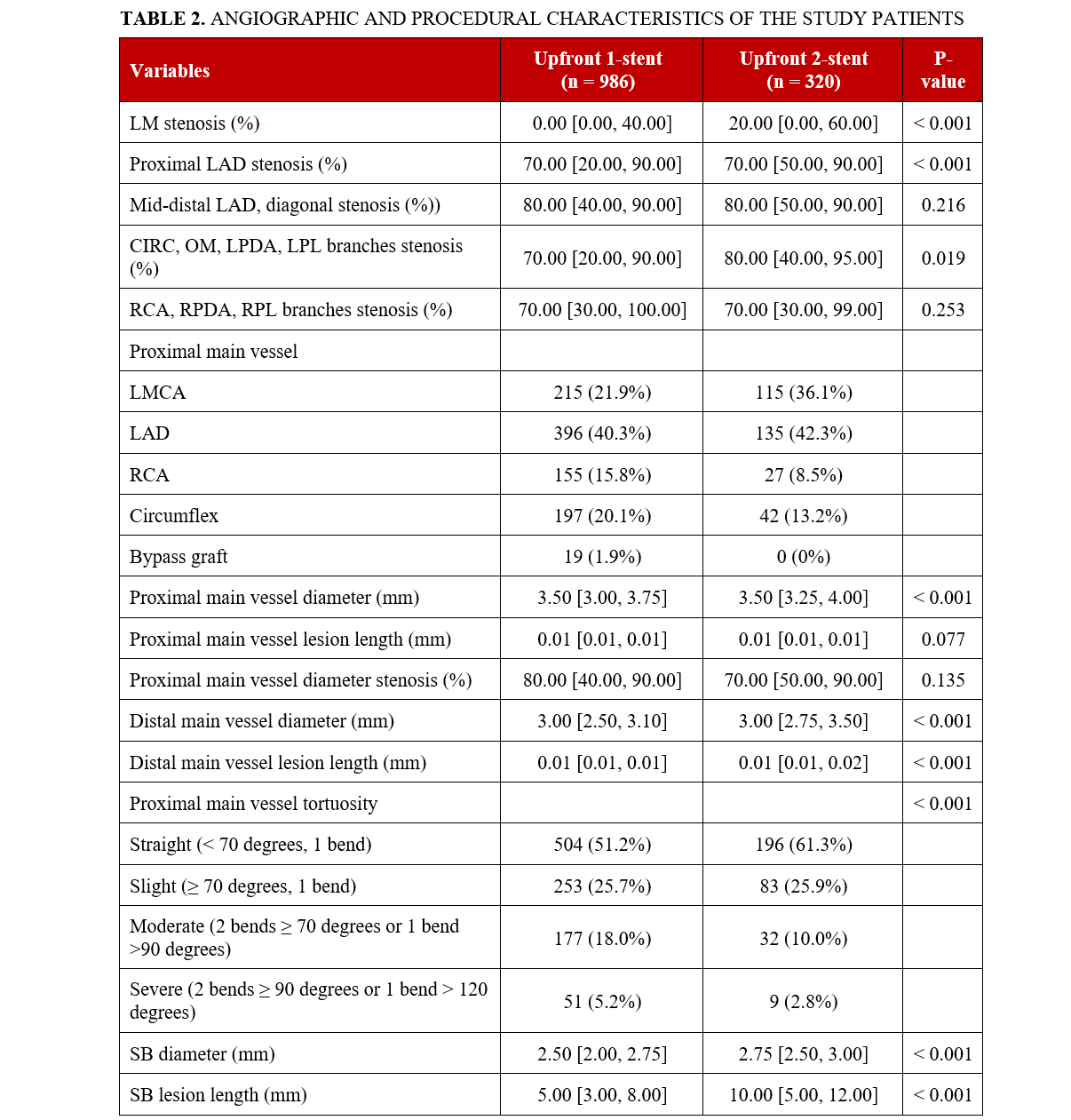
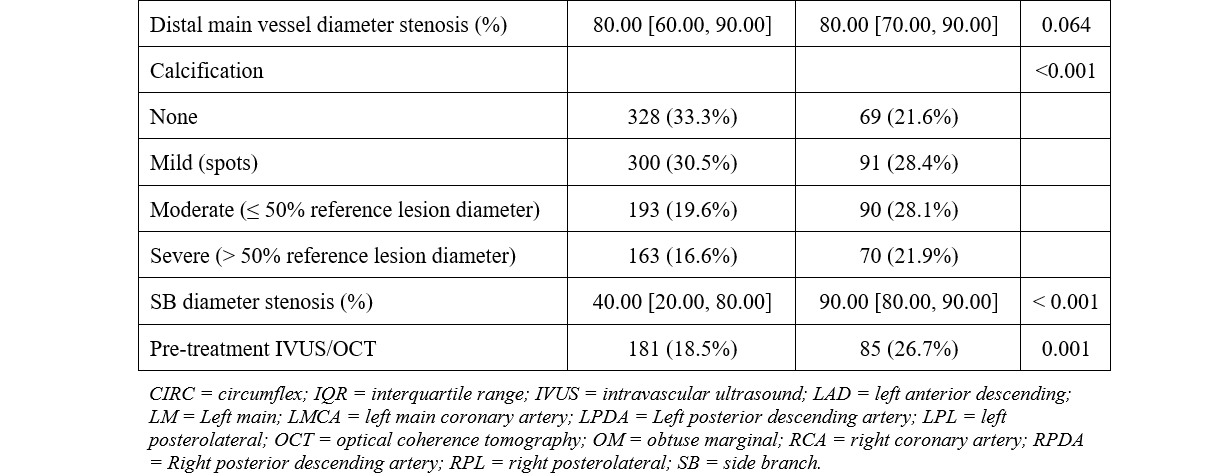
Table 2 displays the angiographic characteristics of the study lesions. Two-stent strategies were more often used in the left main coronary artery (LMCA) and the left anterior descending artery (LAD) as its proximal MV and less often in the right coronary artery (RCA) and circumflex artery. Patients treated with upfront 2-stent strategies had larger proximal and distal MV diameters along with longer MV lesion length. The same trend was observed for SB diameter and lesion length. Two-stent strategies were more common in cases with moderate to severe calcification and less common in cases with moderate to severe tortuosity.
In-hospital outcomes
