Stentless Revascularization of Spontaneous Coronary Dissection Using a Cutting Balloon
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
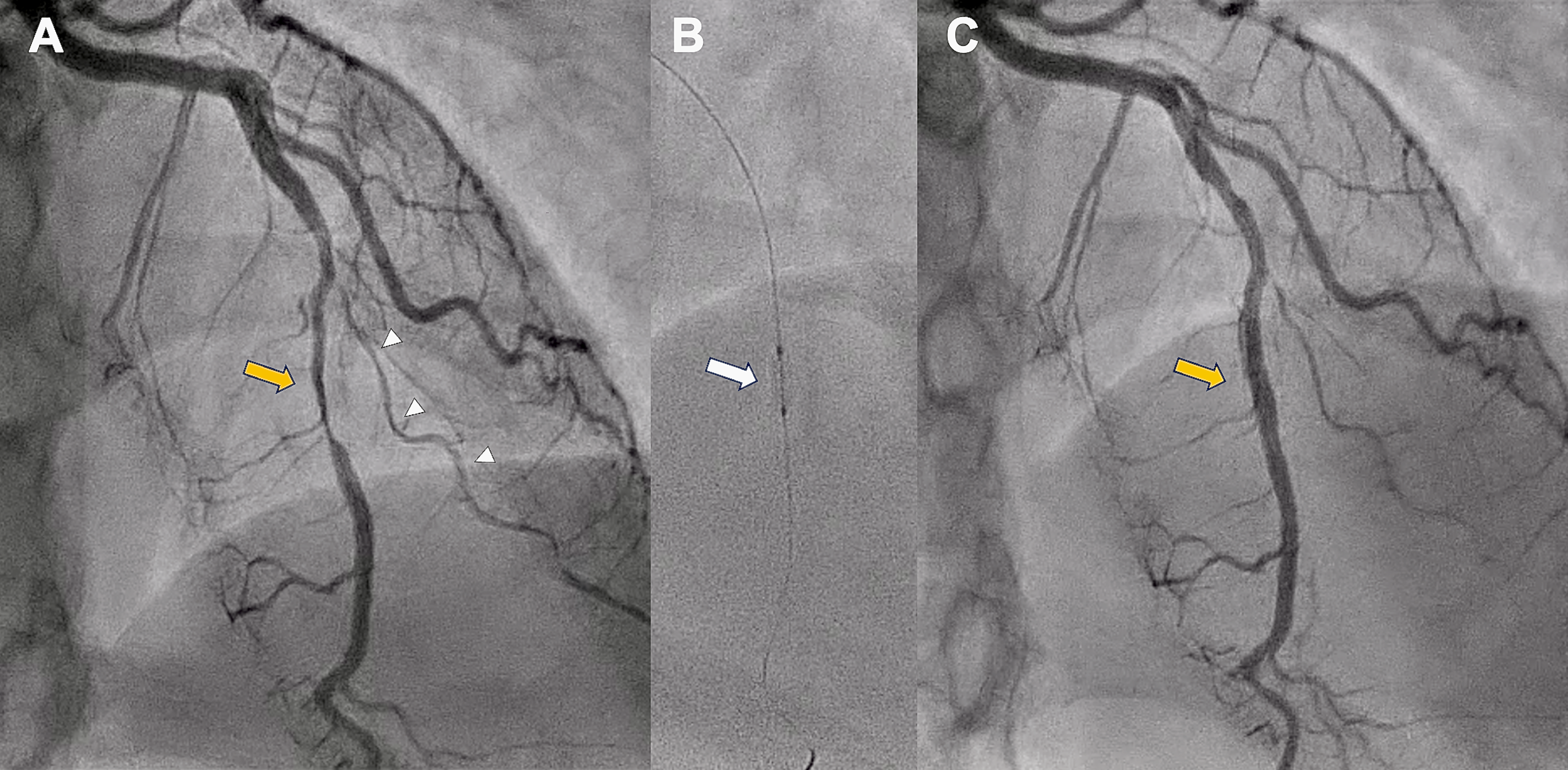
A 37-year-old woman with no prior medical history was admitted with a non-ST-segment elevation myocardial infarction. Despite initial medical therapy, she developed refractory chest pain, T-wave inversion in the precordial leads, and anterior wall akinesia on echocardiography. Emergent coronary angiography revealed a long, smooth, and diffuse narrowing of the mid-left anterior descending artery (LAD), characteristic of type 2 spontaneous coronary artery dissection (SCAD), along with features of type 3 SCAD in a small second diagonal branch (Figure 1A).
