Closure Devices Versus Manual Compression to Achieve Hemostasis Post-Patent Foramen Ovale Closure
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
Abstract
Objectives. Venous access plays a crucial role in various interventional cardiology procedures, including percutaneous patent foramen ovale (PFO) closure. Traditionally, manual compression has been the standard method for achieving hemostasis following venous access. However, this approach may be associated with potential complications such as puncture site bleedings. The aim of the study was to compare the safety and efficacy of different venous closure techniques.
Methods. The authors conducted a single-center observational study of 220 patients undergoing PFO closure. The study quasi-randomized participants to 1 of 3 methods: Z-suture closure, Perclose ProGlide suture-mediated closure (Abbott), and manual compression. The primary outcome was the occurrence of bleeding events, classified according to the standardized Bleeding Academic Research Consortium (BARC) classification system.
Results. Bleeding events were not significantly different between the closure groups. Of the patients who received manual compression, 14.2% (n = 17) experienced BARC bleeding events of 2 or higher. In the Z-suture group, 14.5% (n = 7) of patients had BARC bleeding events of 2 or higher. In the ProGlide group, 15% (n = 8) of patients experienced such events (P = .9). Only 1 patient in the manual compression group experienced a severe bleeding event (BARC 3). However, no cases of BARC 4 or 5 occurred in any of the closure groups.
Conclusions. The Z-suture and ProGlide methods are safe and efficient for venous occlusion after percutaneous PFO closure compared with manual compression.
Introduction
Venous access plays a crucial role in various interventional cardiology procedures, including percutaneous patent foramen ovale (PFO) closure. The procedure requires 9-French (F) venous access for device delivery, making effective hemostasis after the intervention essential. Traditionally, manual compression has been the standard and safe method for achieving hemostasis following venous access. However, this approach may be associated with potential complications such as puncture site bleedings requiring medical intervention.1 As a result, alternative closure techniques have been explored to enhance patient comfort and optimize post-procedural outcomes. While extensive research exists on closure techniques in arterial access, the evidence regarding their application in venous access procedures, particularly in the context of percutaneous PFO closure, is relatively limited. We hypothesized that both the Z-suture and Perclose ProGlide suture-mediated closure (Abbott) are safe in achieving hemostasis after interventional PFO closure. Additionally, we aimed to evaluate their impact on economic outcomes, including procedural efficiency, hospital costs, and length of stay, to provide a comprehensive assessment of their benefits.
Methods
We conducted a single-center observational study in 220 patients undergoing percutaneous PFO closure from 2021 over a period of 2 years to compare the safety and efficacy of different venous closure techniques. The study conformed to the Declaration of Helsinki and was accepted by the Ethics Committee of the Heinrich-Heine University of Düsseldorf, Germany. Informed consent was obtained from all participants.
Patients aged 18 years or older who were scheduled for PFO closure between 2021 and 2022 were included in this study. The observational study assigned participants to 1 of 3 methods: Z-suture closure, ProGlide SMC; additionally, those patients were compared to manual compression. The allocation of closure technique was based on operator preference, as only 2 interventional cardiologists performed the procedures at our center—one exclusively using the Z-suture technique and the other using ProGlide SMC. Those patients were compared to a cohort undergoing PFO closure by interventional cardiologist fellows who applied manual compression.
The primary endpoint of the study was the occurrence of bleeding events, classified according to the standardized Bleeding Academic Research Consortium (BARC) classification system. Bleeding events classified as BARC 2 or higher were considered clinically significant. Baseline demographic and clinical characteristics, such as age, gender, comorbidities, and procedural details, were collected prospectively. This was a hypothesis-generating explorative analysis; therefore, no sample size calculation was performed. All patients had a peri-interventional ACT of 250 to 350 seconds and were subsequently treated with dual antiplatelet therapy consisting of aspirin and clopidogrel. Hemostasis at the access site was achieved using a single 6F ProGlide device, applied according to the manufacturer's instructions for arterial use. The Z-suture was placed following established standard techniques. Subsequently, all patients were provided with a pressure dressing and a sandbag for compression and instructed to maintain bed rest for 4 hours before mobilization.
Results
A total of 220 patients undergoing percutaneous patent foramen ovale (PFO) closure were included in the study; Z-suture closure was performed in 48 patients, and ProGlide SMC in 53 patients. Additionally, these patients were compared with those who underwent manual compression, which was performed in 119 patients.
