Intravascular Ultrasound-Detected Intimal Flap Predicts Acute Diagonal Branch Occlusion After Drug-Eluting Stent Implantation
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00230. Epub August 27, 2025.
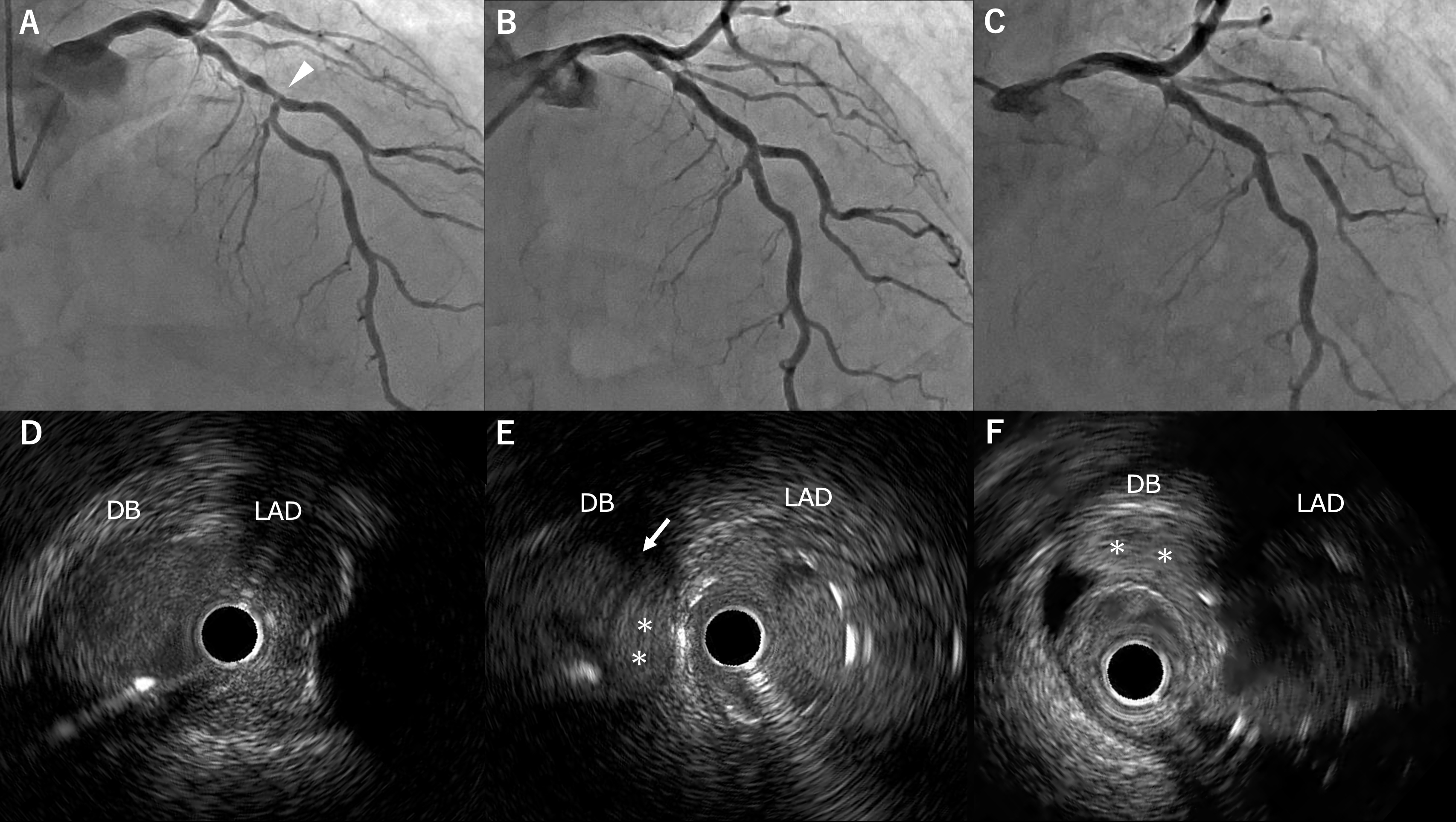
An 81-year-old man with prior myocardial infarction underwent follow-up coronary angiography, which showed severe mid-left anterior descending artery (LAD) stenosis with the first diagonal branch arising from the lesion (Figure A). Percutaneous coronary intervention was performed with diagonal branch protection. After predilatation and drug-eluting stent implantation, angiography showed Thrombolysis in Myocardial Infarction (TIMI)-3 flow (Figure B), but intravascular ultrasound (IVUS) revealed an intimal flap and small hematoma at the diagonal branch ostium (Figure E, Video 1). Shortly after transfer to recovery, the patient developed chest pain with ST-segment elevation. Emergent angiography demonstrated sub-occlusion of the diagonal branch (Figure C), and IVUS confirmed a large hematoma extending from the branch orifice (Figure F, Video 2). A drug-eluting stent was successfully deployed in the diagonal branch, restoring TIMI-3 flow.
Although side-branch occlusion after main-vessel stenting is uncommon, it can lead to serious complications such as myocardial infarction or arrhythmia. This case illustrates that IVUS can identify intimal dissection or hematoma—lesions that may not be apparent angiographically—and thereby predict imminent branch occlusion. When IVUS reveals side-branch injury, adjunctive strategies such as bail-out stenting or cutting-balloon fenestration should be considered.
Affiliations and Disclosures
Tatsuo Yokomine, MD1,2; Yuito Enokida, MD1; Takashi Kajiya, MD1; Tatsuro Takei, MD1; Toshiko Ninomiya, MD1; Nobuhiko Atsuchi, MD, PhD1; Mitsuru Ohishi, MD, PhD2
From the 1Department of Cardiology, Tenyoukai Central Hospital, Kagoshima, Japan; 2Department of Cardiovascular Medicine and Hypertension, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima, Japan.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the interventions described in the manuscript and for the publication thereof, including any and all images.
Address for correspondence: Takashi Kajiya, MD, FACC, FESC, Department of Cardiology, Tenyoukai Central Hospital, Izumi-cho 6-7, Kagoshima 892-0822, Japan. Email: t_kajiya@hotmail.com




















