The Invisible Revealed: The Importance of IVUS in Diagnosing and Treating a Coronary Wire Complication
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Muhammad Imran Hanif, MBBS, FCPS (Cardiology), FSCAI, FRCP; Muhammad Sikandar Saleem, MBBS, FCPS (Cardiology); Muhammad Ansar Maqsood, MBBS, FCPS (Cardiology)
Al-Aleem Medical College, Lahore / Gulab Devi Hospital; Pakistan Kidney and Liver Institute and Research Center (PKLI & RC)
Lahore, Pakistan
Muhammad Imran Hanif, MBBS, can be contacted at dr.imranhashmi786@gmail.com.
Muhammad Sikandar Saleem, MBBS, can be contacted at msikandarsaleem@gmail.com.
Muhammad Ansar Maqsood, MBBS, can be contacted at dr_ansarmaqsood@hotmail.com.
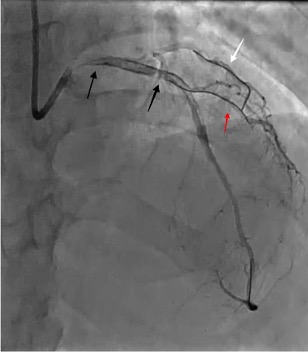
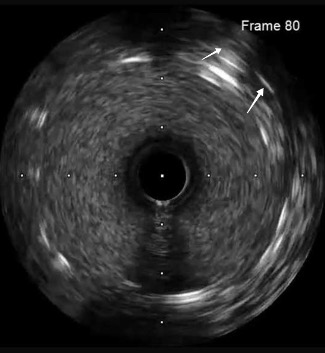
A 72-year-old male underwent elective percutaneous coronary intervention (PCI) for a significant stenotic lesion in the left anterior descending (LAD) artery (Figure 1 white arrow, Video 1).

Video 1
A wire was placed in the diagonal branch prophylactically to preserve side branch patency during main vessel stenting. After successful deployment of a drug-eluting stent (DES) in the LAD, the side branch wire was withdrawn. However, a radiopaque segment remained within the side branch, while the remaining wire fractured and became entrapped behind the stent struts (Figure 2 [black arrows], Video 2).
Video 2
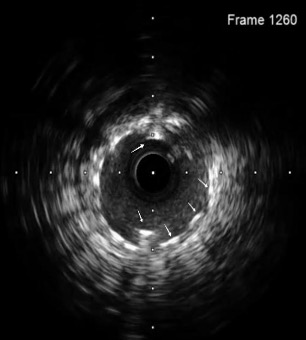
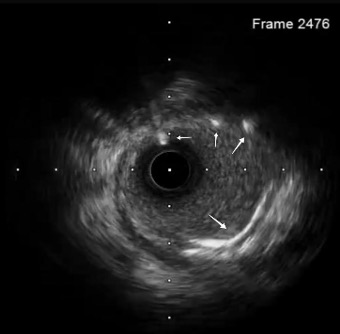
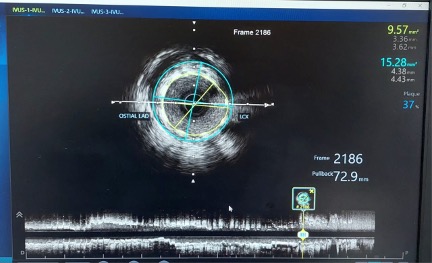
A coronary snare was used to retrieve the proximal segment of the retained wire. Partial extraction was achieved, but tangled wire fragments remained lodged in the proximal LAD. To stabilize these remnants, an additional DES was deployed to pin the wire against the vessel wall. Although angiography initially appeared satisfactory, intravascular ultrasound (OptiCross, Boston Scientific) proved pivotal by revealing that the wire loops had coiled within the stent, extended retrogradely into the proximal LAD, and reentered the stented segment near the left main stem (LMS) (Figures 2 [red arrow], 3A-C, Video 3).
Video 3
Due to persistent slow distal flow and increased thrombotic risk, a repeat snaring attempt was unsuccessful (Video 4).
Video 4
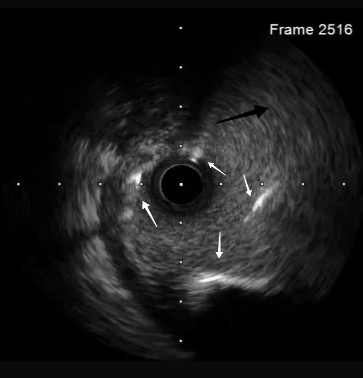
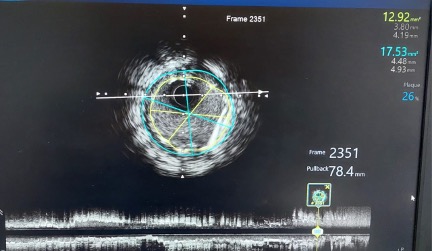
A second DES (Resolute Onyx, Medtronic) was then deployed from the proximal LAD into the LMS, effectively jailing the wire fragments. IVUS assessment was performed from the ostial LAD (Figure 4A-C, Video 5).
Video 5
Final angiography confirmed TIMI-3 flow with no dissection, perforation, or distal embolization; the wire in the side branch remained in place at the end of the procedure (Figures 2 [white arrow], 4A-C, 5, Video 6).

Video 6
Follow-up
The angioplasty was performed in October 2022. The patient remained hemodynamically stable and asymptomatic, with no complications on serial non-invasive evaluations. Periodic follow-up visits were conducted, with the most recent evaluation in early September 2025 showing preserved left ventricular function on echocardiography and good functional status without any cardiac symptoms.
Take-Home Messages
• IVUS guidance provides superior visualization of stent deployment and wire-related complications compared with angiography alone.
• Dual wiring techniques in bifurcation lesions require careful management to prevent entrapment or fracture of the side branch wire.
• Entrapped or fractured wires can be managed by retrieval, crushing with an additional stent, or jailing, depending on feasibility and safety.












