A Kissing WATCHMAN Approach to Bilobar Left Atrial Appendage Occlusion
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00286. Epub September 24, 2025.
An 83-year-old man with a history of atrial fibrillation presented with a subdural hematoma. His apixaban was stopped and a pacemaker was implanted. He re-presented twice following discharge with new neurological findings: the first time was due to extension of his subdural haematoma, and the second time was for a transient ischaemic attack. It was decided to proceed with left atrial appendage occlusion (LAAO).
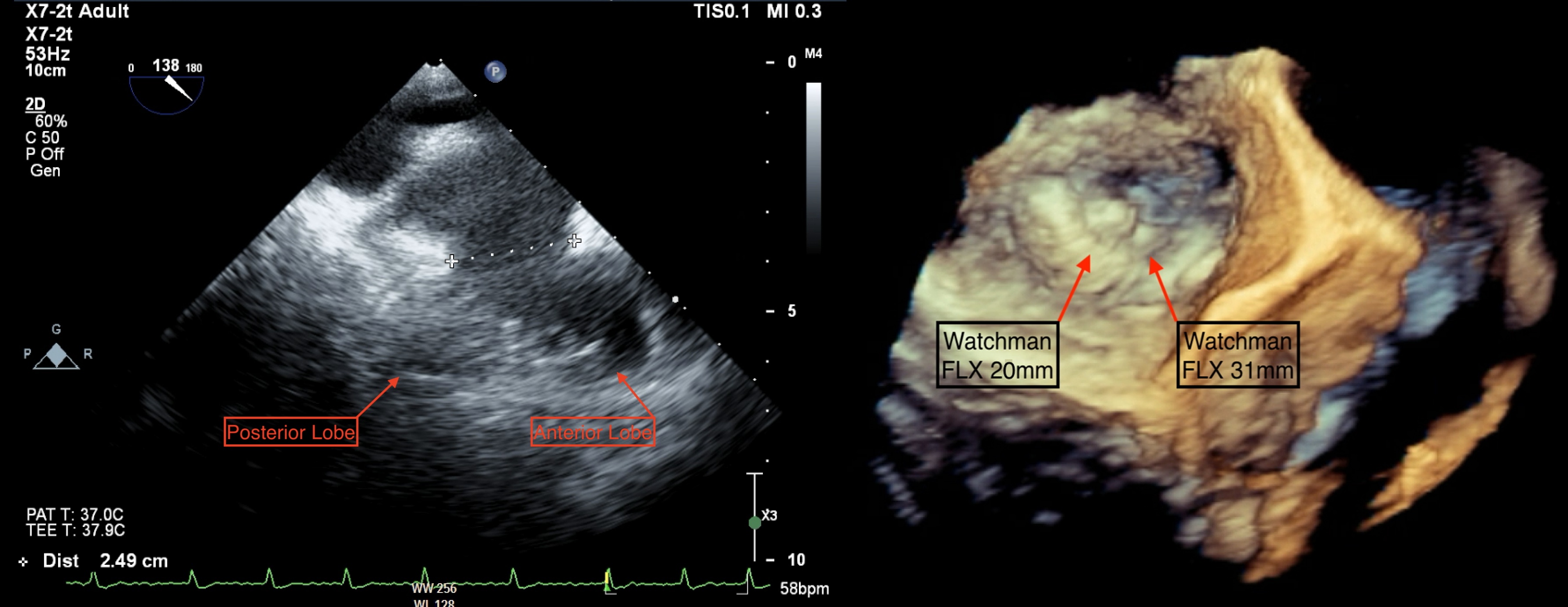
There was no pre-procedure computed tomography as per local protocol. LAA angiography and transoesophageal echocardiography (TOE) revealed a large bilobar LAA (Figure 1A; Video 1) with a maximum ostial diameter of 26 mm. A 31-mm WATCHMAN FLX device (Boston Scientific) was chosen; however, despite multiple device positions, it resulted in complete closure of the anterior lobe and complete patency of the posterior lobe (Video 2).
