The Hidden Threat: Masked Coronary Artery Perforation Due to Coronary No-Reflow
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
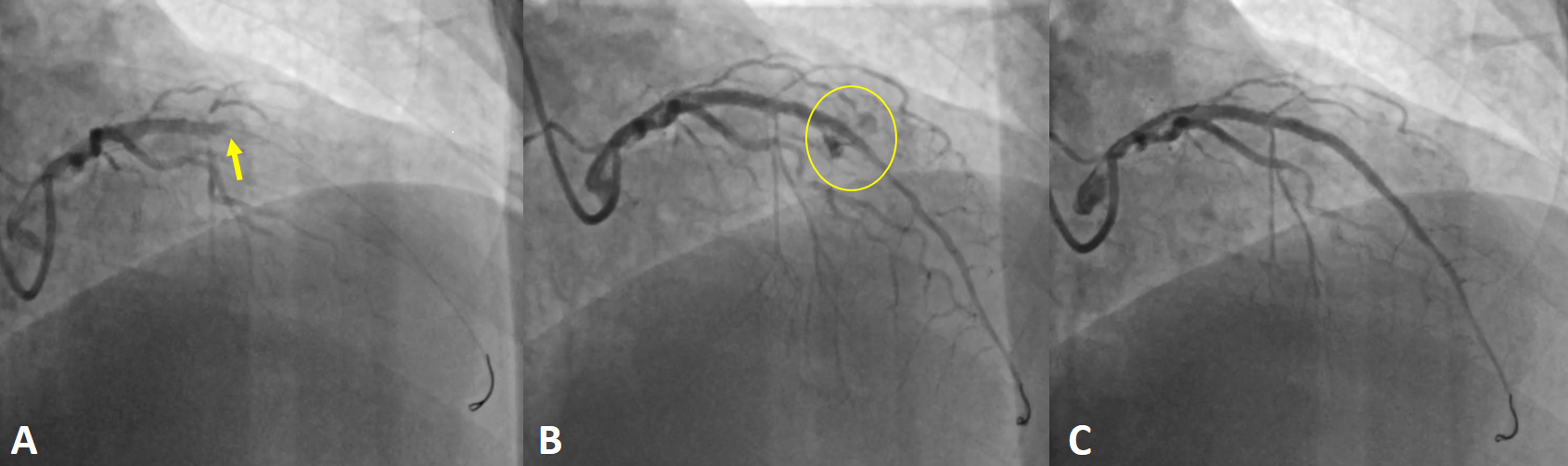
A 58-year-old man presented to the emergency department with chest pain consistent with angina. Electrocardiography revealed no ischemic changes; however, serial troponin measurements showed a rising trend. He was diagnosed with non-ST-elevation myocardial infarction and admitted to the coronary intensive care unit. Coronary angiography revealed a critical lesion in the left anterior descending artery (LAD), prompting immediate percutaneous coronary intervention (PCI) (Figure A). Following predilation, a 3.0 × 28-mm drug-eluting stent was deployed, and post-dilation was performed with a 3.5 × 15-mm noncompliant balloon. Shortly after, contrast injection revealed a no-reflow phenomenon in the LAD (Figure A, Video 1). Intracoronary adenosine and tirofiban were administered, with the patient remaining hemodynamically stable. Coronary flow was successfully restored. However, further imaging revealed an Ellis class III coronary perforation distal to the stent (Figure B, Video 2). Transthoracic echocardiography showed no pericardial effusion. Given the stable clinical status, a covered stent was successfully placed to seal the perforation (Figure C, Video 3). The patient remained asymptomatic during follow-up and was discharged with optimized medical therapy.
The no-reflow phenomenon remains one of the most challenging complications during PCI. It is defined as reduced coronary flow in the absence of mechanical obstruction, typically due to microvascular dysfunction, distal embolization, or reperfusion injury. Standard pharmacologic agents such as intracoronary adenosine, nitroprusside, calcium channel blockers, and glycoprotein IIb/IIIa inhibitors are recommended to restore microvascular flow. Importantly, persistent no-reflow can mask underlying mechanical complications such as coronary perforation. In this case, successful restoration of flow allowed identification and management of a life-threatening perforation. Clinicians should be cautious in interpreting no-reflow and should aim to re-establish flow to avoid missing critical complications.
Affiliations and Disclosures
Burcu Kodal, MD; Tahir Bezgin, MD; Aziz Inan Celik, MD
From the Department of Cardiology, Heart Center, Gebze Fatih State Hospital, Kocaeli, Turkey.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient(s) for the intervention(s) described in the manuscript and for the publication of thereof, including any and all images.
Address for correspondence: Burcu Kodal, MD, Department of Cardiology, Gebze Fatih State Hospital, Heart Center Osman Yilmaz Neighborhood, Istanbul Street, 127, Kocaeli 41400, Turkey. Email: burcu_kodal@hotmail.com




















