A Giant Right Coronary Artery Pseudoaneurysm Successfully Managed With a Covered Stent
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
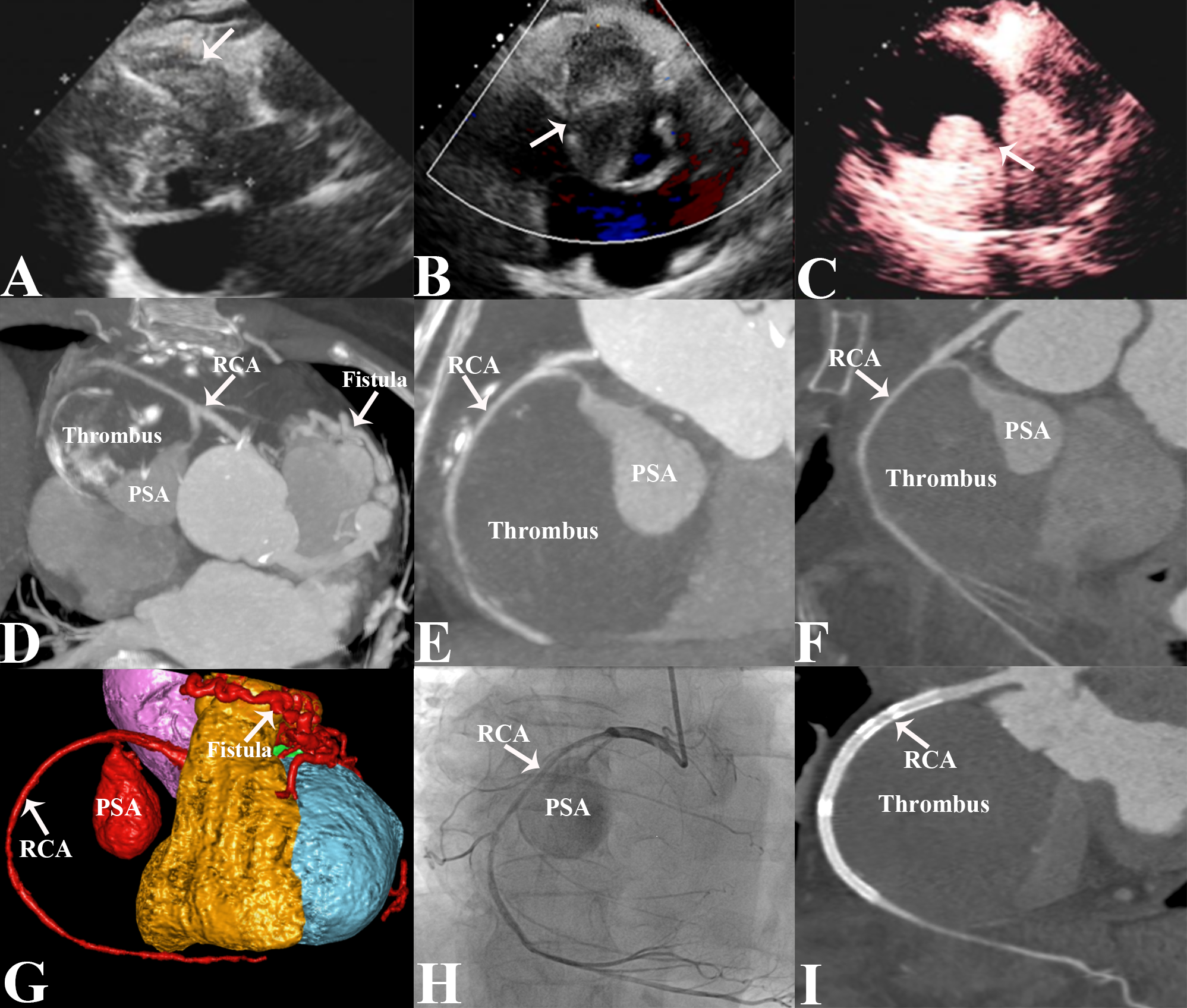
An 80-year-old woman presented with intermittent dizziness and discomfort for 1 month. Electrocardiogram revealed atrial flutter, with bidirectional or inverted T-wave in leads II, III, aVF, and V2-V6. Transthoracic echocardiography (TTE) revealed a hyperechoic and heterogeneous mass with anechoic areas in the right atrioventricular groove (Figure A). Color Doppler blood flow imaging showed no obvious blood flow signal within the mass (Figure B). Left ventriculography demonstrated a filling defect of the solid structure of the mass and contrast agent filling in the anechoic area (Figure C). Computed tomographic angiography (CTA) revealed bilateral coronary artery-pulmonary artery fistulas and a giant pseudoaneurysm (PSA) in the proximal segment of the right coronary artery (RCA), with massive mural thrombus and eggshell calcification at the edge, which compressed the right heart chambers and right coronary artery (RCA) (Figure D-F). A volume-rendering CTA image provided an intuitive view of the PSA with the coronary fistulas (Figure G). Coronary angiography (CAG) revealed the PSA arising from the proximal RCA with severe stenosis of RCA (Figure H, Video).
