From Fragmented to Integrated: A Roadmap to Equity for Psychosocial Support in Rural and Underserved Cancer Programs
Introduction
Although biomedical advances in cancer care continue to improve survival, psychosocial care remains fragmented, especially in underserved and rural populations. Depression, anxiety, and emotional distress are common among patients with cancer and are known to impair treatment adherence, recovery, and overall outcomes. The integration of mental health services into oncology is essential for delivering high-quality, patient-centered care. The need is particularly urgent in medically underserved communities, where limited access to psychosocial support exacerbates health disparities and negatively impacts quality of life.
Materials and Methods
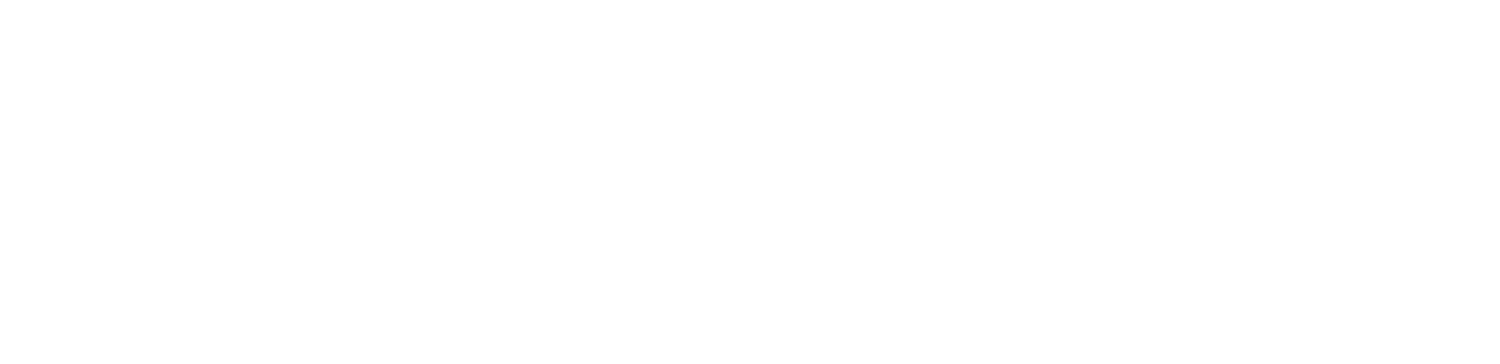
A mixed internal and external environmental scan was conducted to assess current barriers and opportunities for the integration of psychosocial services into cancer care programs, particularly those serving medically underserved populations. The internal assessment used the Commission on Cancer (CoC) standards to evaluate program structure, coordination roles, and policies for psychosocial services. External analysis applied a PESTEL (political, economic, social, technological, environmental, and legal) framework to evaluate broader systemic factors influencing access and implementation (Figure 1).
Strategic Challenges and Macro-Level Barriers to Psychosocial Oncology Care–A PESTEL Framework Analysis: The development and implementation of psychosocial oncology services in medically underserved, rural, and socioeconomically disadvantaged communities are shaped by multifaceted challenges, as illustrated through a PESTEL lens.
Results
The internal assessment identified gaps in role coordination and service delivery despite CoC recommendations for multidisciplinary engagement and distress screening. Financial toxicity remains a major barrier, with high out-of-pocket costs leading to delays or avoidance of care. For patients with low income, limited transportation and access to evidence-based therapies are associated with poorer outcomes.
Externally, inconsistent policies, economic limitations, stigma, and regulatory hurdles impede the integration of mental health care. Geographic and digital divides also limit access in rural and underserved communities. These findings underscore the need for a collaborative, multisector strategy to achieve sustainable integration of psychosocial care.
Recommendations
A four-part implementation framework is proposed to guide cancer programs in expanding psychosocial services:
- Sustainability. Secure financial viability through optimized payment models and retention strategies.
- Team-Based Workforce. Develop interprofessional teams with clear roles and ongoing capacity building.
- Implementation. Streamline integration of services into clinical workflows to maximize patient engagement.
- Dissemination. Improve communication strategies to raise awareness and usage of psychosocial resources.
These solutions are illustrated in a strategic implementation roadmap (Figure 2).
