Utilization of the Catheter Push Technique for Optical Coherence Tomography in Severely Stenotic Lesions
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
Abstract
The authors present 2 case examples of the C-PUSH (catheter push) optical coherence tomography (OCT) technique. The C-PUSH technique allows baseline assessment of virgin (unmodified) plaque in severely stenosed vessels where blood clearance is suboptimal and when OCT acquisition is performed in the standard fashion.
Introduction
Intravascular imaging is increasingly used to guide percutaneous coronary intervention (PCI) and provides valuable information on plaque morphology, lesion preparation, and stent optimization. Optical coherence tomography (OCT) can provide a higher resolution image than intravascular ultrasound but requires blood clearance for image acquisition.1 In severely stenotic lesions, the distally positioned OCT catheter often occludes contrast flow, causing inadequate blood clearance and suboptimal imaging. One technique to provide limited information in this scenario is flushing contrast with the side port to clear blood prior to pullback. Although this gives information on distal vessel sizing, the OCT image is often disrupted by artifacts while also failing to provide information on plaque morphology.
In 2013, Yamaguchi et al described a technique to overcome this problem by first positioning the OCT catheter proximal to the lesion.2 After contrast injection and adequate distal filling, the OCT catheter is rapidly transversed distally, and image acquisition follows. This technique was subsequently termed C-PUSH (catheter push) by Kobayashi et al, who also described an alternative technique using dextran instead of contrast.3 However, the C-PUSH technique is not often utilized, as operators usually predilate with small balloons to improve flow and the subsequent OCT image quality in these severely stenotic lesions. Here, the authors present 2 case examples where the C-PUSH OCT technique proved useful without predilatation.
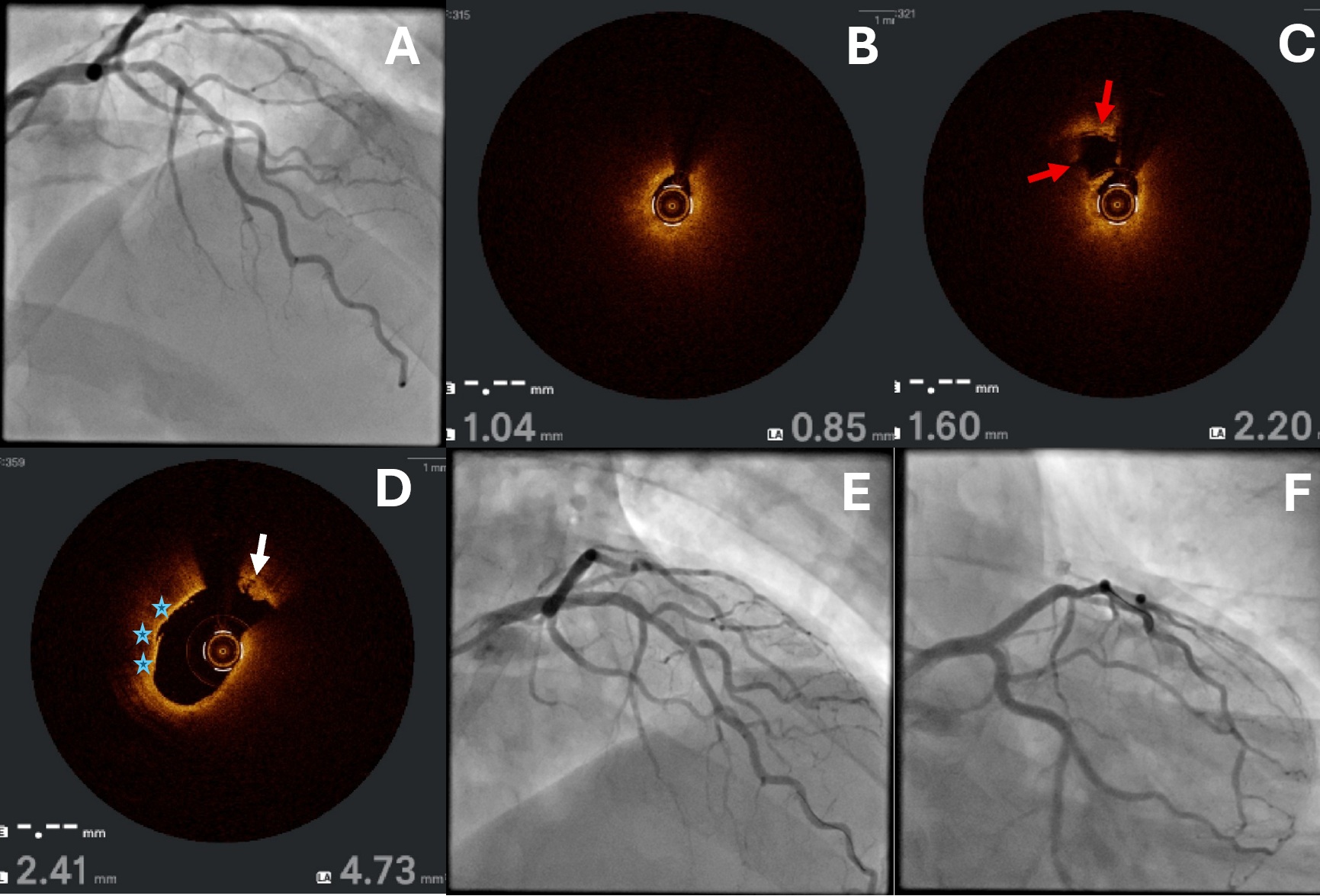
CASE 1
