Use of Microcatheters for Side-Branch Protection During Rotational Atherectomy
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of the Journal of Invasive Cardiology or HMP Global, their employees, and affiliates.
Abstract
Objectives. Side branch protection during rotational atherectomy is an issue when treating bifurcations, particularly those in the left main artery. The authors investigated the effectiveness of side-branch protection with a microcatheter.
Methods. On a simulator, the authors evaluated the behavior of different microcatheters left in place into the side branch during rotational atherectomy.
Results. All microcatheters were variously damaged.
Conclusions. The authors discourage the practice of side-branch protection with a microcatheter, due to distal embolization of non-biological materials.
Introduction
Rotational atherectomy (RA) can be highly effective in treating heavily calcified coronary lesions but can be challenging to perform in the setting of bifurcations. Compromise of a relevant side branch (SB) during atherectomy can lead to hemodynamic compromise1 and periprocedural myocardial infarction.2 If atherectomy is performed across a bifurcation, the SB wire is typically removed, as it can fracture and embolize. Various techniques have been described to protect the SB, such as the use of a microcatheter (MC) over the SB wire. Atherectomy could still damage the MC, but this has received limited study and, thus, was the focus of our study.
Methods
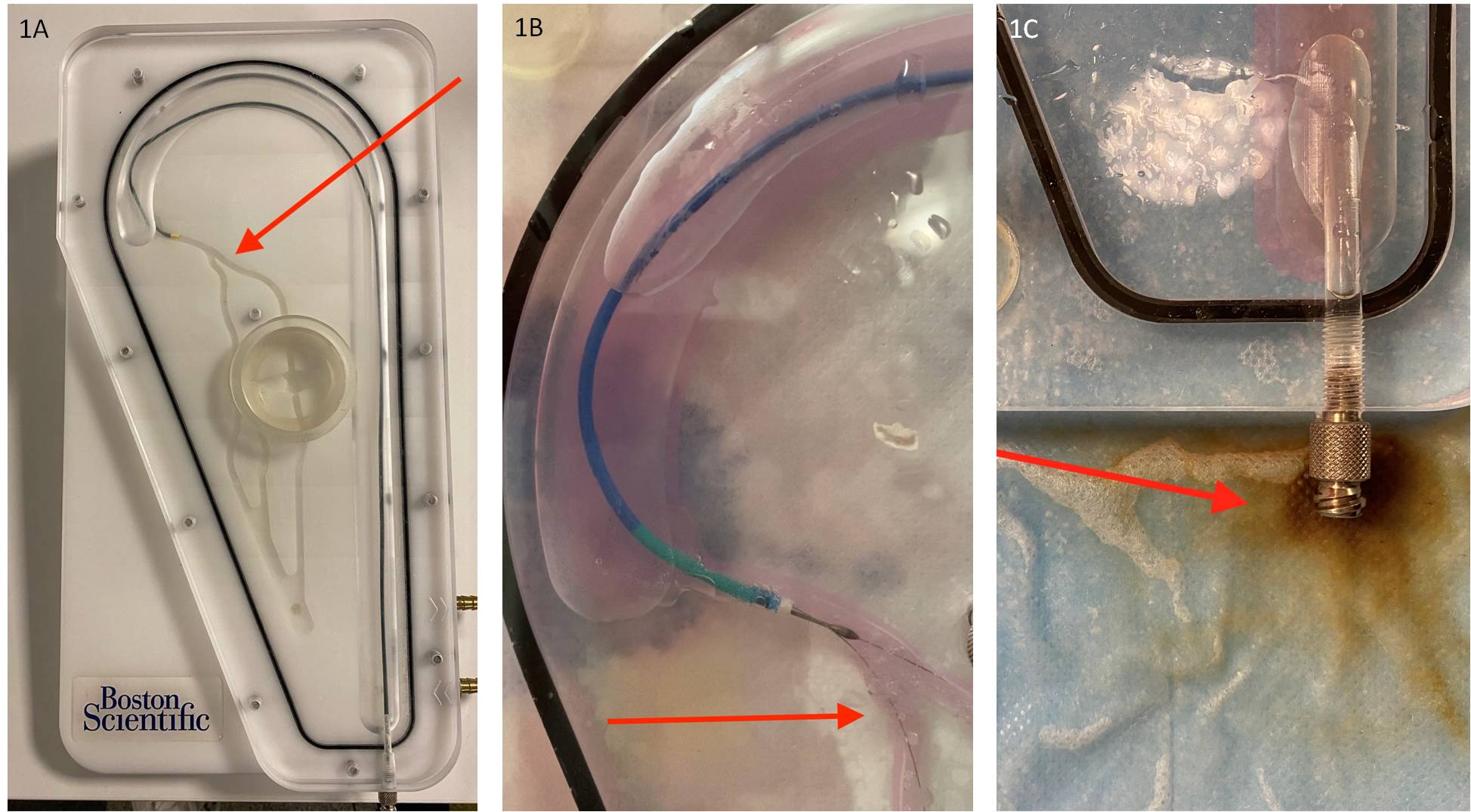
Using the Rotablator simulator (Boston Scientific) (Figure 1A), we positioned the RotaWire (Boston Scientific) on the main branch and an MC over a workhorse wire located in the SB (Figure 1B). We performed two 30-second cycles of RA with a 1.5 mm burr on the following MCs:
- Finecross (Terumo)
- Telemark (Medtronic)
- Turnpike LP (Teleflex Medical)
- Caravel (Asahi Intecc)
- Mamba (Boston Scientific)
- Corsair Pro (Asahi Intecc)
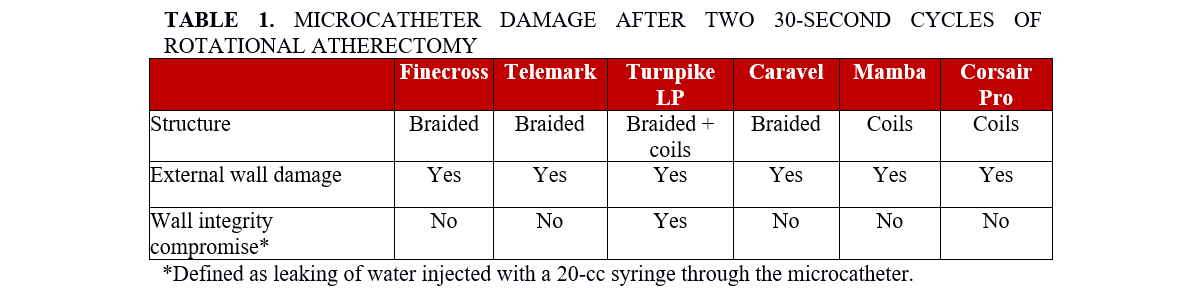