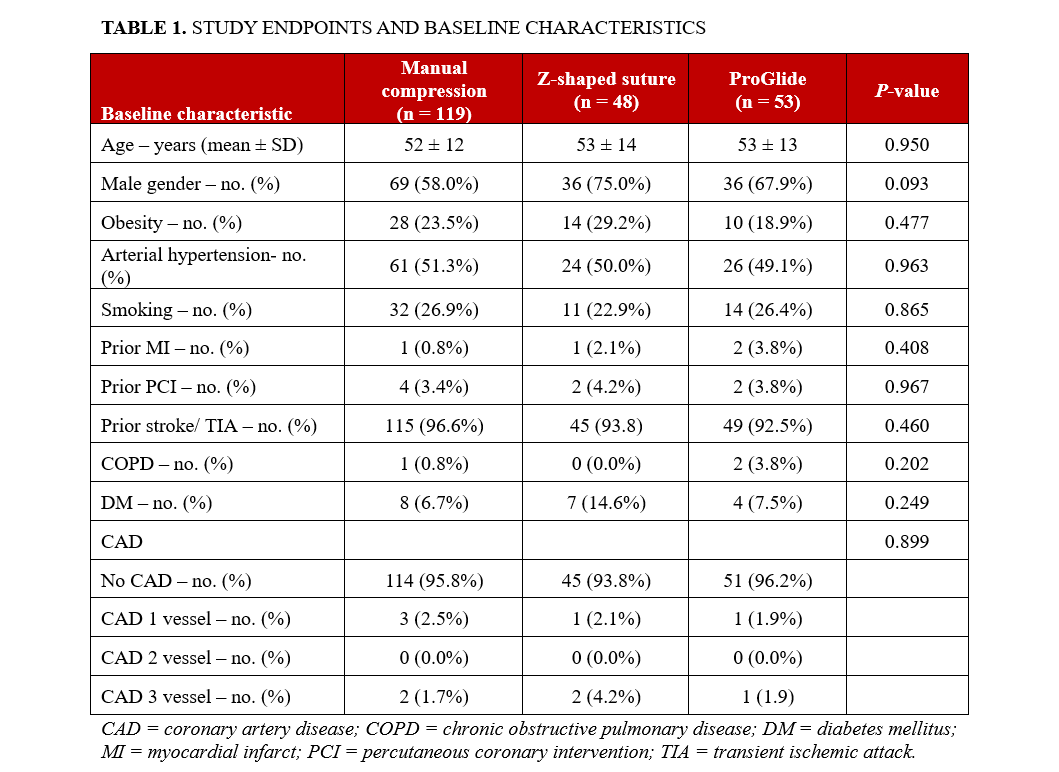
No significant differences were observed between the groups in terms of baseline characteristics, indicating that the study cohorts were well-matched and comparable in demographic and clinical profiles (Table 1).
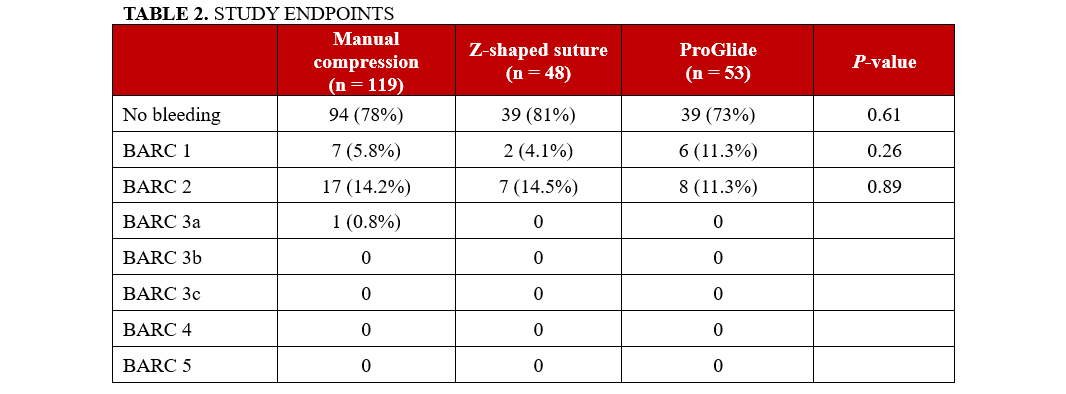
Bleeding events according to the BARC classification system did not show any significant differences between the closure groups. Among the patients who received manual compression, 14.2% (n = 17) experienced BARC bleeding events of 2 or higher. In the Z-suture group, 14.5% (n = 7) of patients had BARC 2 bleeding events of 2 or higher. In the ProGlide group, 15% (n = 8) of patients experienced BARC bleeding events of 2 or higher (P = .9) It is noteworthy that only 1 patient in the manual compression group experienced a severe bleeding event, which was classified as BARC 3. However, no cases of BARC 4 or 5 bleeding occurred in any of the closure groups (Table 2). There were no documented arterio-venous fistulas, access site infections, or pseudoaneurysm in any of the study groups. No statistically significant difference was observed between the 3 groups regarding the duration of hospital stay (manual compression: 1.13 ± 0.88; Z-suture: 1.37 ± 0.93; ProGlide: 1.47 ± 1.35; P =.727).