The patient underwent a percutaneous procedure using 3 overlapping Firebird drug-coated stents sized 2.75 x 33mm, 3.0 x 33 mm, and 3.5 x13 mm (MicroPort), and a polytetrafluoroethylene-covered coronary stent sized 3.5 x 18 mm (Lepu Medical Technology Co., Ltd.) Postoperative CTA demonstrated that the aneurysm was completely thrombosed with no leakage (Figure I). The post-procedural course was uneventful, and the patient was discharged after 4 days. At the 6-month follow-up, the patient remained asymptomatic.
Coronary artery PSAs are rare and usually occur after percutaneous procedures, trauma, dissection, infection, Behçet’s disease, pregnancy, or coronary artery fistula (CAF).1 The natural course of PSAs is largely unknown. The clinical presentation also depends on the size and mass effect of the PSA on surrounding structures. The symptoms include angina and shortness of breath. One-fourth of PSAs have an associated CAF, which can lead to congestive heart failure. The PSA may also be catastrophic because of the high risk of rupture resulting in tamponade, hemodynamic collapse and death.2 A delay in diagnosis or treatment may lead to the potential risk of complications, including ruptured pseudoaneurysm, thromboembolism, compression of adjacent structures, and a poor prognosis.3 There is no standard treatment guideline for rare entities. A conservative observational approach with pharmacological therapy may be used for asymptomatic patients with no evidence of angina or myocardial ischemia.4 Symptomatic patients with PSAs undergo treatment that includes percutaneous coronary intervention, coil embolization, or resection with bypass grafting.5 Our case highlights the crucial role of multimodality imaging, including TTE, CTA, and CAG, in the diagnosis of rare entities, which provides guidance for effective clinical treatment strategies.
Affiliations and Disclosures
Leizhi Ku, MD1; Jianjian Wang, MD2; Xiaojing Ma, PhD3
From the 1Department of Radiology, Wuhan Asia Heart Hospital Affiliated to Wuhan University of Science and Technology, Wuhan, P.R. China; 2Department of Thoracic Surgery, Hubei Cancer Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology, Wuhan, P.R. China; 3Department of Echocardiography, Wuhan Asia Heart Hospital Affiliated to Wuhan University of Science and Technology, Wuhan, P.R. China.
Dr Ku and Dr Wang contributed equally to the article.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Funding: This work is funded by the Wuhan Clinical Medical Research Center for Cardiovascular Imaging (CMRC202307).
Consent statement: The authors confirm that the patient provided informed consent for the procedures presented in this manuscript.
Address for correspondence: Xiaojing Ma, PhD, Department of Echocardiography, Wuhan Asia Heart Hospital Affiliated to Wuhan University of Science and Technology, No.753 Jinghan Road, Hankou District, Wuhan 430022, P.R. China. Email: klz1534292102@163.com; X: @klz13657254286
References
1. Ito Y, Kainuma S, Yoshikawa Y, et al. Unusual case of giant nonthrombosed right coronary artery pseudoaneurysm with coronary artery fistula. JACC Case Rep. 2021;3(5):806-810. doi:10.1016/j.jaccas.2021.01.015
2. Dalal P, Varma D, Chakravorty R, Sethi S, Bailey S, Prasad A. Transcatheter embolization of a giant coronary artery pseudoaneurysm. Cardiovasc Revasc Med. 2018;19(2):204-208. doi:10.1016/j.carrev.2017.10.010
3. Ghannam A, Amoroso N, Mathbout M, et al. Native coronary artery pseudoaneurysm after coronary artery bypass grafting. Heart Surg Forum. 2022 ;25(2):E297-E299. doi:10.1532/hsf.4531
4. Chen D, Chang R, Ho AT, Frivold G, Foster G. Spontaneous resolution of coronary artery pseudoaneurysm consequent to percutaneous intervention with paclitaxel-eluting stent. Tex Heart Inst J. 2008;35(2):189-91; discussion 192.
5. Kar S, Webel RR. Diagnosis and treatment of spontaneous coronary artery pseudoaneurysm: rare anomaly with potentially significant clinical implications. Catheter Cardiovasc Interv. 2017;90(4):589-597. doi:10.1002/ccd.26997