Double Culprit Lesion: A Challenging Case of Simultaneous Coronary Thrombotic Occlusion
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
We report a rare case of simultaneous ST-segment elevation in the infero-lateral and anterior leads with acute double coronary thrombotic occlusion successfully treated with double primary percutaneous coronary intervention (PCI) in a patient with hereditary thrombophilia.
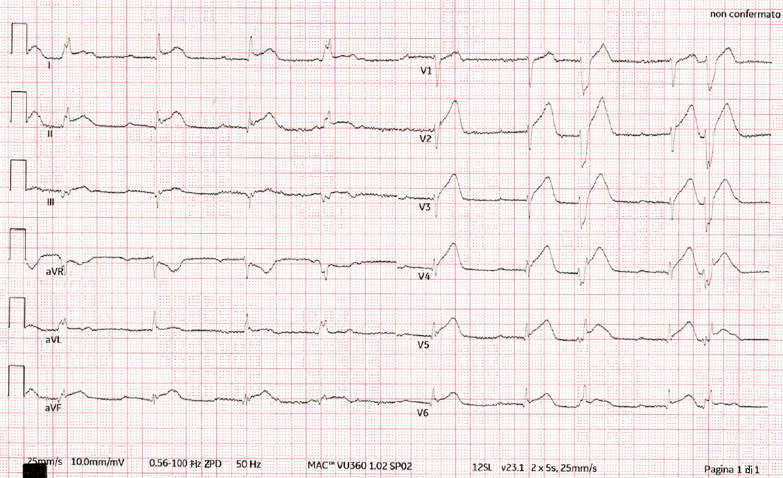
A 54-year-old man alerted the emergency system after experiencing oppressive chest pain radiating to his jugular and left upper limb, followed by syncope. Electrocardiogram (ECG) showed ST-segment elevation in the inferior and antero-lateral leads with complete atrioventricular (AV) block (Figure 1). After intravenous (IV) preloading of 300 mg of acetylsalicylic acid and 5000 IU of unfractioned heparin (UFH), the patient was transferred to the cardiac intensive care unit for primary percutaneous PCI.
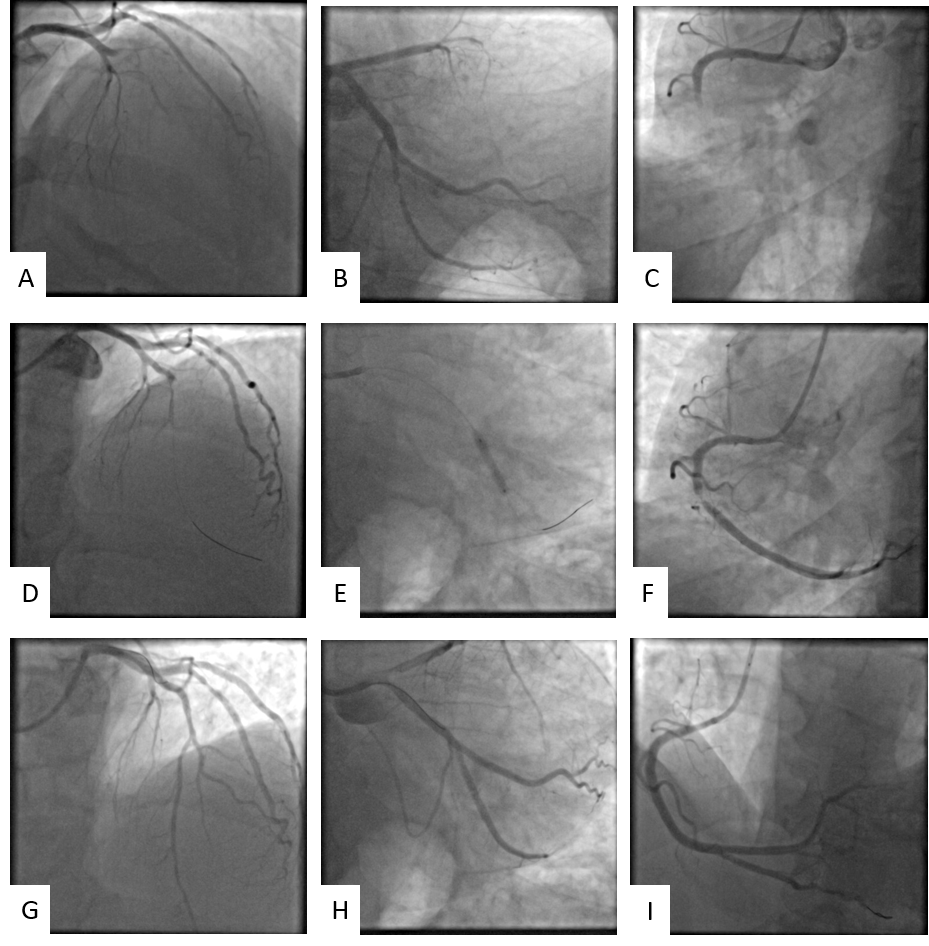
Echocardiogram showed apex, inferior wall, and inferolateral wall akinesia with moderately depressed left ventricular systolic function (ejection fraction [EF] 40%). Coronary angiography was performed via the right transradial approach and showed acute thrombotic occlusion of the mid-left anterior descending artery (LAD) (Figure 2A) and mid-right coronary artery (RCA) (Figure 2C) with Thrombolysis in Myocardial Infarction (TIMI)-flow 0 in both vessels and critical stenosis of the second obtuse marginal (OM) branch (Figure 2B).