A 56-year-old man presenting with non-ST elevation myocardial infarction was found to have a severe stenosis in the proximal left anterior descending artery (LAD) on baseline angiography (Figure 1A; Video 1). OCT-guided PCI was planned, but flow was occlusive with the imaging catheter positioned distal to the lesion. The C-PUSH technique was performed without predilatation, demonstrating a heavy burden of lipidic plaque with a minimal lumen area (MLA) of 0.85 mm2, thin cap fibroatheroma, and plaque rupture (Figure 1B-D; Videos 2 and 3). Because of the plaque morphology, the lesion was directly stented with a 3.5 x 23-mm XIENCE Skypoint (Abbott) and post-dilated with a 4.0-mm noncompliant balloon. Final angiographic and OCT images are shown in Figure 1E and 1F and Video 4, respectively.
In this case, the C-PUSH OCT technique without predilatation allowed the identification of lipid-rich plaque and direct stenting to minimize the risk of slow/no reflow.
CASE 2
A 70-year-old man underwent an invasive angiography for crescendo angina and abnormal coronary computed tomography angiography. Baseline images showed a severe mid-LAD stenosis at the bifurcation of a moderate-sized diagonal artery, which was also diseased at the ostium with a retroflex take-off (Figure 2A; Video 5). The flow was occlusive with the OCT catheter placed distally, so the C-PUSH technique was utilized for baseline imaging acquisition (Videos 6 and 7). This showed a mix of lipidic and fibrocalcific plaque with an MLA of 1.85 mm2 and with heavy plaque burden at the bifurcation/carina (Figure 2B and 2C). The diagonal artery was wired using the reverse-wire technique with a Sion Black wire (Asahi) supported by a dual lumen microcatheter (Figure 2D). The LAD was then predilated, and a 2.75 x 28-mm XIENCE Sierra drug-eluting stent was deployed with a jailed balloon technique using an inflated 1.5 x 12-mm semi-compliant balloon in the diagonal artery (Figure 2E). Final angiographic and OCT images post-dilatation are shown in Figure 2F and Video 8, respectively.
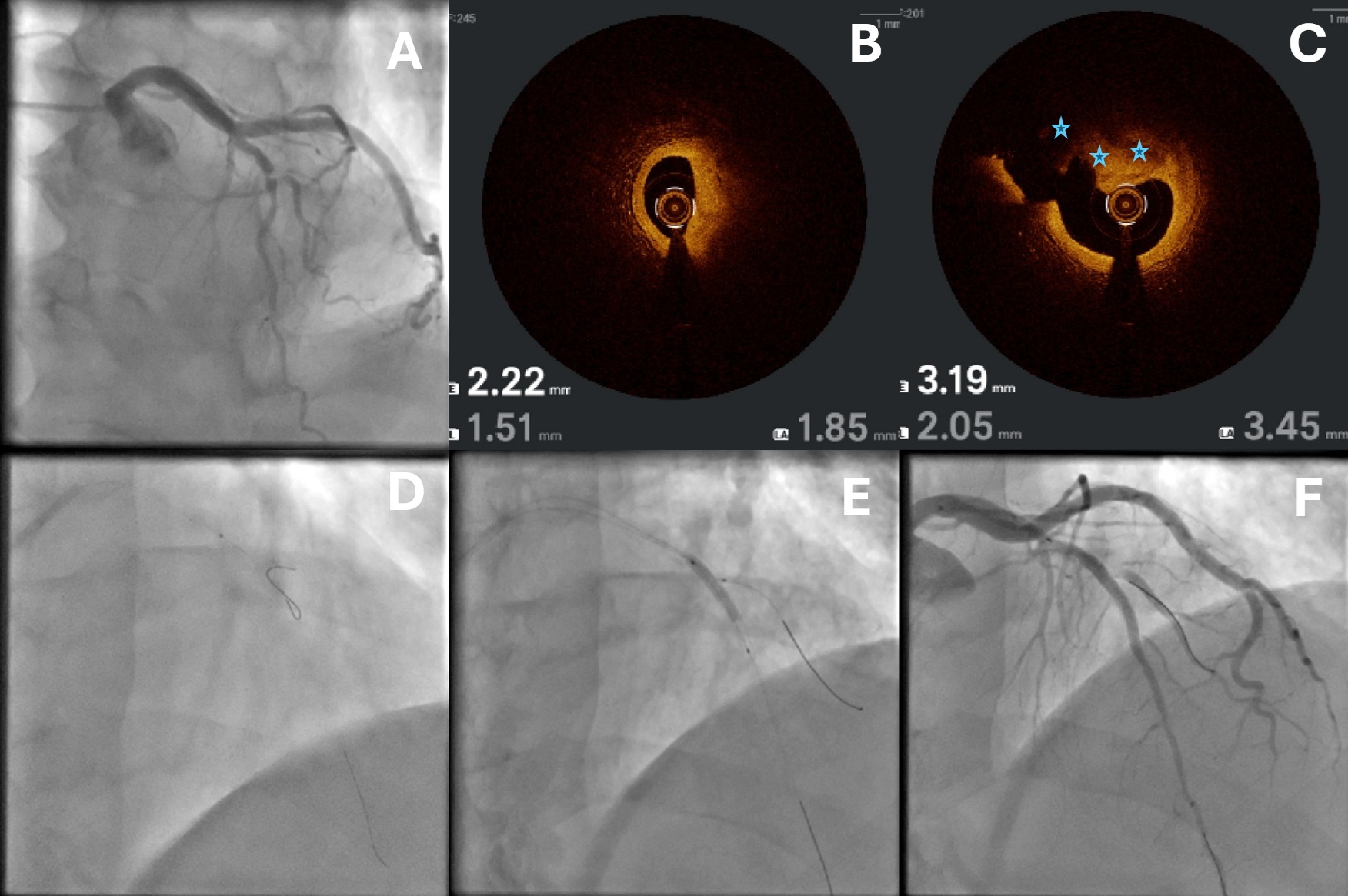
In this case, there would have been a high risk for side branch occlusion if we predilated the LAD for OCT acquisition. The C-PUSH OCT technique allowed us to assess the LAD disease before difficult wiring of the diagonal artery prior to subsequent predilatation/stenting.
Conclusions