Upfront 2-stent strategies had higher technical success (98.4% vs 94.4%; P = .003) without significant difference in procedural success (Table 3), longer procedure and fluoroscopy times, and higher air kerma radiation dose, but similar contrast volume.
Follow-up outcomes
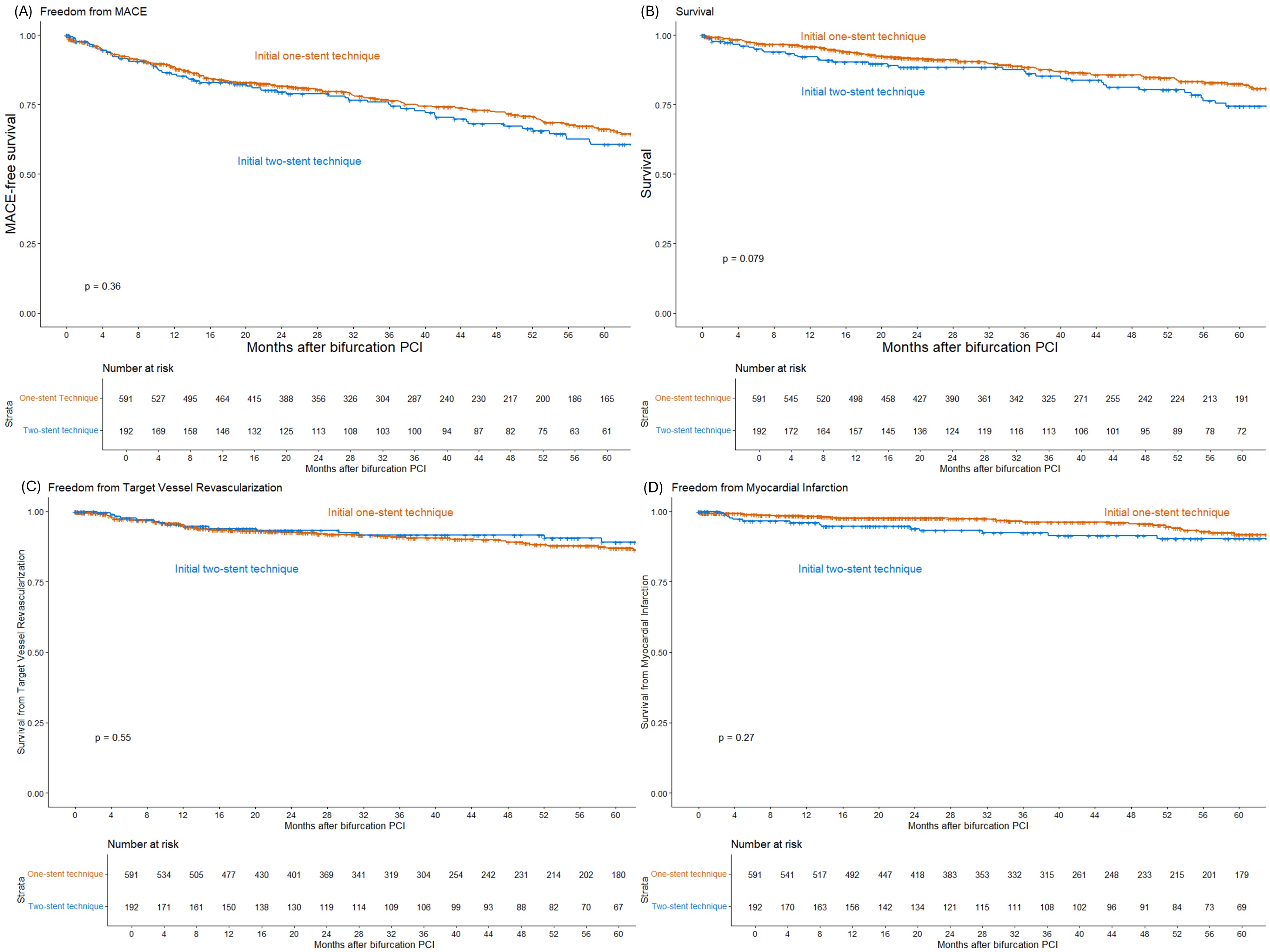
Follow-up data was available for 783 (68.7%) of the 1139 patients for a median follow-up duration of 1095 days. Compared with an upfront single stent strategy, upfront 2-stent techniques had similar incidence of follow-up MACE (HR, 1.18; 95% CI, 0.89-1.57; P = .36), TVR (HR, 0.85; 95% CI, 0.49-1.48; P = .55), and MI (HR, 1.48; 95% CI, 0.80-2.74; P = .27), and a trend for higher all-cause mortality (HR, 1.39; 95% CI, 0.96-2.02; P = .079). After adjusting for confounders, all-cause mortality was similar for 1- and 2-stent strategies (HR, 0.99; 95% CI, 0.61-1.62; P = .98) (Figure).
Subgroup outcomes
There was higher follow-up MACE in acute MI patients and low left ventricular ejection fraction (LVEF) patients who underwent an upfront 2-stent strategy than those who underwent a 1-stent strategy. There was no significant difference in patients with multivessel disease (MVD) or unprotected left main (LM) disease (Supplemental Figure). Using the DEFINITION criteria,9 298 patients had simple bifurcation lesions, of which provisional stenting was used in 215 (72.1%) patients and 2-stent techniques in 99 (33.2%) patients; 815 patients had complex bifurcation lesions, of which provisional stenting was used in 578 (70.9%) patients and 2-stent techniques in 259 (31.8%) patients.