After checking the basal activated coagulation time, UFH supplement was administered and an IV cangrelor infusion was initiated according to the patient’s weight. In consideration of the complete AV block, the RCA was treated first with angioplasty and implantation of one 3.5 x 18-mm Resolute Onyx drug-eluting stent (DES) (Medtronic) (Figure 2I). Subsequently, 2 episodes of ventricular fibrillation occurred and were treated with direct current shock at 200 J with immediate restoration of the sinus rhythm. Angioplasty and implantation of one 3.5 x 18-mm Resolute Onyx DES were performed in the mid-LAD (Figure 2D-G).
In both cases, after advancing the coronary guidewire, severe stenosis was evident after reopening the vessel. TIMI-flow 3 was reestablished in both the LAD and RCA after stent implantation.
Post-procedure, the patient was hemodynamically stable and asymptomatic. Staged angioplasty was performed with implantation of a DES on the second OM branch (Figure 2E-H). The patient was discharged with good hemodynamic compensation; ECG showed sinus rhythm and signs of previous necrosis in the inferior and anterior leads, and the echocardiogram confirmed left ventricular dysfunction (EF 40%). Dual antiplatelet therapy with acetylsalicylic acid (100 mg/die) and ticagrelor (90 mg bis in die) was initiated. In addition, pharmacological therapy for heart failure was set up and the patient was started on a follow-up and rehabilitation path. Forty days post-discharge, the patient was asymptomatic and clinically and hemodynamically stable. His left ventricular function was 45%, and ongoing therapy was confirmed.
ST-elevation myocardial infarction (STEMI) is a common presentation of acute coronary syndrome (ACS); approximately 38% of patients with ACS have a diagnosis of STEMI. Usually, STEMI is caused by thrombotic occlusion linked to atheromatous plaque rupture or erosion in 1 epicardial coronary artery.1 In a small percentage of cases, STEMI can be caused by 2 or more simultaneous epicardial coronary artery thrombotic occlusions (“multiple culprit lesions”); this rare condition is challenging and strictly time-dependent with poor clinical outcomes, including mortality. This condition is probably underestimated because autopsy studies reveal “multiple culprit lesions” with an estimated prevalence of 2.5%.2 In cases of chronic total occlusion (CTO), the occlusion of the infarct-related artery can cause acute ischemia in the collaterally supplied CTO area.3 As in this case, a systematic review found that the simultaneous thrombosis of the LAD and RCA was the most common angiographic finding.4 The clinical presentation is characterized by high-degree AV block, cardiogenic shock, or sudden cardiac arrest.
The optimal treatment of “multiple culprit lesions” is unclear because of the absence of these patients in randomized trials and guidelines.5 Imaging was not performed in this case because of the hemodynamical instability of the patient, and angiography guided the choice of the double revascularization strategy. The treatment was immediately successful with swift pain remission.
In this case, the pathophysiological mechanism was supposed to be the destabilization/rupture of a plaque with consequent massive release of inflammation agents and thrombosis. Additionally, the role of hereditary thrombophilia is uncertain because of the presence of atheromatous disease in other coronaries branches, but it could be a contributing factor for simultaneous thrombosis.
Acute double-vessel coronary thrombosis, an event with a high mortality rate, requires prompt diagnosis and management to prevent complications such as cardiogenic shock and ventricular arrhythmias. Early and efficient treatment is crucial to improve the survival rate of patients with these kinds of lesions. In our experience, a good interpretation of the angiography, along with ECG and echocardiographic findings, may be the fastest and best way to choose the revascularization strategy in a hemodynamically unstable patient.
Affiliations and Disclosures
Giovanni Lorenzoni, MD; Cristiana Denurra, MD; Pierluigi Merella, MD; Giuseppe Talanas, MD; Gavino Casu, MD, FESC
From the S.C. Cardiologia Clinica e Interventistica, Azienda Ospedaliero Universitaria di Sassari, Ospedale Civile SS Annunziata, Sassari, Italy.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication thereof, including any and all images.
Address for correspondence: Giovanni Lorenzoni, MD, S.C. Cardiologia Clinica e Interventistica, A.O.U. Sassari, Ospedale Civile SS Annunziata, Sassari, Italy. Email: giovalore84@gmail.com
References
- Hage G, Reibel I, Dib JC, et al. Double culprit lesions in a patient with ST-Segment Elevation myocardial infarction: should i stent or should i go? JACC Case Rep. 2021;3(18):1906-1910. doi:10.1016/j.jaccas.2021.07.028
- Ginanjar E, Yulianto Y, Salim S, Setyawan W. Double culprits in a patient with ST elevation myocardial infarction: a challenging but rewarding case. Acta Med Indones. 2018;50(2):165-167.
- Scholz M, Meyer T, Maier LS, Scholz KH. Infarct-related artery as a donor of collaterals in ST-segment-elevation myocardial infarction with concomitant chronic total occlusion: challenge of the double-jeopardy thesis. J Am Heart Assoc. 2023;12(7):e028115. doi:10.1161/JAHA.122.028115
- Saito R, Koyama K, Kongoji K, Soejima K. Acute myocardial infarction with simultaneous total occlusion of the left anterior descending artery and right coronary artery successfully treated with percutaneous coronary intervention. BMC Cardiovasc Disord. 2022;22(1):206. doi:10.1186/s12872-022-02652-3
- Jariwala P, Kulkarni GP, Misra KC, Jaishetwar G. “Double myocardial infarct syndrome” resulting from simultaneous occlusion of dual coronary arteries: a double jeopardy. Indian Journal of Clinical Cardiology. 2023;4(2):110-114. doi:10.1177/26324636231174725




