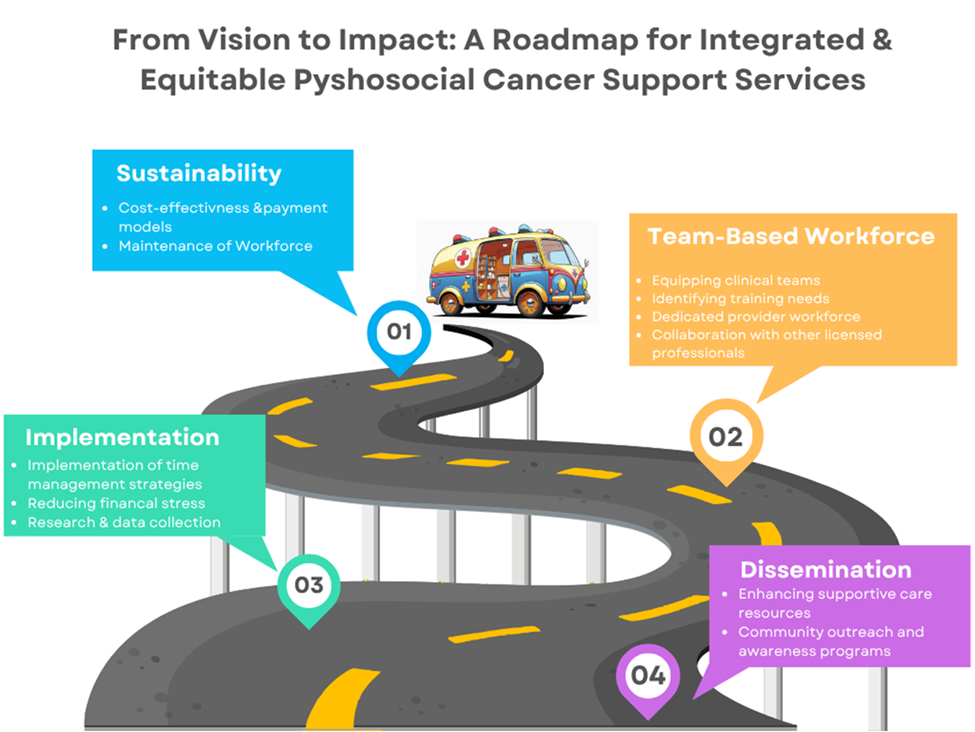
Addressing Psychosocial Care Disparities in Oncology–A Strategic Framework: Persistent gaps in access to psychosocial oncology care—driven by systemic barriers, workforce shortages, and adverse social determinants—require a targeted, system-level response. This framework highlights 4 strategic domains essential to advancing equity: sustainability, team-based workforce, implementation, and dissemination.
Conclusion
Psychosocial support is a critical, yet often overlooked, component of comprehensive cancer care. Addressing disparities in access, particularly in rural and underserved communities, requires structural changes, policy alignment, and multisector collaboration. By following a strategic, equity-driven implementation framework, cancer programs can improve holistic outcomes for vulnerable populations and deliver on the promise of truly patient-centered care.
Author Information
Authors:
Jerlinda Ross, MD, MS, MBA1; James Emery, PhD2
Affiliations:
1Methodist University Cape Fear Valley Health School of Medicine, Fayetteville, NC
2Duke University Fuqua School of Business, Durham, NC
References
- Alder NE, Page AEK, et al. Cancer care for the whole patient: meeting psychosocial health needs, Washington DC (DC) National Academies Press (US). Published online 2008. Accessed July 7, 2025. https://nap.nationalacademies.org/catalog/11993/cancer-care-for-the-whole-patient-meeting-psychosocial-health-needs
- Optimal resources for cancer care (2020 standards. American College of Surgeons. Updated January 1, 2023. Accessed July 7, 2025. https://www.facs.org/quality-programs/cancer-programs/commission-on-cancer/standards-and-resources/2020/
- Abbott DE, Voils CL, Fisher DA, Greenberg CC, Safdar N. Socioeconomic disparities, financial toxicity, and opportunities for enhanced system efficiencies for patients with cancer. J Surg Oncol. 2017;115(3):250-256. doi:10.1002/jso.24528
- Noyes K, Monson JRT, Rizvi I, Savastano A, Green JSA, Sevdalis N. Regional multiteam systems in cancer care delivery. J Oncol Pract. 2016;12(11):1059-1066. doi:10.1200/JOP.2016.013896
- Crabtree-Ide C, Sevdalis N, Bellohusen P, et al. Strategies for improving access to cancer services in rural communities: a pre-implementation study. Front Health Serv. 2022;2:818519. doi:10.3389/frhs.2022.818519