Live Three-Dimensional Multiplanar-Reconstruction for Advanced Guidance of Transcatheter Tricuspid Valve-in-Valve Procedure
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00194. Epub September 5, 2025.
The recent increase in volume of transcatheter tricuspid valve (TV) replacements, along with the intrinsic TV anatomical complexities, has stimulated the development of intraprocedural imaging techniques. Transesophageal echocardiography (TEE), fluoroscopy, and intracardiac echo (ICE) are the cornerstone of imaging guidance for TV interventions. Multiplanar reconstruction (MPR) of 3-dimensional (3D) volume datasets improves spatial orientation within the heart and allows for the visualization of cardiac structures in multiple simultaneous planes. This better understanding of 3D relationships helps with intraprocedural guidance of complicated percutaneous TV interventions.1,2
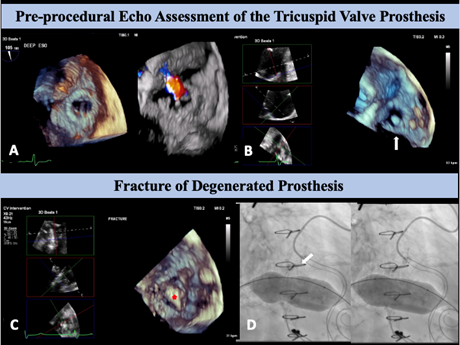
A 65-year-old woman with a past medical history of rheumatic heart disease underwent mechanical mitral and aortic valve replacements in 1992 followed by a 27-mm Epic tricuspid valve (Abbott) replacement in 2018 for treatment of severe tricuspid regurgitation. She presented with complaints of lower leg edema with ascites, and TEE revealed a degenerated tricuspid bioprosthesis from mixed regurgitation and stenosis (Figure A-C, Video 1). The heart team deemed her at extreme risk for the third open-heart surgery and referred her for a transcatheter tricuspid valve-in-valve (TVIV) procedure.
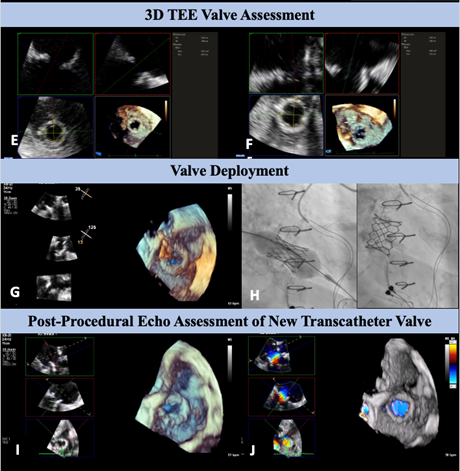
In this case, live-MPR was complementary to fluoroscopy and enabled advanced guidance of the TVIV procedure, allowing us to follow the fracture of the degenerated bioprosthesis (Figure D-E; Video 2), to assess wire positioning across the valve, and to confirm the final deployment and absence of paravalvular leak (Figure F-J; Video 3). Live-MPR also allowed for less probe manipulation and thereby reduced esophageal injury risk.
Affiliations and Disclosures
Giulia Passaniti, MD1,2; Sahil Khera, MD, MPH1; Rajeev R. Samtani, MD1; Stamatios Lerakis, MD1; Gilbert H. L. Tang, MD, MSc, MBA1,3; Lucy M. Safi, DO1
From the 1Division of Cardiology, Mount Sinai Heart Fuster Hospital, Icahn School of Medicine at Mount Sinai, New York, New York; 2Centro Alte Specialità e Trapianti, Policlinico “G. Rodolico-San Marco” University of Catania, Catania, Italy; 3Department of Cardiovascular Surgery, Mount Sinai Health System, Mount Sinai Heart Fuster Hospital, Icahn School of Medicine at Mount Sinai, New York, New York.
Disclosures: Dr Khera is a consultant and proctor for Medtronic and Abbott Structural Heart, a consultant for Terumo and W. L. Gore & Associates, a consultant for and advisory board member of East End Medical, and serves on the speaker’s bureau for Zoll Medical and Edwards Lifesciences. Dr Tang has received speaker's honoraria from, and served as a physician proctor, consultant, advisory board member, TAVR publications committee member, RESTORE study steering committee member, APOLLO trial screening committee member, and IMPACT MR steering committee member for Medtronic; has received speaker's honoraria from, and served as a physician proctor, consultant, advisory board member, and TRILUMINATE trial anatomic eligibility and publications committee member for Abbott Structural Heart; has served as an advisory board member for Boston Scientific; has served as a consultant and physician screening committee member for Shockwave Medical; has served as a consultant for Philips and Edwards Lifesciences, Peija Medical, and Shenqi Medical Technology; and has received speaker's honoraria from Siemens Healthineers. Dr Safi has received speaker honoraria from Abbott and Medtronic and served on advisory board for Triclip. The remaining authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and to the publication, including any and all images.
Address for correspondence: Lucy M. Safi, DO, FACC, FASE, FSCAI, Icahn School of Medicine, Mount Sinai Fuster Heart Hospital, 1468 Madison Ave, New York, NY 10029, USA. Email: Lucy.Safi@MountSinai.org; X: @LucySafi, @GilbertTangMD, @Khera_MD, @PassanitiGiulia
References
1. Hahn RT, Nabauer M, Zuber M, et al. Intraprocedural imaging of transcatheter tricuspid valve interventions. JACC Cardiovasc Imaging. 2019;12(3):532-553. doi:10.1016/j.jcmg.2018.07.034
2. Wollborn J, Schuler A, Sheu RD, Shook DC, Nyman CB. Real-time multiplanar reconstruction imaging using 3-dimensional transesophageal echocardiography in structural heart interventions. J Cardiothorac Vasc Anesth. 2023;37(4):570-581. doi:10.1053/j.jvca.2022.11.011




















