Collateral Clarity: Balloon Occlusion of an Epicardial Right Coronary Artery Branch to Map Left Anterior Descending Artery Perfusion
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
J INVASIVE CARDIOL 2025. doi:10.25270/jic/25.00243. Epub August 28, 2025.
We present a technically informative case of a 65-year-old man referred for coronary angiography (CAG) because of new onset presented angina during exercise. His past medical history included a percutaneous coronary intervention (PCI) to the mid-left anterior descending artery (LAD) due to acute myocardial infarction 3 years prior.
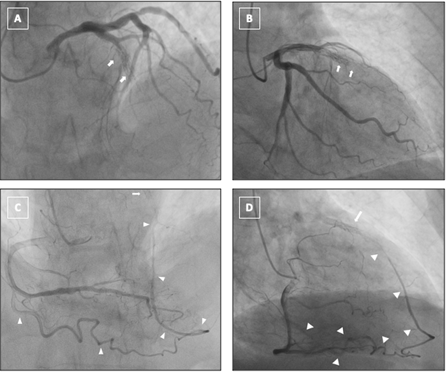
Diagnostic CAG revealed a chronic total occlusion (CTO) within the previously stented segment of the mid-LAD (Figure A and B; Videos 1 and 2). The lesion was heavily calcified, longer than 20 mm, and exhibited a tapered proximal cap. Importantly, no antegrade opacification of the distal LAD was observed. A single epicardial collateral channel originating from the acute marginal (AM) branch of the right coronary artery (RCA) was seen supplying the LAD territory (Figure C and D; Videos 3 and 4). No septal or secondary collateral pathways were visualized.
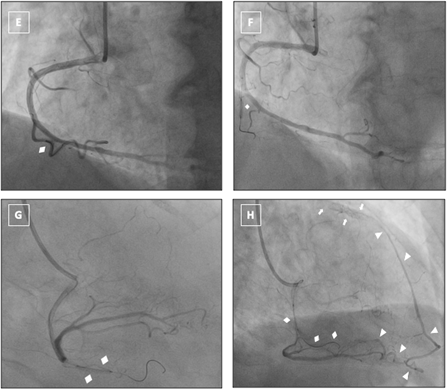
To functionally assess the completeness of collateral perfusion and uncover potential secondary channels, a selective balloon occlusion test was performed. A 2.0 × 15-mm semi-compliant balloon was advanced into the AM branch over a 0.014-inch guidewire (Figure E) and inflated to occlusive pressure to transiently obstruct the dominant epicardial collateral supplying the LAD (Figure F and G). Repeat RCA injections during balloon inflation failed to reveal any supplementary collateral filling of the LAD, thereby confirming the RCA-AM as the sole conduit of retrograde flow (Videos 5 and 6). Following balloon deflation, collateral flow promptly resumed, and the patient remained hemodynamically stable (Figure H, Video 7).
This targeted, temporary interruption of collateral supply provided real-time physiologic assessment of the coronary collateral network and yielded critical insight into LAD perfusion, directly shaping the staged procedural plan. Despite subsequent PCI attempts with antegrade and retrograde strategies, crossing was not achieved. This case illustrates the practical use of selective balloon occlusion of an epicardial collateral during CTO planning to confirm collateral dependence and guide strategy.
Affiliations and Disclosures
Dimitris Karelas, MD, MSc; Konstantinos Filippou, MD, MSc; Panagiotis Varelas, MD, MSc; Konstantinos Manousopoulos, MD, PhD; Ioannis Papadopoulos, MD; Ioannis Tsiafoutis, MD, PhD
From the 2nd Cardiology Department, Hellenic Red Cross Hospital Korgialenio-Benakio, Athens, Greece.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient for the intervention described in the manuscript and for the publication thereof, including any and all images.
Address for correspondence: Dimitris Karelas, MD, MSc, Cardiology Department, Hellenic Red Cross Hospital Korgialenio-Benakio, Athanasaki 2, Athens 11526, Greece. Email: dim.f.karelas@gmail.com; X: @d_karelas




















