Coronary Artery Aneurysm: Treat It Easily With a Stent?
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
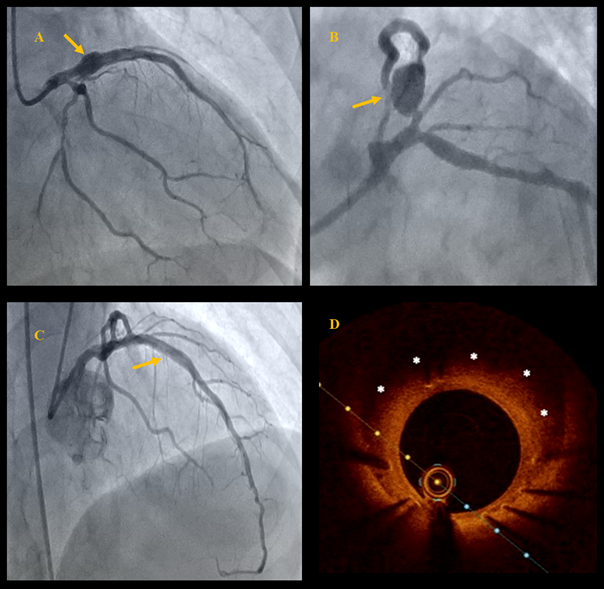
A 63-year-old man who was a smoker with no prior treatment for chronic diseases was admitted to the cardiology department with chest pain for the past 2 days due to non-ST-elevation acute myocardial infarction. Transthoracic echocardiography showed a left ventricular ejection fraction (LVEF) of 30% and akinesia of the inferior wall, interventricular septum, and apex. Coronary angiography revealed multivessel coronary artery disease without significant lesions in the right coronary artery (RCA) and with a prominent coronary artery aneurysm (CAA) in the proximal segment of the left anterior descending artery (LAD), as well as concomitant significant stenosis in LAD segments 6 and 7 and the marginal artery (Figure A and B, Video 1).
The heart team decided to perform percutaneous coronary intervention (PCI). The first stage involved PCI of the left main artery (LM) and LAD via the right radial approach with implantation of 2 zotarolimus-eluting stents (3.5 x 30 mm and 3.5 x 34 mm), and PCI of the circumflex artery (Cx) with a drug-coated balloon. The procedure led to improvement of flow through the LAD and residual filling of the aneurysmatic sac (Video 2). Further in-hospital stay was uneventful. The patient received dual antiplatelet therapy and statins and was scheduled for cardiac rehabilitation and follow-up angiography in 3 months. At the 3-month follow-up, echocardiography showed LVEF improvement to 45%. Follow-up coronary angiography confirmed a good PCI result (Figure C, Videos 3 and 4), and optical coherence tomography revealed full stent strut coverage, moderate neointimal hyperplasia, and complete sealing of the aneurysm cavity with endothelialized stent struts (Figure D).
CAA is defined as a vessel dilation exceeding 1.5 times the normal diameter and represents an asymptomatic vascular condition with an incidence of 0.3% to 5.3%.1 CAAs are more common in men and often affect the RCA, followed by the Cx, LAD, and LM. Aneurysms differ from ectasias by their localized nature and morphology, which can be saccular or fusiform.1 Causes include atherosclerosis, inflammation, genetic disorders, and iatrogenic factors.1 Complications include rupture, fistulas, mediastinal compression, or thrombus formation leading to stenosis, occlusion, or embolization. Treatment guidelines for CAAs are unclear, with options including surgery, percutaneous interventions, and pharmacological therapy.2,3 The approach depends on aneurysm size, location, structure, and symptoms. Surgery is preferred for large aneurysms (> 20 mm), high-risk perforation cases, or concurrent valvular defects. Percutaneous angioplasty with drug-eluting stents is effective for acute coronary syndrome or unstable angina. Stent grafts provide good short-term outcomes but carry long-term restenosis risks.2,3 Stable cases, small aneurysms (< 10 mm), or Kawasaki disease may benefit from less invasive methods. This case highlights stent implantation as a valid and safe treatment for CAA.
Affiliations and Disclosures
Wojciech Żakiewicz, MD1,2; Mariusz Łebek, MD1,2; Maciej T. Wybraniec, MD, PhD2,3,4; Grzegorz Smolka, MD, PhD1,2
From the 1Department of Cardiology, School of Health Sciences, Medical University of Silesia, Katowice, Poland; 2Upper-Silesian Medical Center, Katowice, Poland; 3First Department of Cardiology, School of Medicine in Katowice, Medical University of Silesia, Katowice, Poland; 4Member of the European Reference Network on Heart diseases - ERN GUARD-HEART
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the study and interventions described in the manuscript and for the publication of their data.
Address for correspondence: Wojciech Żakiewicz, MD, Department of Cardiology, School of Health Sciences, Medical University of Silesia, 47 Ziołowa St., 40-635 Katowice, Poland. Email: wzakiewicz@hotmail.com
References
- Kawsara A, Núñez Gil IJ, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC Cardiovasc Interv. 2018;11(13):1211-1223. doi:10.1016/j.jcin.2018.02.041
- Will M, Kwok CS, Nagaraja V, et al. Outcomes of patients who undergo elective covered stent treatment for coronary artery aneurysms. Cardiovasc Revasc Med. 2022;36:91-96. doi:10.1016/j.carrev.2021.05.018
- Takano M, Yamamoto M, Inami S, et al. Delayed endothelialization after polytetrafluoroethylene-covered stent implantation for coronary aneurysm. Circ J. 2009;73(1):190-193. doi:10.1253/circj.cj-07-0924




