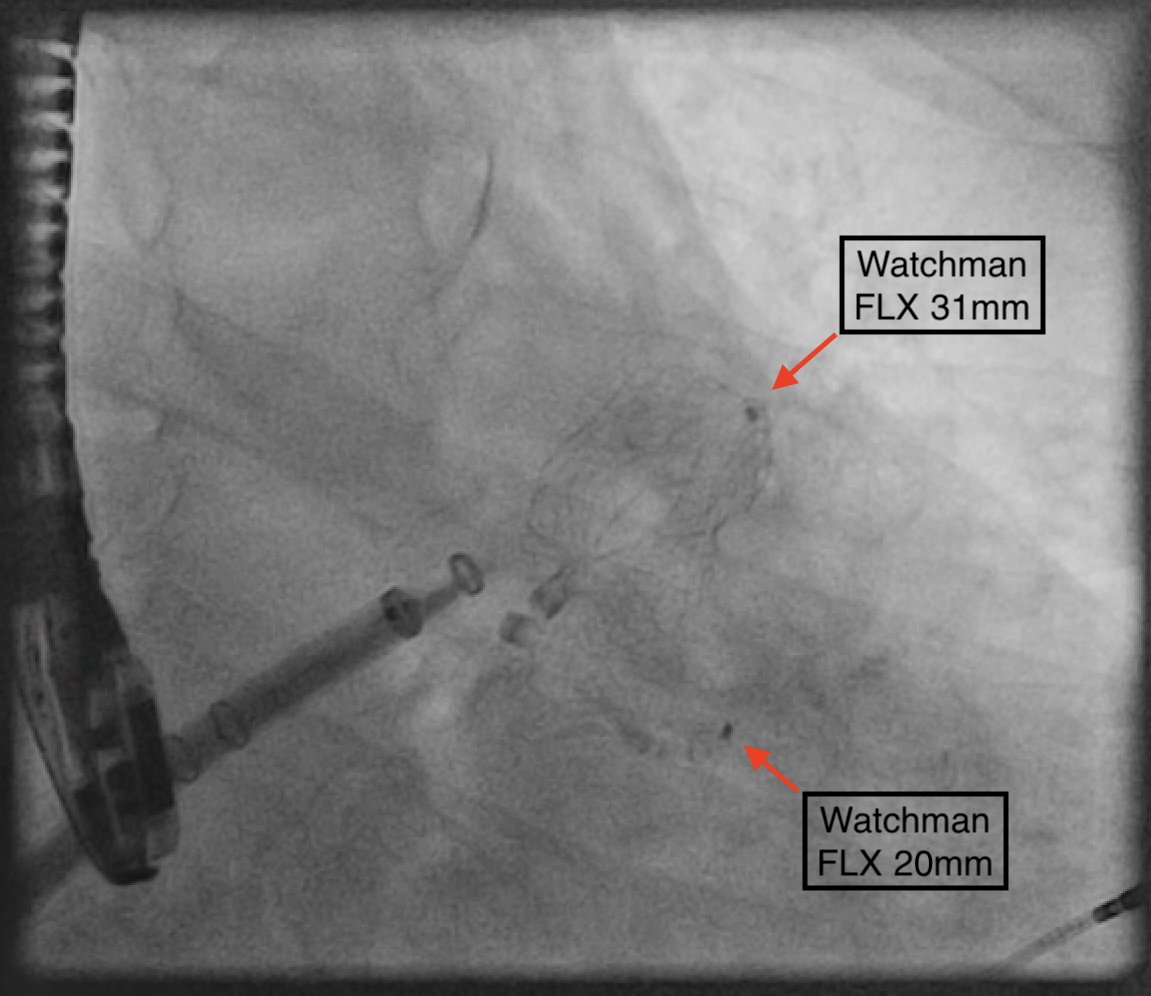
As there were no suitable alternative devices available, it was decided that a dual device closure strategy would be feasible, given the residual ostial diameter of 10 mm in the posterior lobe. Using a sequential single sheath strategy, the 31-mm WATCHMAN FLX was deployed in the larger anterior lobe. Subsequently, a 20-mm WATCHMAN FLX was delivered, positioned, and unsheathed on the first attempt. Both devices were stable in a kissing arrangement in the LAA (Figure 2), with reassuring TOE images (Figure 1B).
The patient was discharged the following day on aspirin monotherapy. His 3-month surveillance TOE showed well-seated devices with no significant leak or no device-related thrombus.
This case highlights the complexity of LAAO in patients with significant variations in anatomy. Dual-device closure was a safe and feasible solution in this case; however, long-term efficacy and thrombotic risk for this strategy remains unknown.
Affiliations and Disclosures
Gregory Offiah, MB, BAO, BCh; Ciara Mahon, MB, MAO, BCh; James Shand, MBBS, MD, FRCP
From the Department of Cardiology, St Vincent’s University Hospital, Dublin, Ireland.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication of their data/thereof, including any and all images
Address for correspondence: Gregory Offiah, MB, BAO, BCh, Department of Cardiology, St Vincent’s University Hospital, Dublin 4, Ireland. Email: goffiah@tcd.ie. X: @gregoffiah




















