“Olive Sign” During Transcatheter Aortic Valve Implantation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00219. Epub September 3, 2025.
A 67-year-old woman with a 6-month history of chest discomfort was admitted to our center. Transthoracic echocardiogram revealed severe aortic stenosis (AS), and the patient was subsequently accepted for transcatheter aortic valve implantation (TAVI). Based on preoperative computed tomography and echocardiogram measurements along with balloon dilation angiography results, a Venus A23 prosthetic valve (Peijia Medical) was selected.
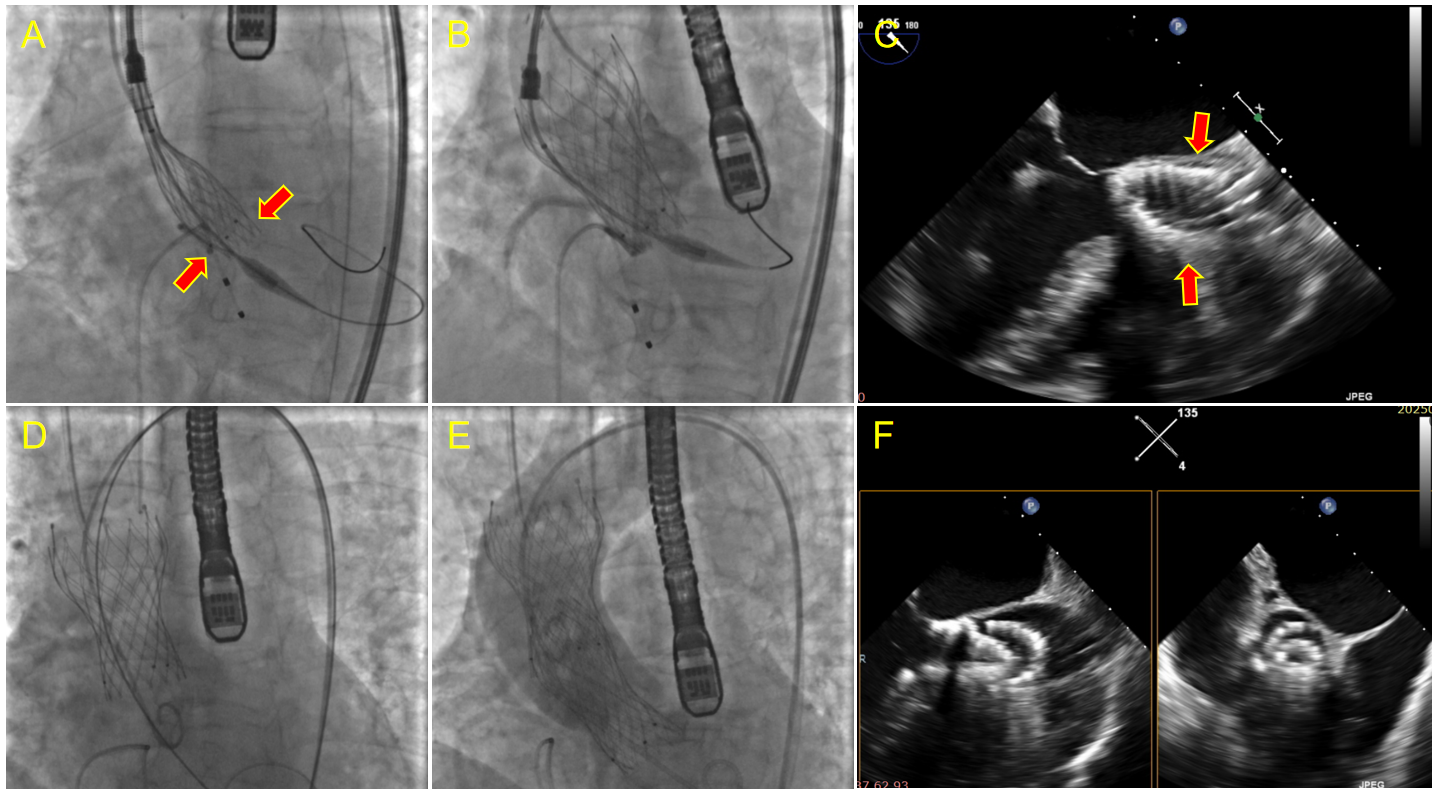
During the deployment, subvalvular stent compression was observed (Figure A). After the valve was deployed (Figure B), transesophageal echocardiogram (TEE) showed an olive-shaped deformation (Figure C). Immediately after the catheter delivery system was withdrawn, the valve migrated into the ascending aorta (Figure D). Subsequently, we decided to adopt a valve-in-valve (ViV) strategy, and the second valve (a Venus A23) was progressively deployed to achieve a tandem configuration with the first valve (Figure E and F). Both the left and right coronary artery ostia remained unobstructed, and only mild aortic regurgitation was noted.
To the best of our knowledge, we are the first to report an “olive sign” under TEE during TAVI, characterized by an olive-shaped deformation of the valve stent immediately after prosthetic valve deployment. This sign indicates subvalvular stent compression, resulting in valve instability and potential migration into the ascending aorta. The underlying mechanism may involve unevenly distributed calcification, causing the valve stent to establish focal rather than circumferential contact with the annulus.
Affiliations and Disclosures
Dawei Lin, MD, PhD; Lei Zhang, MD; Wei Li, MD; Wenzhi Pan, MD, PhD; Daxin Zhou, MD, PhD
From the Department of Cardiology, Zhongshan Hospital, Fudan University, National Clinical Research Center for Interventional Medicine, Shanghai, China.
Dr Lin and Dr Zhang contributed equally to this work.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Funding: Shanghai Clinical Research Center for Interventional Medicine (No.19MC1910300) and National Natural Science Foundation of China (82270377).
Data availability statement: The data underlying this article will be shared upon reasonable request to the corresponding author.
Consent statement: The patient was informed about the potential risks of the operation and signed informed consent forms.
Address for correspondence: Daxin Zhou, MD, PhD, Zhongshan Hospital, Fudan University, 180 Fenglin Road, Shanghai 200032, China. Email: daxin_zhou@163.com




















