Transcatheter Closure of Right Coronary Cusp Aneurysm-to-Right Ventricle Paravalvular Leak in a Patient With Complex Congenital Heart Disease
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
A 41-year-old man with unrepairable pulmonary atresia with ventricular septal defect presented with new onset dyspnea. His medical history included infective endocarditis requiring mechanical aortic valve replacement (AVR) in 2019 and recurrent infective endocarditis complicated with periaortic abscess requiring debridement, pericardial patch repair, and redo-AVR with bioprosthesis in 2022. However, postprocedural imaging revealed a residual right coronary cusp (RCC) aneurysm.
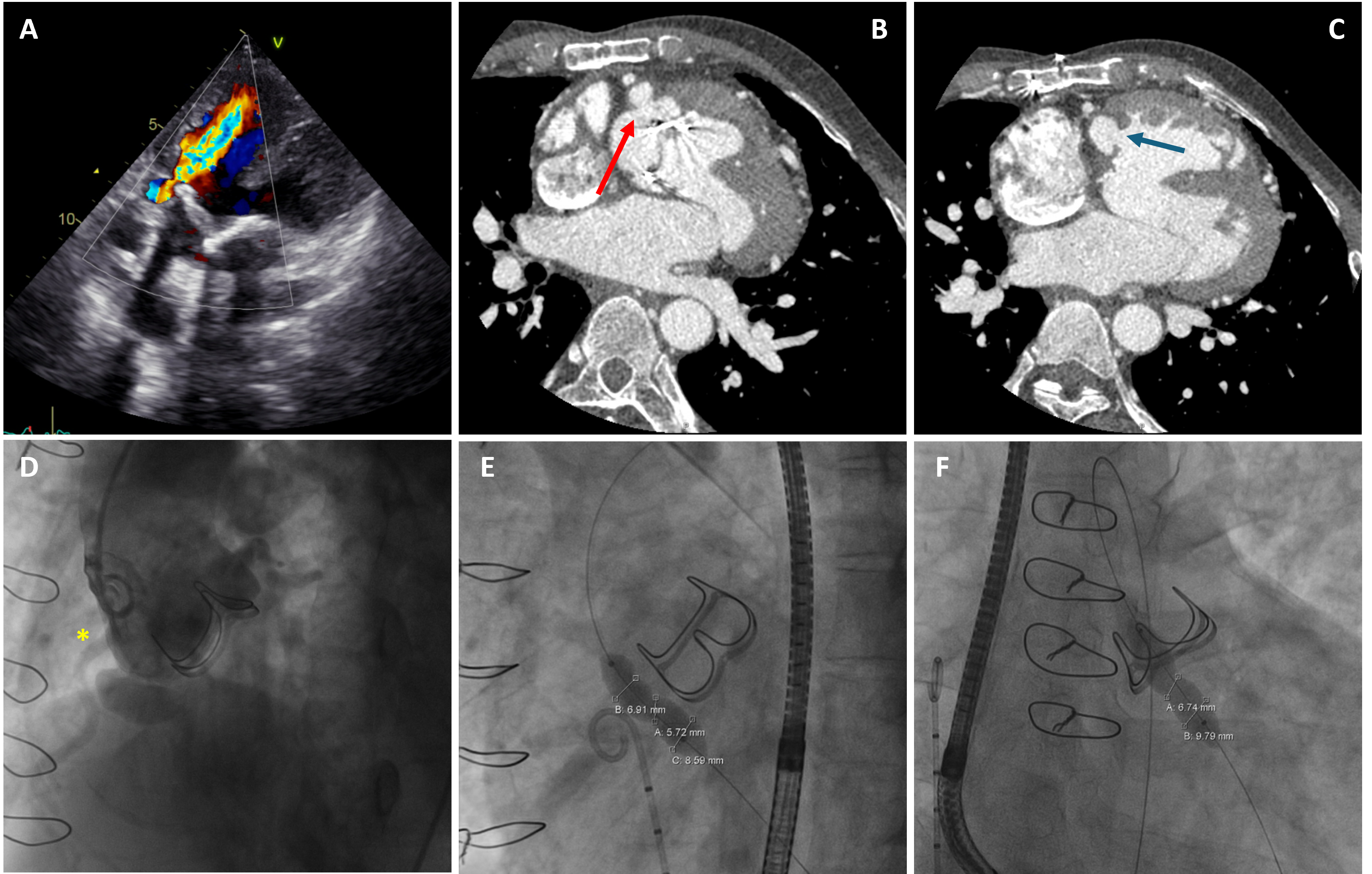
At presentation, transthoracic echocardiography and computed tomography scan confirmed the presence of a perforated RCC aneurysm with diastolic flow into the right ventricle (RV), causing severe aortic paravalvular leak in the context of univentricular physiology, leading to impaired systolic function and exercise tolerance (Figure 1, Video 1). Microbiological workup was unremarkable. In view of the prohibitive surgical risk, transcatheter closure was recommended by the heart team.
