Autonomy in End-of-Life Cancer Care Measurement: A Bioethical Framework for Analyzing Quality Measures
The predominant US health care quality measure development and endorsement processes, as summarized in the Center for Medicare and Medicaid Services (CMS) Blueprint, have various well-accepted criteria for evaluating measures. This blog series examines the characteristics of a good quality measure through the framework of bioethical principles, with oncology measures serving as case studies. While bioethical principles are fundamental to all health care practices, they are not formally prioritized during quality measure development. This second blog in the series will apply the principle of autonomy to analyze the Percentage of Patients who Died from Cancer Receiving Systemic Cancer-Directed Therapy in the Last 14 Days of Life quality measure (where a lower score indicates better performance). The first blog in the series addressed the principles of beneficence and nonmaleficence, and a future third blog will consider the principle of justice.
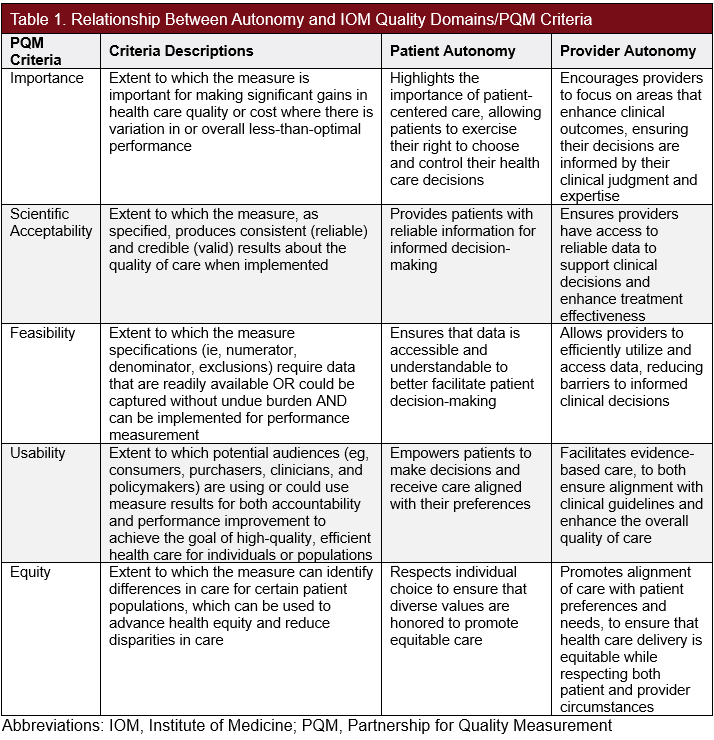
In Principles of Biomedical Ethics, bioethicists Beauchamp and Childress describe the principles of autonomy, beneficence, nonmaleficence, and justice to collectively form a framework for analyzing ethical issues in health care. Quality measures are often classified using the CMS Consensus-Based Entity (CBE) criteria. The current CBE, the Partnership for Quality Measurement (PQM), employs a set of specific criteria to evaluate these measures, including importance, scientific acceptability, feasibility, usability, and equity. These criteria often intersect with bioethical principles, as illustrated in Table 1. Although these criteria implicitly touch on components of the 4 key bioethical principles, an additional ethical perspective offers further insights into how quality measures serve public health, enhance the quality of care, and meet patient needs.
Autonomy
The principle of autonomy emphasizes the right of competent adults to make informed decisions about their lives and health, free from coercion or interference by external forces. To exercise autonomy, individuals must possess the capacity to make decisions, receive and understand critical, unbiased, and culturally sensitive information, and demonstrate the ability to reason and communicate their decisions clearly and comprehensibly. Based on these criteria, autonomy seldom extends to children younger than 18 years or to individuals incapacitated by physical or mental conditions. In clinical settings, autonomy is upheld through formal informed consent and by informal expression of preferences that provide patients with clear information about diagnoses, treatment options, risks, benefits, and potential outcomes. Minimizing bias in the delivery of this information to preserve decision-making independence is equally important.
While the principle of autonomy is often viewed from the patient's perspective, clinician autonomy is also vital, as it encompasses the right of health care professionals to make decisions that are in the best interest of their patients, free from coercion influenced by undue or irrelevant pressures from insurance companies, government regulations, peers, and patient or family demands. This autonomy enables shared decision-making, fostering a collaborative care environment where both patient values and clinician expertise are respected.
Quality measures can actively promote autonomy by ensuring that patients are informed, engaged, and empowered in their care. Tools such as patient satisfaction surveys, decision aids, and robust informed consent processes contribute to transparent care delivery. However, quality measures may, in certain situations, conflict with clinician professional judgment, frustrating clinicians who are being assessed on adherence to clinical standards.