We tested both braided and coiled MCs (Table 1). The MC was kept in the same position during the 2 cycles. We evaluated the damage on the surface of the MCs visually and by camera zoom. We also tested the integrity of the MC wall by injecting saline to determine whether it was perforated.
The study conformed to the Declaration of Helsinki.
Results
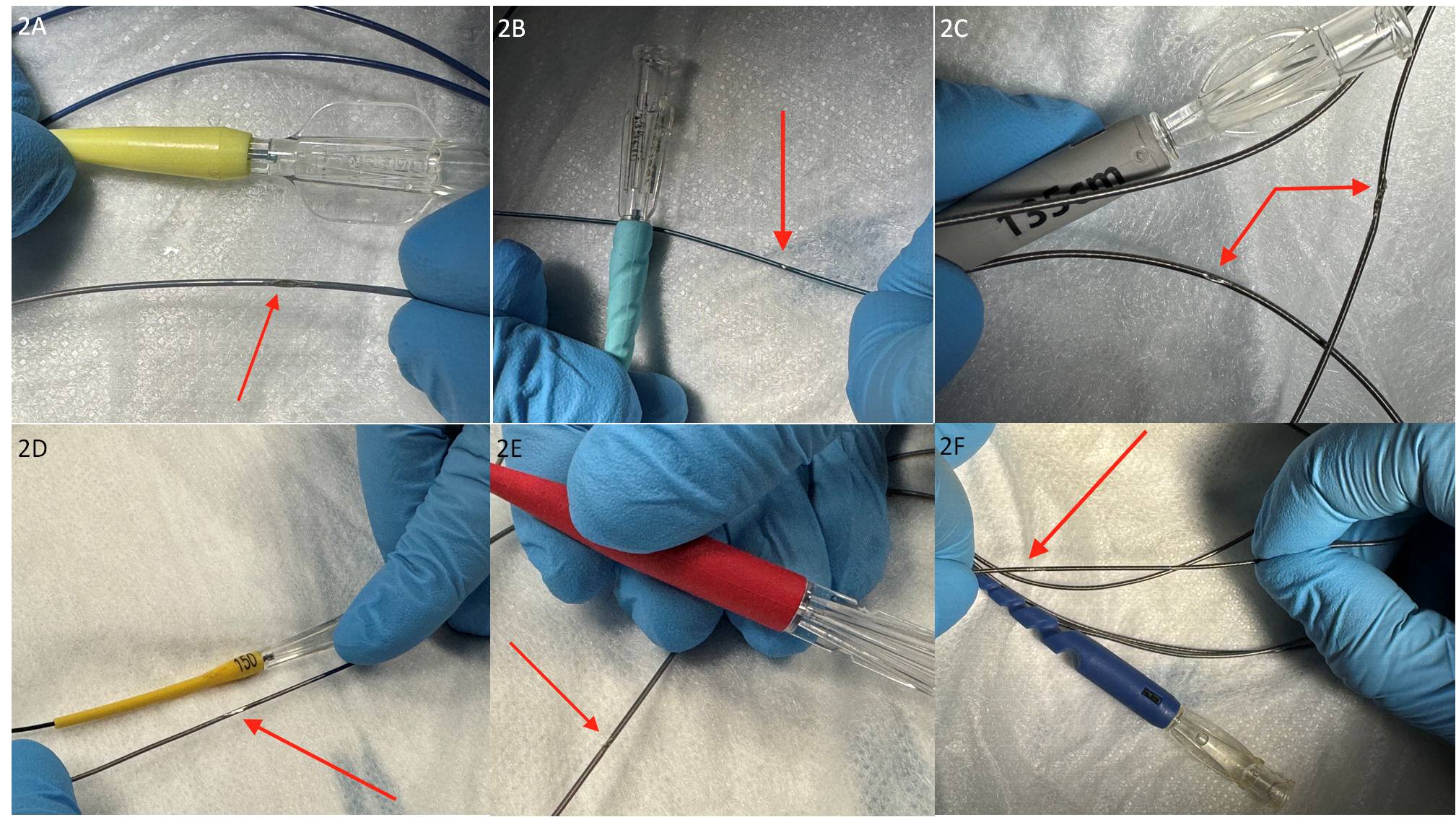
All 6 tested MCs were severely damaged by RA and none of them was completely intact after the 2 cycles of RA (Table 1, Figure 2). Moreover, the saline within the simulator contained debris in all cases (Figure 1C).
Discussion
Our study demonstrates that MC protection of an SB wire during RA results in significant MC damage and liberates debris.
The incidence of SB loss during RA of the main vessel was 3.6% to 10%.3 Protecting the SB may not always be needed: in 2 studies that used balloon-based techniques, calcium debulking with RA reduced SB occlusion (31.9% vs 7.4%, P = .001; 10.5% vs 3.6%, P = .017).4,5 SB occlusion depends on several parameters, such as vessel size, stenosis diameter, and baseline Thrombolysis in Myocardial Infarction flow.
