Recalcitrant Total Occlusion of the Superficial Femoral Artery – Image-Guided Stent Placement
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Ivana Kumar, Research Associate1; Kusum Lata, MD, FACC, FSCAI2; Anshita Kumari, MBBS3
1Sutter Health, Tracy, California; Quarry Lane School, Dublin, California;
2Interventional Cardiology, Sutter Health, Tracy, California; Board of Trustees, SCAI;
3Kasturba Medical College, Manipal, India; Research Associate, Sutter Health, Tracy, California
Disclosures: The authors report no conflicts of interest regarding the content herein.
The authors can be contacted via Ivana Kumar at ivana.dkumar@gmail.com.
Click here for a PDF of this article, courtesy of Cath Lab Digest.
Over the past two decades, endovascular peripheral vascular intervention has undergone substantial development and is now a standard treatment for complex peripheral vascular disease. Innovations such as drug-coated balloons, intravascular lithotripsy, and atherectomy devices have helped to further the “leave no metal behind” approach. However, stent implantation is still necessary for some refractory lesions in order to guarantee long-term patency.
Herein, we report a case of recurrent superficial femoral artery occlusion that necessitated the use of endovascular intervention with image-guided stent placement.
Case Presentation/Procedure
A 91-year-old female with a past medical history of hypertension, hyperlipidemia, and chronic tobacco use initially underwent intervention for a 100% chronic occlusion of the left superficial femoral artery (SFA) in August 2021. Treatment included intravascular lithotripsy (IVL) and prolonged percutaneous transluminal angioplasty (PTA). She was managed medically post-procedure with a low-dose anti-Xa inhibitor, statins, and blood pressure control. Her claudication symptoms resolved initially.
Despite reducing her smoking, symptoms recurred, and 7 months later, a repeat peripheral angiogram revealed re-occlusion at the same site in the left SFA. She was successfully treated with laser atherectomy, PTA, and drug-coated balloon. Her symptoms again improved.
However, claudication worsened over time. A third peripheral angiogram performed 2 years later, showed 100% occlusion at the same location in the left SFA. The lesion was successfully recanalized using laser atherectomy, PTA, and drug-coated balloon. At least a two-vessel runoff below the knee was restored.
The patient remained asymptomatic until another 10 months passed, when recurrent symptoms prompted further evaluation. Angiography confirmed total occlusion of the left SFA at the same location. Revascularization with stent placement was planned due to repeated occlusions and failure of prior endovascular therapies.
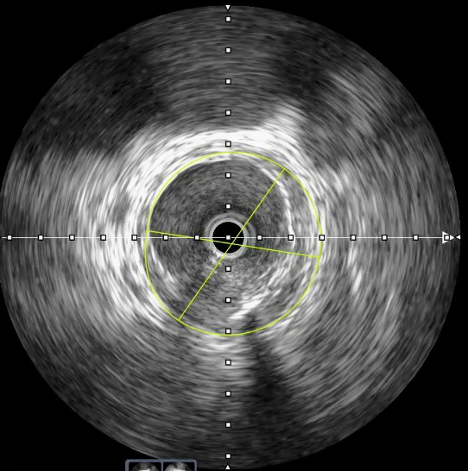
The occlusion was successfully crossed with a guidewire (Videos 1-3). Intravascular ultrasound (IVUS) was utilized to evaluate vessel morphology and size, and guide precise stent placement. IVUS from the distal to proximal SFA revealed a distal luminal area of approximately 6.0 mm² and significant calcific burden (Figure 1). Sequential PTA with 5.0 mm and 6.0 mm balloons was performed, followed by successful deployment of a 6.0 mm x 150 mm self-expanding stent. Post dilatation was done with a 6.0 mm balloon (Videos 4-5).
Video 1. Mid superficial femoral artery chronic total occlusion sections.
Video 2. Distal reconstitution of mid superficial femoral artery chronic total occlusion.