Discussion
The main finding of our study is that both the Z-suture and ProGlide methods are safe and effective techniques for achieving venous occlusion following percutaneous PFO closure compared with manual compression. Additionally, no significant differences were observed between the Z-suture and ProGlide methods in terms of bleeding complications or efficacy.
Vascular complication and puncture site hematoma represent about 5% of adverse events in patients undergoing interventional PFO closure.2 At the time of this study, data had been published regarding Z-suture vs manual compression in procedures using venous sheaths 10F or larger and ProGlide vs manual compression in patients undergoing percutaneous mitral valve repair.1,3 It was found that, compared with manual compression, the Z-suture effectively achieved hemostasis after 10F to 22F femoral venous sheath removal, enabling faster hemostasis, earlier hospital discharge, and fewer complications.1 Furthermore, ProGlide closure after percutaneous mitral valve repair as compared with manual compression was feasible, safe, and allowed earlier patient mobilization.3 Here, we compared Z-suture and ProGlide closure and found no differences between both closure techniques. However, cost effectiveness is a major topic in medical care, and the Z-suture is substantially cheaper than the ProGlide closure,4 which may be an argument in favor of the Z-suture.
Limitations
While limited by a relatively small sample size, this single-center trial is the first study to directly compare the Z-suture and ProGlide methods against manual compression in an observational setting. It is important to interpret the results in the context of the study design, as the safety of the “Z”-stitch and ProGlide were evaluated against manual compression. Furthermore, femoral vein puncture was not ultrasound-guided, which is now considered state of the art. Additionally, this study focused exclusively on 9F sheaths, and further research is needed to evaluate the performance of these methods with cases involving larger bore sheaths and multiple sheaths.
Conclusions
Both the Z-suture and ProGlide SMC techniques were found to be safe and effective in achieving hemostasis after PFO closure with a 9F sheath. Despite differences in closure methods, there was no statistically significant difference between these approaches in terms of bleeding severity as classified by the BARC system or hospital length of stay. Additionally, manual compression was equally effective in minimizing bleeding events, further supporting the overall safety of all 3 techniques in this specific setting.
Affiliations and Disclosures
Saif Zako, MD1; David Naguib, MD1; Kathrin Klein, MD1; Asena Öz, MD1; Carolin Helten, MD1; Philipp Mourikis, MD1; Daniel Metzen, MD1; Malte Kelm, MD1,2; Tobias Zeus, MD1,2; Amin Polzin, MD1-3
From the 1Department of Cardiology, Pulmonology, and Vascular Medicine, University Hospital Düsseldorf, Medical Faculty of the Heinrich Heine University Düsseldorf, Düsseldorf, Germany; 2Cardiovascular Research Institute Düsseldorf (CARID), Düsseldorf, Germany; 3National Heart and Lung Institute, Imperial College London, London, United Kingdom.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Amin Polzin, Department of Cardiology, Pulmonology, and Vascular Medicine, Heinrich Heine University Medical Center Düsseldorf Moorenstrasse 5, Düsseldorf 40225, Germany. Email: amin.polzin@med.uni-duesseldorf.de
References
1. Pracon R, Bangalore S, Henzel J, et al. A randomized comparison of modified subcutaneous "Z"-stitch versus manual compression to achieve hemostasis after large caliber femoral venous sheath removal. Catheter Cardiovasc Interv. 2018;91(1):105-112. doi:10.1002/ccd.27003
2. Merkler AE, Gialdini G, Yaghi S, et al. Safety outcomes after percutaneous transcatheter closure of patent foramen ovale. Stroke. 2017;48(11):3073-3077. doi:10.1161/STROKEAHA.117.018501
3. Geis NA, Pleger ST, Chorianopoulos E, Müller OJ, Katus HA, Bekeredjian R. Feasibility and clinical benefit of a suture-mediated closure device for femoral vein access after percutaneous edge-to-edge mitral valve repair. EuroIntervention. 2015;10(11):1346-1353. doi:10.4244/EIJV10I11A231
4. Lodhi H, Shaukat S, Mathews A, Maini B, Khalili H. Comparison of figure-of-eight suture and Perclose ProGlide suture-mediated closure in large bore venous access hemostasis: a randomized controlled trial. Am J Cardiol. 2023;209:181-183. doi:10.1016/j.amjcard.2023.09.105





