In 1992, Leya et al tested in vitro SB protection during directional atherectomy (DA) using a “modified kissing atherectomy” technique and reported that nitinol wires were more resilient to mechanical trauma and had more axial strength than comparable stainless steel guide wires.6 In 1994, Lewis et al presented a case series of 30 patients treated with DA and SB protection with the aforementioned technique and reported 37% acute side branch closure, which was easily reopened as a result of the protection wire.7
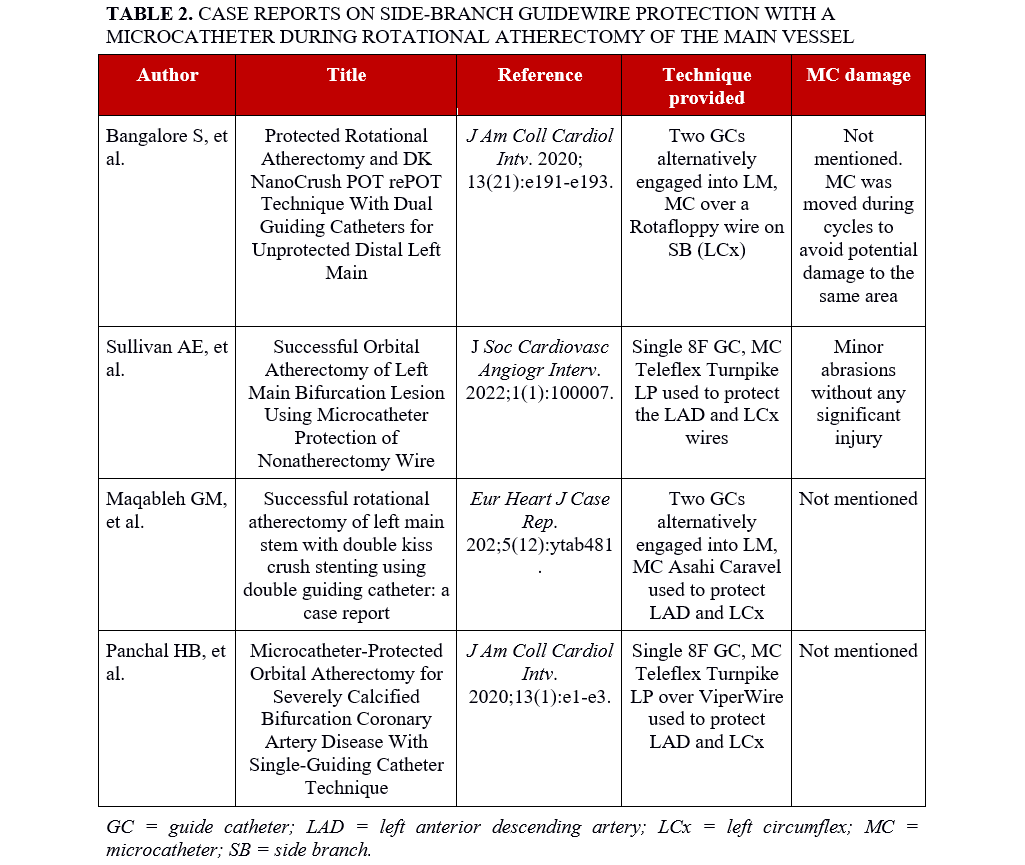
DA has been replaced by RA and orbital atherectomy, but SB occlusion remains a potential problem even with modern debulking techniques. In 2019, Medda reported use of an MC-protected SB wire in a patient undergoing left main percutaneous coronary intervention using 2 guide catheters (“ping-pong” technique)8 but did not mention whether any damage occurred to the MC. In 2022, Yang et al published an in vitro and in vivo (2 patients) study that evaluated the Finecross microcatheter (Terumo) protecting an SB guidewire during RA through two 7-Fr guide catheters. The protective MCs were damaged to varying degrees, but none was completely fractured; hence, they recommended limiting use of this technique to highly selected patients.9 Other case reports available on the subject are listed in Table 2.
Our study shows that any type of microcatheter can be damaged by RA; therefore, they should not be used to protect the SB wire. Moreover, distal embolization is likely to occur, potentially leading to no-reflow and myocardial injury.10
A guide extension has also been used to protect the SB guidewire during atherectomy of the main vessel (Guideliner sleeve technique),11 but this technique may also result in guide extension damage and distal embolization.
Limitations
Our study is limited by its in vitro design, although in-vivo MC use is likely to provide similar results. Moreover, we did not try different angulations and different main vessel and side branch sizes.
Conclusions
Rotablator use should increase as complexity of coronary artery disease increases and more evidence on good clinical practice is needed. MC protection of the SB wire during RA of the main vessel should be avoided due to risk of MC damage and distal embolization. We do not have data about the clinical relevance of distal embolization of microcatheter fragments, however, considering the non-biological material, we can assume it could impair flow in addition to calcium debris. Further in vivo studies are needed to evaluate the clinical importance of our findings.