Video 3. Road map imaging of wiring of mid superficial femoral artery chronic total occlusion.
Video 4. Stent at mid superficial femoral artery.
Video 5. Distal stent segment of mid superficial femoral artery chronic total occlusion.
Moderate disease in the anterior tibial artery was addressed with prolonged PTA (Videos 5-6). The peroneal artery was patent, while the posterior tibial artery showed chronic 100% occlusion.
Video 6. Below-knee arteries outflow.
Video 7. Below-knee anterior tibial artery.
Discussion
Endovascular therapy has become a crucial option in the management of chronic total occlusions (CTOs) of peripheral arteries, particularly for patients who are high-risk surgical candidates.1 While the “no metal” approach — using atherectomy, prolonged PTA, and drug-coated balloon therapies — has been successful in many cases, a subset of lesions, especially in elderly patients with extensive calcification and recurrent disease, necessitates stent placement.
This patient, despite being 91 years old, remained functionally active but experienced significant limitations due to progressive peripheral vascular disease. All initial attempts adhered to standard endovascular therapeutic strategies aimed at avoiding stents, including:2
1. Intraluminal wire crossing;
2. Prolonged PTA;
3. Use of laser atherectomy and IVL;
4. Optimizing outflow with at least two-vessel runoff below the knee;
5. Comprehensive medical management with anticoagulants, antiplatelets, statins, and lifestyle modifications including smoking reduction.
Despite repeated endovascular interventions, recurrent occlusions of the SFA ensued, necessitating bailout stenting as a viable and minimally invasive salvage strategy, given the high perioperative morbidity risk associated with surgical bypass in a geriatric patient of advanced age (91 years).
Although atherectomy and PTA have been shown to reduce target lesion revascularization in many cases,3 bailout stenting still has a role when all other strategies fail, particularly in symptomatic patients.4
Conclusion
We successfully employed a standard endovascular therapy-first approach to manage a complex CTO of the left SFA in a very elderly patient. Although initial non-stenting interventions were unsuccessful in achieving durable patency, subsequent IVUS-guided stent placement yielded favorable immediate outcomes.5 The patient’s asymptomatic status and maintained activity level underscore the importance of tailoring treatment strategies to individual patient needs in complex peripheral vascular disease cases.
References
1. Aihara H, Soga Y, Mii S, et al; RECANALISE Registry Investigators. Comparison of long-term outcome after endovascular therapy versus bypass surgery in claudication patients with Trans-Atlantic Inter-Society Consensus-II C and D femoropopliteal disease. Circ J. 2014; 78(2): 457-64. doi:10.1253/circj.cj-13-1147
2. Sakamoto Y, Hirano K, Mori S, et al. Impact of extravascular ultrasound-guided wiring on achieving optimal vessel preparation and patency in endovascular therapy for superficial femoral artery chronic total occlusion. J Invasive Cardiol. 2022 Oct; 34(10): E730-E738. doi:10.25270/jic/22.00102
3. Suriyanto MGRI, Pranata R, Kamarullah W, et al. The efficacy and safety of atherectomy combined with drug-coated balloon angioplasty vs. drug-coated balloon angioplasty for the treatment of lower extremity artery disease: a systematic review and meta-analysis. Front Cardiovasc Med. 2024 Sep 27; 11: 1472064. doi:10.3389/fcvm.2024.1472064
4. Rammos C, Radecke T, Lortz J, Steinmetz M, Rassaf T. Guidelines adherence or chronic total occlusion recanalization of the superficial femoral artery with a stentless approach: The next frontier? SAGE Open Med Case Rep. 2019 Jan 11; 7: 2050313X18823445. doi:10.1177/2050313X18823445
5. Writing Committee Members; Gornik HL, Aronow HD, Goodney PP, et al. 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the management of lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2024 Jun 18; 83(24): 2497-2604. doi:10.1016/j.jacc.2024.02.013