Discussion
The major findings of our study are that, in bifurcation PCI, (a) upfront 1-stent strategies were utilized more often than upfront 2-stent strategies; (b) patients treated with upfront 2-stent strategies were older with more comorbidities and had higher prevalence of LM bifurcations, less lesion tortuosity, more calcification, and a larger SB diameter; (c) upfront 2-stent strategies had higher technical but similar procedural success and in-hospital MACE; and (d) upfront 2-stent strategies had similar incidence of follow-up MACE, TVR, MI, and all-cause mortality.
As expected, most (75.5%) bifurcations in our study were treated using an upfront single-stent strategy.4,5 According to the European Bifurcation Club, provisional stenting is preferred for most bifurcation lesions.10 The most frequently used upfront 2-stent strategy was DK crush (used in 48.1%).11 Patients treated with an upfront 2-stent technique were older and more likely to have dyslipidemia and heart failure.12-14 They also had larger main and SB diameters, longer lesion length, and required longer fluoroscopy times and higher air kerma radiation dose.
Despite more comorbidities and higher lesion complexity, patients treated with an upfront 2-stent strategy had similar long-term outcomes to patients treated with the provisional approach. Previous studies and meta-analyses have produced mixed results on this issue. The 5-year follow-up of the European Bifurcation Club (EBC) TWO Trial15 showed no difference between upfront 1- vs 2-stent strategies, similar to other studies.12-14 In contrast, the Double Kissing Crush versus Provisional Stenting for Left Main Distal Bifurcation Lesions (DK-CRUSH) II16 and DK-CRUSH V17 trials showed lower TLR and TVR with upfront 2-stent compared with provisional stenting. All-cause 5-year mortality was lower with provisional stenting in the Nordic and British Bifurcation studies,18 alongside other studies.4,19-23 Judicious use of upfront 2-stent strategies is important for optimizing both the acute and long-term outcomes of bifurcation PCI.
Limitations
The PROGRESS‐BIFURCATION registry is an observational registry subject to all inherent limitations. All PCIs were performed at specialized centers, which can limit the generalizability of the results. The study included procedures from 2014 to 2024, and the indications for intravascular imaging significantly changed during that period. Clinical events were not independently adjudicated, and there was no core laboratory analysis of the angiographic images. The choice of stenting technique was at the discretion of the operator.
Conclusions
Upfront 1-stent bifurcation PCIs had lower technical success but were associated with similar procedural success and follow-up outcomes compared with upfront 2-stent strategies during a median period of 3 years.
Affiliations and Disclosures
Zachary Chan, BS1,2; Michaella Alexandrou, MD2; Dimitrios Strepkos, MD2; Deniz Mutlu, MD2; Pedro E. P. Carvalho, MD2; Oleg Krestyaninov, MD3; Dmitrii Khelimskii, MD3; Barkin Kultursay, MD4; Ali Karagoz, MD4; Ufuk Yildirim, MD5; Korhan Soylu, MD5; Mahmut Uluganyan, MD6; Ozgur Selim Ser, MD2; Olga Mastrodemos, BA2; Bavana V. Rangan, BDS, MPH2; Sandeep Jalli, DO2; Konstantinos Voudris, MD, PhD2; Yader Sandoval, MD2; M. Nicholas Burke, MD2, Emmanouil S. Brilakis, MD, PhD2
From 1Cornell University, Ithaca, New York; 2Minneapolis Heart Institute and Minneapolis Heart Institute Foundation, Abbott Northwestern Hospital, Minneapolis, Minnesota; 3Meshalkin Novosibirsk Research Institute, Novosibirsk, Russia; 4Kartal Kosuyolu Postgraduate Training and Research Hospital, Istanbul, Turkey; 5Ondokuz Mayis University, Samsun, Turkey, 6Bezmialem Vakif University, Istanbul, Turkey.
