Non-Invasive Imaging-Guided Transcatheter Closure of Aorto-Right Atrial Shunt in a Young Man
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
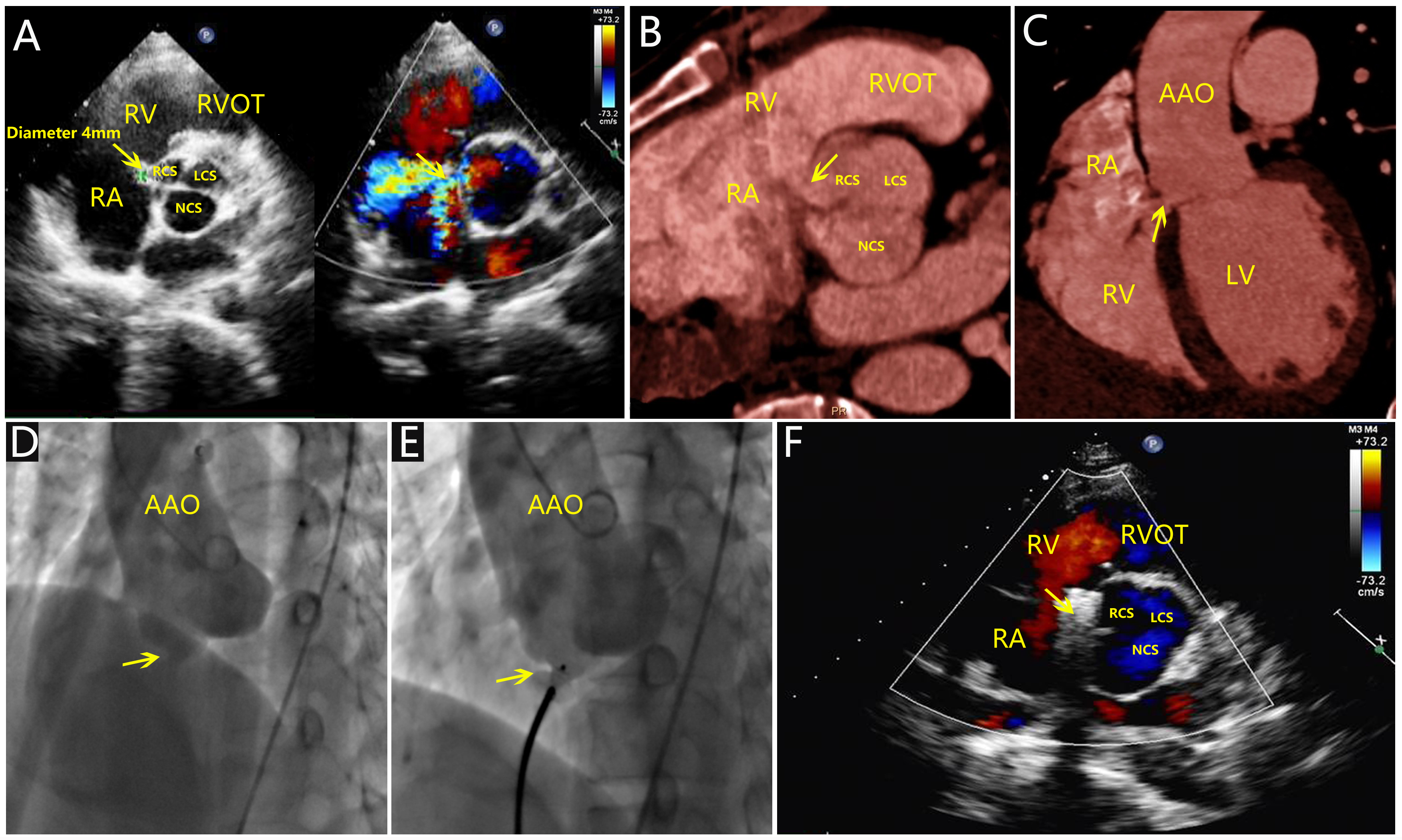
A 31-year-old man presented to our cardiac center with progressive dyspnea and fatigue. Physical examination revealed a continuous 3/6 systolic murmur at the lower left sternal border. Electrocardiography showed sinus tachycardia, while routine laboratory tests were normal. Transthoracic echocardiography (TTE) identified a 4-mm echo-free structure extending from the right coronary sinus into the right atrium. Color Doppler demonstrated a high velocity left-to-right shunt with peak velocity of 6.2 m/s and pressure gradient of 155 mm Hg, suggestive of aorto-right atrial fistula (Figure A). Contrast-enhanced computed tomography (CT) confirmed a ruptured right sinus of Valsalva aneurysm, with the defect located greater than 2 mm from the right coronary artery and aortic valve annulus (Figure B and C), indicating suitability for transcatheter closure.
The patient underwent successful percutaneous closure using a waist-shaped Cera VSD Occluder (Lifetech Scientific) (Figure D and E, Videos 1 and 2). Immediate post-procedural TTE showed complete elimination of the shunt with no residual flow or complications (Figure F). He was discharged 3 days post-procedure and resumed full-time work within 3 months.
This case demonstrates that transcatheter closure is a safe, effective, and minimally invasive option for managing ruptured sinus of Valsalva aneurysm in anatomically suitable young patients. Multimodality imaging—particularly echocardiography and CT—is essential for accurate diagnosis and procedural planning. Compared with surgical repair, catheter-based intervention reduces trauma, accelerates recovery, and supports rapid reintegration into daily life.
Affiliations and Disclosures
Jie Wang, MD1; Ping Hu, MD2; Ya-Feng He, MD2; Xiao-Jing Ma, PhD2
From the Departments of 1Radiology and 2Echocardiography, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology, Hankou District, Wuhan, China.
Dr Wang, Dr Hu, and Dr He served as co-first authors.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Funding: This work was funded by the Wuhan Clinical Medical Research Center for Cardiovascular Imaging and the Open Fund of Imaging Center (Project No. CMRC202302).
Data availability statement: The data that support the findings of this study are available from the corresponding author.
Consent statement: This report has obtained the patient's informed consent for the publication of their anonymized clinical data.
Address for correspondence: Xiao-Jing Ma, PhD, Department of Echocardiography, Wuhan Asia Heart Hospital Affiliated Wuhan University of Science and Technology, No 753 Jinghan Road, Hankou District, Wuhan 430022, China. Email: ma312312ma@163.com




