Respecting autonomy in end-of-life care requires honoring the patient’s treatment preferences and ensuring that medical interventions align with their goals of comfort and quality of life. Chemotherapy utilization at the end of life is associated with worse quality of life near death among patients with otherwise good baseline performance status, increased emergency department visits, cardiopulmonary resuscitation, mechanical ventilation, dying in an intensive care unit (ICU), and higher estimated costs of care. Holding physicians accountable for reducing the number of patients receiving end-of-life systemic therapy benefits patient quality of life while also improving medical resource utilization.
Measure Analysis
The Percentage of Patients who Died from Cancer Receiving Systemic Cancer-Directed Therapy in the Last 14 Days of Life (lower score = better performance) measure aims to address the use of systemic cancer-directed therapy in end-of-life care. This CMS Merit-Based Incentive Payment System (MIPS) measure, stewarded by the American Society of Clinical Oncology (ASCO), evaluates the number of patients who received systemic cancer-directed therapy in the last 14 days of life. As an inverse measure, achieving a lower performance score indicates better quality of care (Table 2).
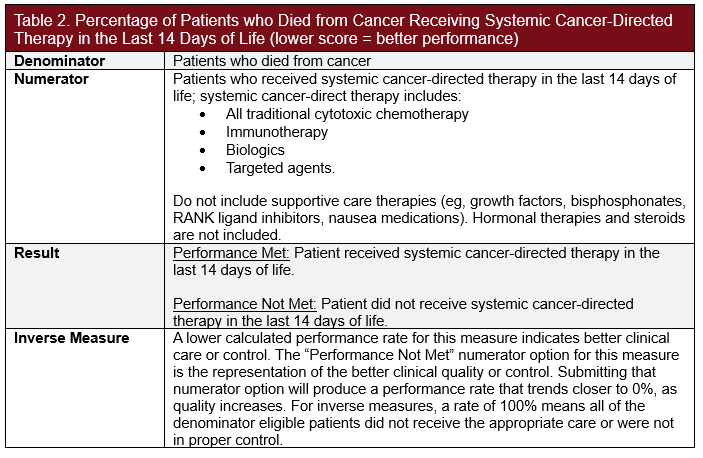
Key criteria needed to evaluate this quality measure through the lens of autonomy include components for fostering discussions to support informed shared decision-making between patients and clinicians. While minimizing the use of systemic cancer-directed therapy in end-of-life care is generally important, applying this standard uniformly across all patients neglects potential needs and desires for rejecting palliative care, which could be influenced by preferences, cultural beliefs, and situational understanding.
Provider autonomy plays a crucial role in supporting end-of-life treatment decisions. Clinical judgment and experience allow providers to offer recommendations to patients empathetically and pragmatically. In certain cases, such as when patients or families request to pursue all possible treatments, provider autonomy is vital in contextualizing treatment options and expected outcomes. Providers can use their autonomy and expertise to guide families in framing decisions around the patient's values and goals, ensuring choices align with a comprehensive understanding of both a good life and a good death, supported by clinically sound recommendations.
Opportunities for Enhancement
To identify opportunities for enhancement of the Percentage of Patients who Died from Cancer Receiving Systemic Cancer-Directed Therapy in the Last 14 Days of Life measure, it is useful to analyze how its components align with the subprinciples of autonomy, as well as to identify any existing gaps. For instance, incorporating reporting requirements for unbiased patient education and shared decision-making prior to discontinuing systemic cancer-directed therapy can better align this measure with the principle of autonomy.
Patient autonomy is compromised when patients do not fully comprehend their care plan and palliative care options. Without thorough discussions to inform and educate patients, there is a risk that systemic chemotherapy may be discontinued without their consent, or patients may not fully grasp the reasons for discontinuation. Incorporating cultural sensitivity in patient decision-making is crucial, as cultural beliefs significantly influence perceptions of acceptable treatments, illness, and end-of-life care preferences. This situation could lead to decision-making that lacks the full scope of informed consent, with patients relying on guidance from clinicians or other external forces to make critical end-of-life decisions (Table 3).