The abstract has been previously published: Chan Z, Alexandrou M, Stepkos D, et al. One- vs two-stent stenting strategies in coronary bifurcation lesions. JACC. 85(12_Supplement):857. doi:10.1016/S0735-1097(25)01341-5
Acknowledgments: The authors are grateful for the philanthropic support of our generous anonymous donors (2), and the philanthropic support of Drs Mary Ann and Donald A. Sens; Mrs Diane and Dr Cline Hickok; Mrs Wilma and Mr Dale Johnson; the Mrs Charlotte and Mr Jerry Golinvaux Family Fund; the Roehl Family Foundation; the Joseph Durda Foundation; Ms Marilyn and Mr William Ryerse; and Mr Greg and Mrs Rhoda Olsen. The generous gifts of these donors to the Minneapolis Heart Institute Foundation’s Science Center for Coronary Artery Disease (CCAD) helped support this research project.
Disclosures: Dr Sandoval is a consultant for, and serves on the advisory board of Abbott and gE Healthcare; is a consultant for, serves on the advisory board of, and is a speaker for Roche Diagnostics and Philips; serves on the advisory board of Zoll; is a consultant for CathWorks; is a speaker for HeartFlow; is a speaker for, and receives research grants from Cleerly; is an associate editor for JACC Advances; and he and others hold patent 20210401347. Dr Brilakis receives consulting/speaker honoraria from Abbott Vascular, the American Heart Association (Associate Editor, Circulation), Biotronik, Boston Scientific, Cardiovascular Innovations Foundation (Board of Directors), Cordis, CSI, Elsevier, GE Healthcare, Haemonetics, IMDS, Medtronic, SIS Medical, Teleflex, and Orbus Neich; receives research support from Boston Scientific and GE Healthcare; is the owner of Hippocrates, LLC; and is a shareholder in LifeLens Technologies, Inc, MHI Ventures, Cleerly Health, Stallion Medical, and TrueVue, Inc. The remaining authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Emmanouil S. Brilakis, MD, PhD, Minneapolis Heart Institute, 920 E 28th Street #300, Minneapolis, MN 55407, USA. Email: esbrilakis@gmail.com; X: @esbrilakis
References
1. Park DY, An S, Jolly N, et al. Systematic review and network meta‐analysis comparing bifurcation techniques for percutaneous coronary intervention. J Am Heart Assoc. 2022;11(12):e025394. doi:10.1161/JAHA.122.025394
2. Garot P, Lefèvre T, Savage M, et al. Nine-month outcome of patients treated by percutaneous coronary interventions for bifurcation lesions in the recent era: a report from the Prevention of Restenosis With Tranilast and its Outcomes (PRESTO) Trial. J Am Coll Cardiol. 2005;46(4):606-612. doi:10.1016/j.jacc.2005.01.065
3. Kırat T. Fundamentals of percutaneous coronary bifurcation interventions. World J Cardiol. 2022;14(3):108-138. doi:10.4330/wjc.v14.i3.108
4. Ford TJ, McCartney P, Corcoran D, et al. Single‐ versus 2‐stent strategies for coronary bifurcation lesions: a systematic review and meta‐analysis of randomized trials with long‐term follow‐up. J Am Heart Assoc. 2018;7(11):e008730. doi:10.1161/JAHA.118.008730
5. Kan J, Zhang JJ, Sheiban I, et al. 3-year outcomes after 2-stent with provisional stenting for complex bifurcation lesions defined by DEFINITION criteria. JACC Cardiovasc Interv. 2022;15(13):1310-1320. doi:10.1016/j.jcin.2022.05.026
6. Louvard Y, Thomas M, Dzavik V, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2008;71(2):175-183. doi:10.1002/ccd.21314
7. Medina A, Suárez de Lezo J, Pan M. [A new classification of coronary bifurcation lesions]. Rev Esp Cardiol. 2006;59(2):183.
