Large Radial Artery Pseudoaneurysm Following Diagnostic Coronary Angiography
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
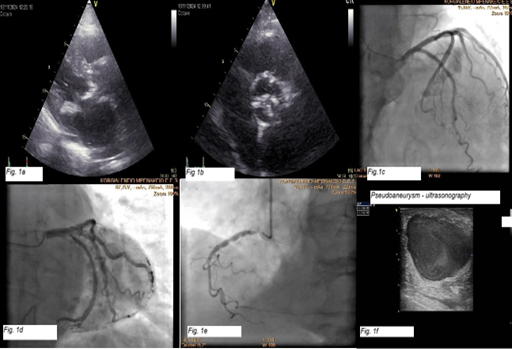
An 81-year-old woman was admitted with dyspnea and irregular heartbeat due to atrial fibrillation with a rapid ventricular response. Echocardiography showed preserved left ventricular ejection fraction, severe aortic stenosis (paradoxical low flow-low gradient), and moderate mitral stenosis (Figure 1A and B). Coronary angiography revealed no significant coronary artery disease (Figure 1C-E).
Radial access was used, and hemostasis was achieved using a radial artery compression device. Following clinical improvement, the patient was discharged on acenocoumarol (target internalized ratio: 2-3), bisoprolol, furosemide, and eplerenone.
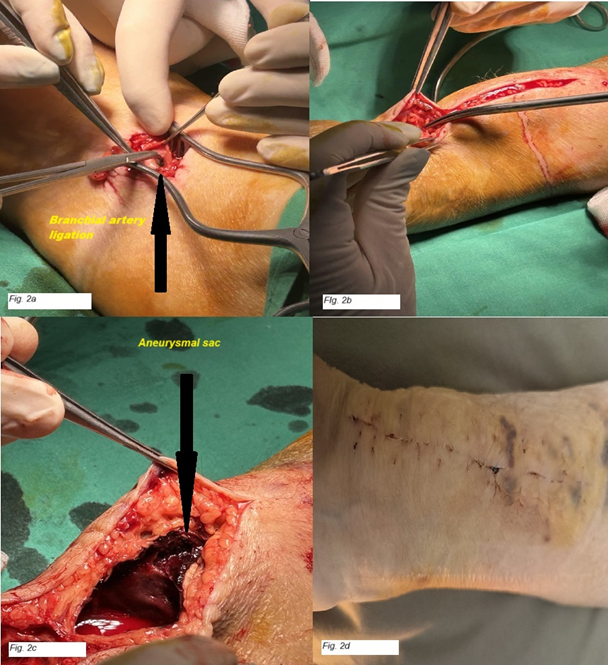
Two weeks later, a soft, painless, non-inflammatory mass was noted at the radial puncture site. Doppler ultrasound revealed a 3.9 × 2.3-cm pseudoaneurysm with turbulent flow (Figure 1F, Video). Ultrasound-guided compression was attempted but was unsuccessful because of the size of the lesion. Surgical consultation was sought, and the pseudoaneurysm was excised following brachial artery control and radial artery ligation. The patient's postoperative recovery was uneventful, and full healing was confirmed at the 2-week follow-up (Figure 2).
The radial artery is now the preferred access site for coronary procedures, offering lower risks of bleeding and vascular complications than femoral access.1,2 However, rare complications may still occur, including pseudoaneurysm formation.3,4 Radial pseudoaneurysms are infrequent (0.03%-0.09%) but should be suspected when a pulsatile mass develops post-procedure. Risk factors include older age, multiple punctures, anticoagulation, and insufficient compression.3,4 Diagnosis is confirmed via Doppler ultrasound. Management depends on size and symptoms. Small, stable pseudoaneurysms may be treated minimally with thrombin ejection,5 and percutaneous treatment with covered stents may be an alternative in select cases.6 Larger pseudoaneurysms require surgical treatment.7,8
This case highlights a rare vascular complication of transradial access. Prompt recognition and appropriate management are essential to avoid serious adverse outcomes.
Affiliations and Disclosures
Ioannis Papadopoulos, MD1; Konstantinos Filippou, MD1; Athanasios Papadopoulos, MD2; Panagiotis Varelas, MD1; Dafni Pitsiori, MD2; Konstantinos Manousopoulos, MD, PhD1; Dimitrios Karelas, MD1; Theofanis Pappas, MD, PhD3; Nikolaos Giannakopoulos, MD3; Konstantinos Nakas, MD3; Dimitra Manou, MD3; Ioannis Tsiafoutis, MD, PhD1
From the 1Hemodynamic Laboratory, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, Athens, Greece; 22nd Cardiology Department, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, Athens, Greece; 3Vascular Surgical Department, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, Athens, Greece.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The author/s confirm that written consent for submission and publication of this case report, including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Address for correspondence: Konstantinos Filippou, MD, Hemodynamic Department, General Hospital GHA Korgialeneio Mpenakeio-Hellenic Red Cross, 11145 Nikolaidou Street, Athens 11526, Greece. Email: filippakos.kos@gmail.com
References
- Chiarito M, Cao D, Nicolas J, et al. Radial versus femoral access for coronary interventions: an updated systematic review and meta-analysis of randomized trials. Catheter Cardiovasc Interv. 2021;97(7):1387-1396. doi:10.1002/ccd.29486
- Fazel R, Rao SV, Cohen DJ, et al. Temporal trends and clinical outcomes with radial versus femoral arterial access for percutaneous coronary intervention in the United States. J Soc Cardiovasc Angiogr Interv. 2024;3(5)(Supplement):101866. doi:10.1016/j.jscai.2024.101866
- Sandoval Y, Bell MR, Gulati R. Transradial artery access complications. Circ Cardiovasc Interv. 2019;12(11):e007386. doi:10.1161/CIRCINTERVENTIONS.119.007386
- Roy S, Kabach M, Patel DB, Guzman LA, Jovin IS. Radial artery access complications: prevention, diagnosis and management. Cardiovasc Revasc Med. 2022;40:163-171. doi:10.1016/j.carrev.2021.12.007
- Moussa Pacha H, Alraies MC, Soud M, Bernardo NL. Minimally invasive intervention of radial artery pseudoaneurysm using percutaneous thrombin injection. Eur Heart J. 2018;39(3):257. doi:10.1093/eurheartj/ehx592
- Tsiafoutis I, Zografos T, Koutouzis M, Katsivas A. Percutaneous endovascular repair of a radial artery pseudoaneurysm using a covered stent. JACC Cardiovasc Interv. 2018;11(11):e91-e92. doi:10.1016/j.jcin.2018.03.047.
- Collins N, Wainstein R, Ward M, Bhagwandeen R, Dzavik V. Pseudoaneurysm after transradial cardiac catheterization: case series and review of the literature. Catheter Cardiovasc Interv. 2012;80(2):283-287. doi:10.1002/ccd.23216
- Cunha R, Silva M, Henrique A, et al. Pseudoaneurysm of radial artery after coronary angiography. J Surg Case Rep. 2023;2023(8):rjad446. doi:10.1093/jscr/rjad446




