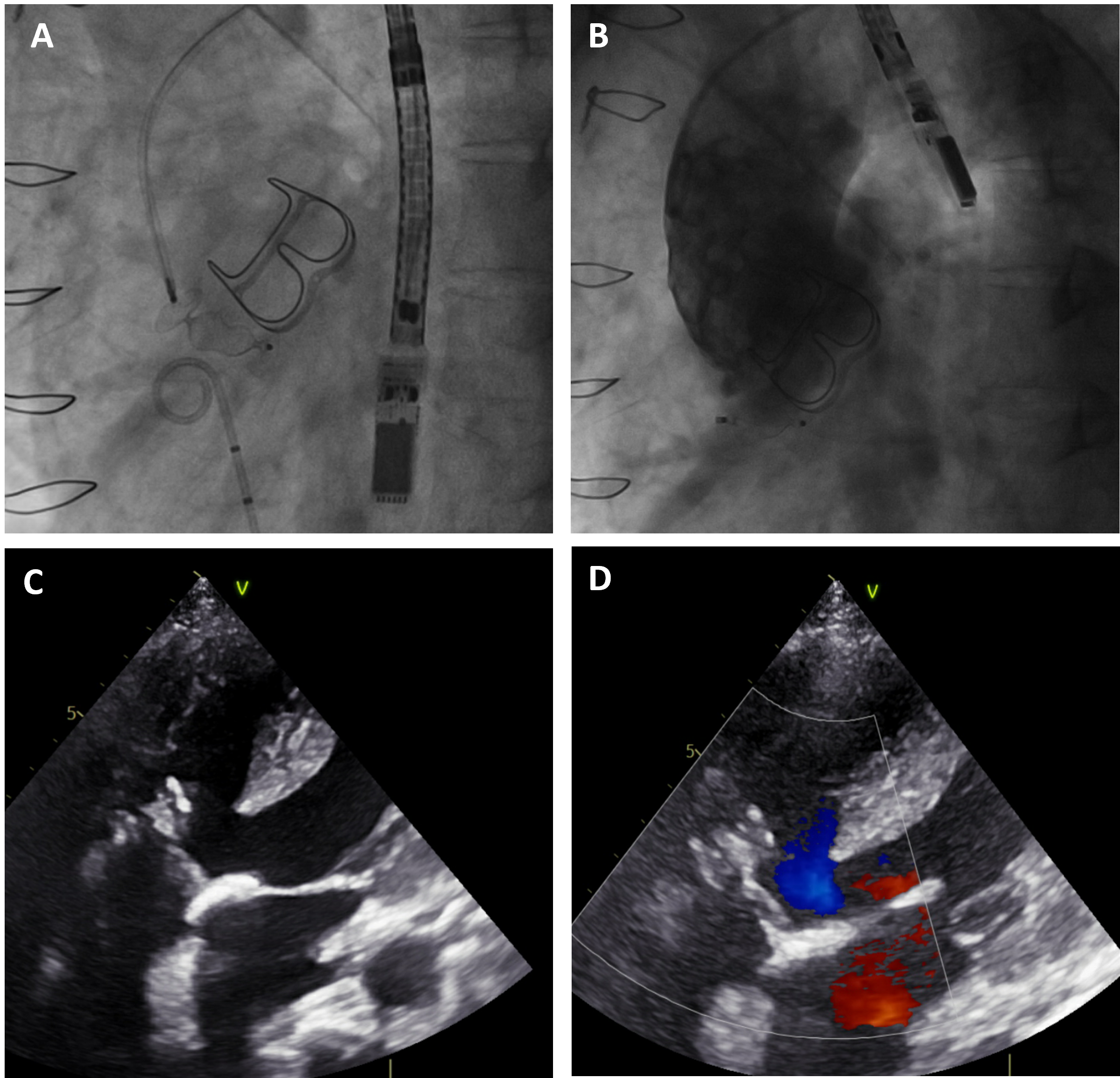
The procedure was performed under local anaesthesia under the guidance of transesophageal echocardiography. Balloon sizing confirmed a 6- to 7-mm waist at the communication neck. A 10-mm Amplatzer Vascular Plug II (Abbott) was successfully deployed, achieving complete occlusion of the paravalvular leak (Figure 2, Video 2). Final imaging demonstrated no residual leak. At follow-up, the patient’s exercise tolerance returned to baseline. Imaging showed normalized ventricular function with no residual leak or signs of infection.
This case highlights a rare complication of prosthetic valve endocarditis—RCC aneurysm-to-RV communication—and demonstrates the feasibility of transcatheter closure as a less invasive option in select high-risk patients.
Affiliations and Disclosures
Tsun-ho Lam, MBBS1,2; Chun-ka Wong, MBBS1,2,3; Cheuk-wing Jonathan Lee, MBBS1,2,4; MBBS; Hay-son Robin Chen, MBBS, MMedSc5; Ka-chun Un, MBBS, MRes1,2
From the 1Cardiology Division, Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong SAR; 2Cardiology Division, Department of Medicine, Queen Mary Hospital, Hong Kong SAR; 3Cambridge Stem Cell Institute, University of Cambridge, United Kingdom; 4Department of Cardiology, Guys’ and St. Thomas’ NHS Foundation Trust, London, United Kingdom; 5Cardiology Unit, Department of Paediatrics and Adolescent Medicine, Hong Kong Children’s Hospital, Hong Kong SAR.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and to the publication thereof. The authors also report that patient consent was provided for publication of the images used herein.
Address for correspondence: Ka-Chun Un, MBBS, MRes, FHKCP, FHKAM(Medicine), FRCP (London), FACC, Cardiology Division, Department of Medicine, Queen Mary Hospital, The University of Hong Kong, Hong Kong SAR, China. Email: drtimothyun@gmail.com; X: @timothy_un




