8. Cannon CP, Brindis RG, Chaitman BR, et al. 2013 ACCF/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease. Circulation. 2013;127(9):1052-1089. doi:10.1161/CIR.0b013e3182831a11
9. Chen SL. DEFINITION criteria for left main bifurcation stenting - from clinical need to a formula. AsiaIntervention. 2023;9(1):20-24. Published 2023 Mar 15. doi:10.4244/AIJ-D-22-00074
10. Pan M, Lassen JF, Burzotta F, et al. The 17th expert consensus document of the European Bifurcation Club - techniques to preserve access to the side branch during stepwise provisional stenting. EuroIntervention. 2023;19(1):26-36. doi:10.4244/EIJ-D-23-00124
11. Nikolakopoulos I, Vemmou E, Karacsonyi J, et al. Practice patterns in the interventional treatment of coronary bifurcation lesions: a global survey. J Invasive Cardiol. 2022;34(1):E43-E48. doi:10.25270/jic/21.00077
12. Zhang J, Liu S, Geng T, Xu Z. One-stent versus two-stent techniques for distal unprotected left main coronary artery bifurcation lesions. Int J Clin Exp Med. 2015;8(8):14363-14370.
13. Lee CH, Ahn JM, Kang DY, et al. Comparison of simple versus complex stenting in patients with true distal left main bifurcation lesions. Catheter Cardiovasc Interv. 2021;97(5):776-785. doi:10.1002/ccd.29219
14. Gao Z, Xu B, Yang Y, et al. Comparison between one-stent versus two-stent technique for treatment of left main bifurcation lesions: a large single-center data. Catheter Cardiovasc Interv. 2015;85(7):1132-1138. doi:10.1002/ccd.25849
15. Arunothayaraj S, Behan MW, Lefèvre T, et al. Stepwise provisional versus systematic culotte for stenting of true coronary bifurcation lesions: five-year follow-up of the multicentre randomised EBC TWO Trial. EuroIntervention. Published online May 16, 2023. doi:10.4244/EIJ-D-23-00211
16. Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions. JACC. 2011;57(8):914-920. doi:10.1016/j.jacc.2010.10.023
17. Chen X, Li X, Zhang JJ, et al. 3-year outcomes of the DKCRUSH-V Trial comparing DK crush with provisional stenting for left main bifurcation lesions. JACC Cardiovasc Interv. 2019;12(19):1927-1937. doi:10.1016/j.jcin.2019.04.056
18. Behan MW, Holm NR, de Belder AJ, et al. Coronary bifurcation lesions treated with simple or complex stenting: 5-year survival from patient-level pooled analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Eur Heart J. 2016;37(24):1923-1928. doi:10.1093/eurheartj/ehw170
19. Katritsis DG, Siontis GCM, Ioannidis JPA. Double versus single stenting for coronary bifurcation lesions. Circ Cardiovasc Interv. 2009;2(5):409-415. doi:10.1161/CIRCINTERVENTIONS.109.868091
20. Cho S, Kang TS, Kim JS, et al. Long-term clinical outcomes and optimal stent strategy in left main coronary bifurcation stenting. JACC Cardiovasc Interv. 2018;11(13):1247-1258. doi:10.1016/j.jcin.2018.03.009
21. Kandzari DE, Gershlick AH, Serruys PW, et al. Outcomes among patients undergoing distal left main percutaneous coronary intervention. Circ Cardiovasc Interv. 2018;11(10):e007007. doi:10.1161/CIRCINTERVENTIONS.118.007007
22. Sarma VRSS, Gopalakrishna K, Purnachandra Rao K, et al. A study of unprotected left main intervention in the ACS population 2013–2018. Indian Heart J. 2021;73(4):492-496. doi:10.1016/j.ihj.2021.06.010
23. Ferenc M, Banholzer N, Hochholzer W, et al. Long-term results after PCI of unprotected distal left main coronary artery stenosis: the Bifurcations Bad Krozingen (BBK)-Left Main Registry. Clin Res Cardiol. 2019;108(2):175-184. doi:10.1007/s00392-018-1337-9