Affiliations and Disclosures
Veronica Lio, MD1; Emmanouil S. Brilakis, MD, PhD2; Federico Beqaraj, MD1; Stefano Drago, MD1; Massimo Giammaria, MD1; Andrea Gagnor, MD1
From the 1Cardiology Department, Maria Vittoria Hospital, Turin, Italy; 2Minneapolis Heart Institute and Minneapolis Heart Institute Foundation, Abbott Northwestern Hospital, Minneapolis, Minnesota.
Disclosures: Dr Brilakis receives consulting/speaker honoraria from Abbott Vascular, the American Heart Association (associate editor, Circulation), Biotronik, Boston Scientific, Cardiovascular Innovations Foundation (Board of Directors), CSI, Elsevier, GE Healthcare, IMDS, Medtronic, and Teleflex; research support from Boston Scientific and GE Healthcare; is the owner of Hippocrates LLC; and is a shareholder in MHI Ventures, Cleerly Health, and Stallion Medical. The remaining authors report no financial relationships or conflicts of interest regarding the content herein.
Address for correspondence: Veronica Lio, MD, Maria Vittoria Hospital, Via Luigi Cibrario, 72, Turin 10144, Italy. Email: veronicalio@hotmail.it; X: @veronica_lio
References
1. Todoran TM, Yourshaw JP, Powell SP, Evans MC. Effectiveness of debulking strategies in coronary and endovascular interventions: targets and tools. In: Topaz O, ed. Debulking in Cardiovascular Interventions and Revascularization Strategies. Academic Press; 2022:133-179. doi:10.1016/b978-0-12-821451-0.00018-5
2. Zeitouni M, Silvain J, Guedeney P, et al; ACTION Study Group. Periprocedural myocardial infarction and injury in elective coronary stenting. Eur Heart J. 2018;39(13):1100-1109. doi:10.1093/eurheartj/ehx799
3. Walton AS, Pomerantsev EV, Oesterle SN, et al. Outcome of narrowing related side branches after high-speed rotational atherectomy. Am J Cardiol. 1996;77(5):370-373. doi:10.1016/s0002-9149(97)89366-6
4. Allali A, Abdel-Wahab M, Traboulsi H, et al. Impact of lesion preparation technique on side branch compromise in calcified coronary bifurcations: a subgroup analysis of the PREPARE-CALC trial. J Interv Cardiol. 2020;2020:9740938. doi:10.1155/2020/9740938
5. Mizuno Y, Sakakura K, Jinnouchi H, et al. Impact of rotational atherectomy on the incidence of side branch compromise in calcified bifurcation lesions undergoing elective percutaneous coronary intervention. J Cardiol. 2022;80(6):518-524. doi:10.1016/j.jjcc.2022.07.004
6. Leya FS, Lewis BE, Sumida CW, et al. Modified "kissing" atherectomy procedure with dependable protection of side branches by two-wire technique. Cathet Cardiovasc Diagn. 1992;27(2):155-161. doi:10.1002/ccd.1810270216.
7. Lewis BE, Leya FS, Johnson SA, et al. Acute procedural results in the treatment of 30 coronary artery bifurcation lesions with a double-wire atherectomy technique for side-branch protection. Am Heart J. 1994;127(6):1600-1607. doi:10.1016/0002-8703(94)90392-1
8. Medda M, Casilli F, Bande M, et al. Protected Rotational Atherectomy With Double-Guiding Catheter Technique for Unprotected Distal Left Main. JACC Cardiovasc Interv. 2019;12(4):e27-e29. doi:10.1016/j.jcin.2018.10.058.
9. Yang S, Dong S, Zhou Y, et al. Safety assessment of microcatheter-protected rotational atherectomy with the double guiding catheter technique for severely calcified left main bifurcation. J Interv Cardiol. 2022;2022:1399510. doi:10.1155/2022/1399510
10. Ndrepepa G, Kastrati A. Coronary no-reflow after primary percutaneous coronary intervention-current knowledge on pathophysiology, diagnosis, clinical impact and therapy. J Clin Med. 2023;12(17):5592. doi:10.3390/jcm12175592
11. Hafiz AM, Smith C, Kakouros N. The GuideLiner-Sleeve Technique: A novel technique for high-risk PCI using two left main guides for orbital atherectomy of two-vessel calcified ostial coronary artery disease. J Invasive Cardiol. 2017;29(11):E159-E160.





