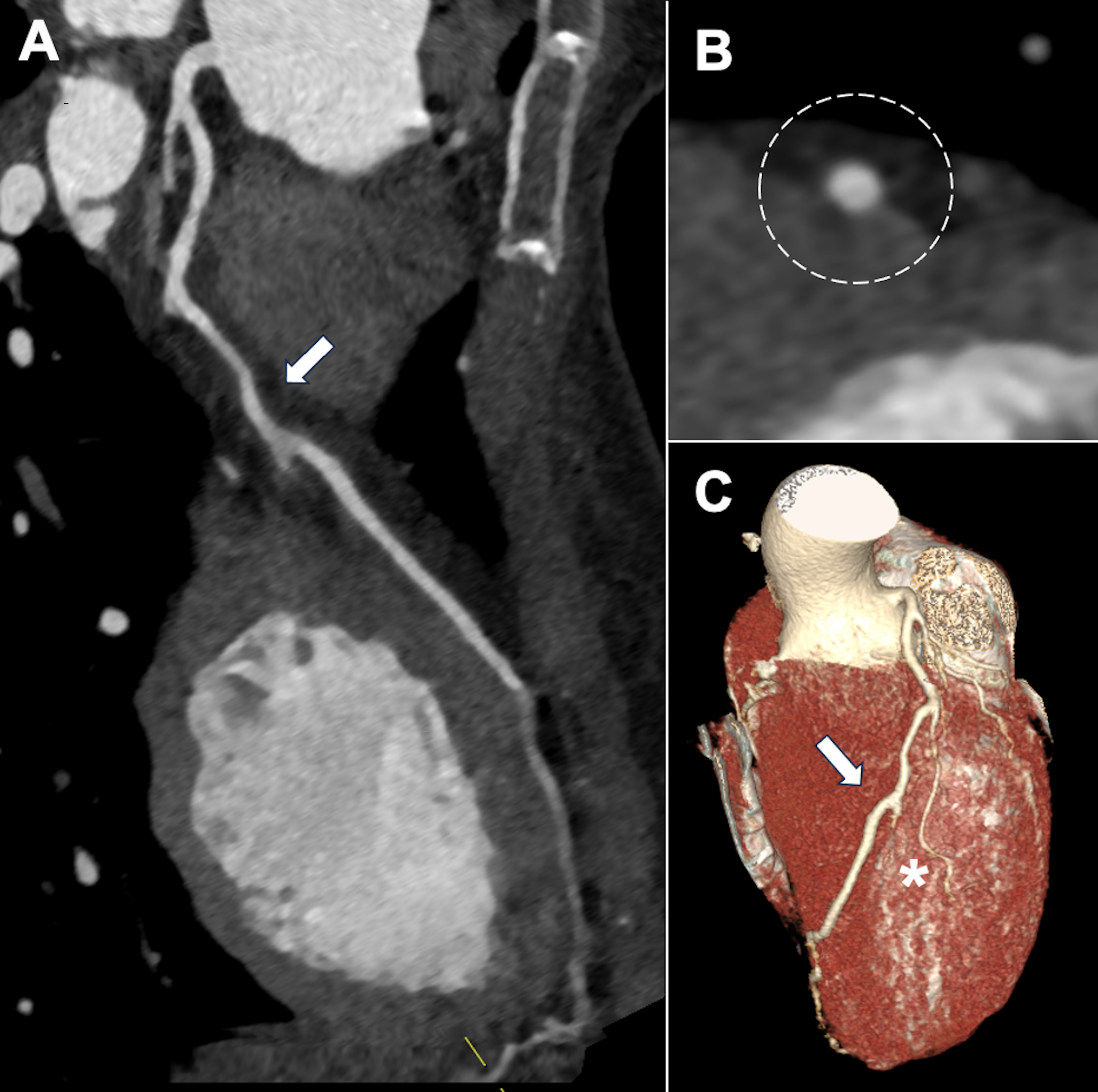
Given ongoing ischemia and hemodynamic stability, a percutaneous coronary intervention was performed with a deliberate stent-avoidance strategy. A cutting balloon was used to fenestrate the intramural hematoma and decompress the false lumen (Figure 1B), achieving full restoration of LAD flow and complete resolution of symptoms (Figure 1C). No stents were implanted. Coronary computed tomography angiography before discharge confirmed a patent LAD without intramural hematoma or atherosclerosis (Figure 2).