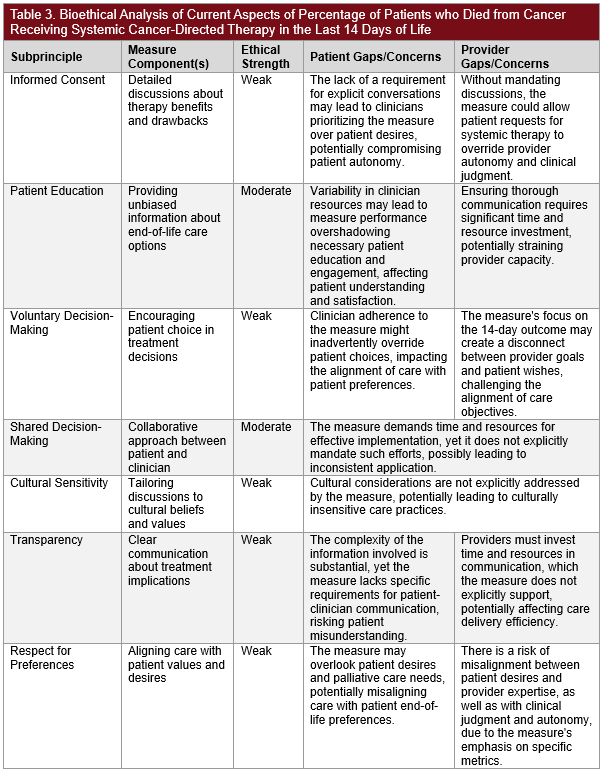
While maintaining clinician autonomy enables health care professionals to advocate for clinically sound decisions, it is crucial for clinicians to engage in open, bilateral conversations with patients. This process requires time and resources to ensure thorough communication, both of which can be limited for providers. Additionally, differing goals of care can create a disconnect between the wishes of patients and what their clinicians consider clinically appropriate, leading to potential tensions. Conflicts may arise when provider autonomy clashes with patient autonomy. In building shared decision-making with patients, clinicians must offer recommendations without being paternalistic. Clinicians must respect both their professional judgment and the autonomy of patients, ensuring collaborative treatment decisions with a full understanding of their implications for the patient's quality of life. Providers should use culturally sensitive assessment tools, such as adapted questionnaires and interpreters, to understand patients' diverse cultural backgrounds. This approach is also beneficial for opening the most effective and clear line of provider-patient communication, ensuring that the provider’s expertise, recommendations and thoughts are communicated adequately.
Conclusion
This analysis of the Percentage of Patients who Died from Cancer Receiving Systemic Cancer-Directed Therapy in the Last 14 Days of Life measure illustrates how the bioethical principle of autonomy can be applied to assess quality measures. Autonomy highlights the importance of patient-centered shared decision-making and adequate informed consent, as well as clinician professional judgment. By integrating an ethical framework into quality measurement analysis, measure developers and implementers can enhance the effectiveness of quality measures in addressing health outcomes and meeting patient needs.
 About Nandita Ammanamanchi, BA
About Nandita Ammanamanchi, BA
Nandita Ammanamanchi is a senior analyst on the Market Access team at Real Chemistry, where she applies her expertise in health care research, health equity, and data analytics to inform strategic decision-making across therapeutic areas. She is currently pursuing a Master of Science in Bioethics at Harvard Medical School, with a capstone focus on narrative ethics in high-intensity care settings. Nandita brings a multidisciplinary lens to complex challenges in health care policy and access, and is passionate about leveraging data and research to drive equitable health outcomes and shape the future of health care.
 About Rachel Delinger, MPH
About Rachel Delinger, MPH
Rachel Delinger is a senior manager on the Real Chemistry Market Access team. She is data-driven with expertise in outcomes research and real-world evidence generation, and works across functions to inform market access strategy, serve as a quantitative methodologist, and supports evidence generation efforts that align with evolving access landscapes. She brings a strong analytical foundation to market access strategy, bridging clinical, economic, and patient-centered perspectives.

About David Blaisdell, BA
David Blaisdell, a senior director at Real Chemistry, leads and manages client projects, providing insight and subject matter expertise, particularly on quality landscape analyses and measure gap identification. David has led and contributed to projects focused on oncology quality measurement to identify key gaps in measures used in accountability programs and opportunities for measure development. Through this experience, David helps clients navigate measurement and value-based payments and define strategies for success.
 About Tom Valuck, MD, JD
About Tom Valuck, MD, JD
Tom Valuck, MD, JD, is the editor of Quality Outlook. He formerly led the Market Access Value-Based Care discipline for the Market Access team at Real Chemistry. The team uses research and strategic advisory services to help our clients improve health and health care by assessing, responding to, and shaping the value landscape.
Tom is a thought leader on health care system transformation, focused on achieving better health and health care outcomes at a lower cost. Tom’s work includes facilitating the exploration of next-generation measurement and accountability models for health care delivery systems. He also helps clients develop strategies to achieve success within the value-based marketplace.