In our experience, the C-PUSH OCT technique is useful in severely stenotic lesions where predilatation may increase procedural risk. The technique requires synchronization of 3 team members: the second operator/scrub nurse to inject contrast, the primary operator to rapidly transverse the lesion with the OCT catheter after adequate distal contrast flushing, and the technician to manually acquire the OCT images. Because of the need for rapid advancement of the OCT catheter after contrast injection, operators should take caution in tortuous or calcified anatomy, as resistance may increase risk of damaging the OCT catheter.
Affiliations and Disclosures
Bernard Wong, MBChB1; Cuneyt Ada, MBBS, PhD2; Bharat Khialani, MBBS3; George Touma, MBBS4; Sarah Fairley, MBBCh, BAO (Hons), PhD5; Eugene B. Wu, MD6
From the 1Cardiovascular Unit, North Shore Hospital, Auckland, New Zealand; 2Macquerie University Hospital, Sydney, New South Wales, Australia; 3Tan Tock Seng Hospital, National Healthcare Group, Novena, Singapore; 4Hurstville Private Hospital, Sydney, New South Wales, Australia; 5Wellington Cardiology Department, Wellington Hospital, Wellington, New Zealand; 6Prince of Wales Hospital, Chinese University of Hong Kong, Hong Kong SAR, China.
Disclosures: The authors report no financial relationships or conflicts of interest regarding the content herein.
Consent statement: The authors confirm that informed consent was obtained from the patient(s) for the study and/or intervention(s) described in the manuscript and for the publication of their data/thereof, including any and all images.
Address for correspondence: Bernard Wong, North Shore Hospital, 124 Shakespeare Road, Takapuna, Auckland 0620, New Zealand. Email: bernardwong@hotmail.co.nz; X: @Bernard_TW_Wong
References
1. Almajid F, Kang DY, Ahn JM, Park SJ, Park DW. Optical coherence tomography to guide percutaneous coronary intervention. EuroIntervention. 2024;20(19):e1202-e1216. doi:10.4244/EIJ-D-23-00912
2. Yamaguchi Y, Kagawa E, Kato M, et al. A novel procedure for imaging acute coronary syndrome lesions using frequency-domain optical coherence tomography. EuroIntervention. 2013;9(8):996-1000. doi:10.4244/EIJV9I8A166
3. Kobayashi N, Shibata Y, Okazaki H et al. A novel technique of low molecular weight dextran infusion followed by catheter push (D-PUSH) for optical coherence tomography. EuroIntervention. 2021;17(2):e149-e151. doi:10.4244/EIJ-D-20-00996




