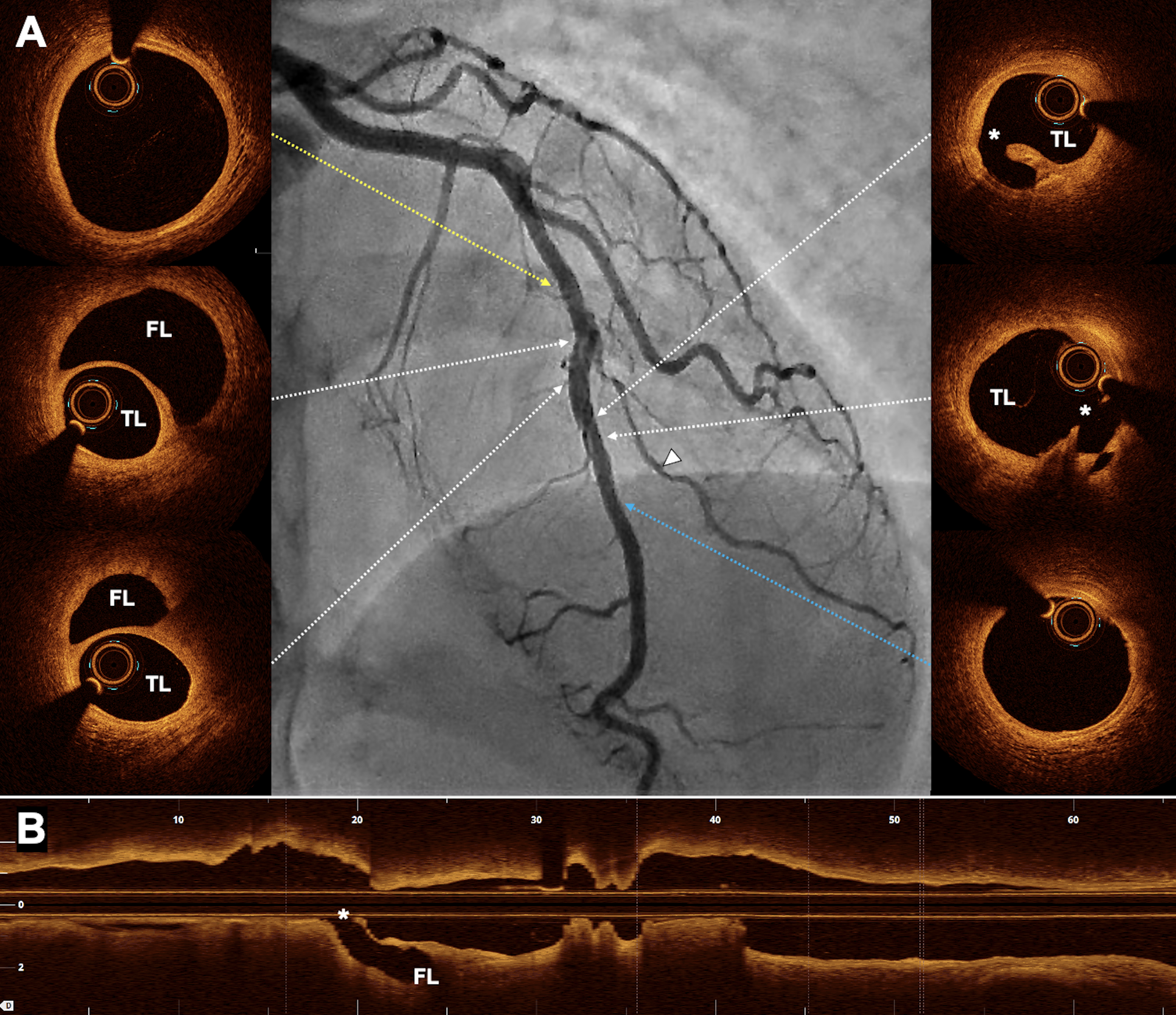
At the 1-month follow-up, repeat angiography demonstrated sustained LAD patency, with a faint radiolucent line across the previously treated segment and spontaneous healing of the diagonal branch (Figure 3; center). Optical coherence tomography revealed the intimal tear caused by the cutting balloon and the residual false lumen without compromise of flow (Figure 3). As the patient remained asymptomatic, conservative follow-up was adopted.
SCAD is generally treated conservatively because spontaneous healing occurs in most cases. However, intervention is warranted in selected scenarios, such as ongoing ischemia, hemodynamic compromise, or high-risk anatomy. In this young patient, the presence of refractory chest pain and anterior wall motion abnormalities justified a revascularization attempt. In certain cases, balloon angioplasty enables vessel decompression and flow restoration without the need for stent implantation, providing an optimal balance between therapeutic efficacy and long-term vessel preservation.
Affiliations and Disclosures
Kristian Rivera, MD1,2; Humberto Coimbra, MD1; Diego Fernández-Rodríguez, MD, PhD1,2; Eva Pueo, MD1; Mireia Martínez, MD1; Juan Casanova-Sandoval, MD, PhD1,2
From the 1Department of Cardiology, Arnau de Vilanova University Hospital, Lleida, Spain; 2Grup de Fisiologia i Patologia Cardíaca, Institut de Recerca Biomèdica de Lleida Fundació Dr. Pifarré, IRBLleida, Lleida, Spain.
Disclosures: The authors report that they have no financial relationships or conflicts of interest with respect to the content herein.
Consent statement: This article was conducted in accordance with local ethics committee regulations and the Declaration of Helsinki for experiments involving humans. The patient provided his signed informed consent for publication.
Address for correspondence: Kristian Rivera, MD, Arnau de Vilanova University Hospital, Av. Alcade Rovira Roure 80, Lleida 25198, Spain. Email: psrivera.lleida.ics@gencat.cat; X: @NoReflow




















