Spotlight: Jersey Shore University Medical Center
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Margaret McGowan, MSN, RN, CEN, CV-BC, Clinical Nurse Educator Specialist (CNES); Tresy Thomas, MSN, RN, FNP-BC, Lead APN for Invasive Cardiology
Neptune, New Jersey
The authors can be contacted via Margaret McGowan, MSN, RN, CEN, CV-BC, Clinical Nurse Educator Specialist (CNES), at margaret.mcgowan@hmhn.org.
Click here for a PDF of this article, courtesy of Cath Lab Digest.
Tell us about your hospital.

Jersey Shore University Medical Center (JSUMC), located in Neptune, New Jersey, offers advanced, compassionate care just minutes from the beach. Serving the communities of central New Jersey, our 691-bed academic medical center is a member of Hackensack Meridian Health and is nationally recognized for nursing excellence with Magnet designation since 1995. We provide numerous advanced specialty care services to a large population, including Level I adult and pediatric trauma services, comprehensive stroke care, cardiac rehabilitation, cancer treatment, structural heart services, cardiothoracic surgery, and much more. SUMC has been ranked by U.S. News & World Report as a Top 10 hospital in NJ for 13 consecutive years. Jersey Shore has received 10 consecutive ‘A’ grades for patient safety from The Leapfrog Group. The medical center is the only open and minimally invasive heart surgery center in New Jersey’s Monmouth and Ocean counties.
Tell us about your cath lab.
In December 2024, our department moved to a newly built Invasive Cardiology unit in the hospital. This facility is equipped with 11 specialized labs, including 4 for interventional cardiology, 4 for electrophysiology (featuring one bi-plane lab), 2 hybrid labs for structural heart procedures and device lead extractions, and a dedicated lab for transesophageal echocardiograms (TEEs) and cardioversions.
To ensure a seamless patient experience, the unit also includes 29 bays, 9 of which are radial lounge chairs, for prepping and recovering our patients in one spacious state-of-the-art unit. In response to our high patient volume, we expanded our care area to another unit in June 2025 with an additional 8-bay discharge area.
As a designated primary percutaneous coronary intervention (PCI) center with on-site cardiothoracic surgery, JSUMC is a leader in cardiac intervention. In 2024, our team performed 4,099 diagnostic cases and 1,781 PCIs, as reported by the National Cardiovascular Data Registry (NCDR).
We have earned accreditation from the American College of Cardiology (ACC) for our Cath Lab, Chest Pain Center, Electrophysiology Lab, and Transcatheter Valve Program. Furthermore, we have achieved the ACC HeartCARE Center of Excellence designation and the NCDR Platinum Performance Award.

What cases does your cath lab perform?
We provide extensive and comprehensive diagnostic and interventional care. More often than not, we incorporate intravascular ultrasound (IVUS), diastolic hyperemia-free ratio (DFR), and fractional flow reserve (FFR) with the AVVIGO+ System (Boston Scientific) and FFR, resting full cycle ratio (RFR), coronary flow reserve (CFR), and index of microvascular resistance (IMR) with the CoroFlow Cardiovascular System (Abbott). We also have CathWorks FFRangio (Medtronic) integrated in our four cath labs.
Our PCIs commonly involve rotational atherectomy with RotaPro (Boston Scientific), intravascular lithotripsy with Shockwave (Johnson & Johnson MedTech), thrombectomy, and laser atherectomy. We also utilize mechanical circulatory support devices, including Impella (Abiomed) and intra-aortic balloon pumps.
We perform peripheral, carotid, and renal angiograms and interventions, including renal denervation with Symplicity (Medtronic). In February 2023, we began performing pulmonary embolism and deep venous thrombosis thrombectomies using Inari/Stryker devices, and our caseload has since increased significantly. Additionally, we perform patent foramen ovale and atrial septal defect closure, balloon aortic valvuloplasty, pericardiocentesis, temporary transvenous pacemaker insertion, cardiac biopsy, and CardioMEMS (Abbott) implants in our laboratory.
Most recently, we welcomed endovascular neurosurgery into our department and have begun performing cerebral angiograms and interventions, including treatment for strokes. This initiative allows us to leverage our cath lab team’s procedural expertise and skill to serve an additional patient population.

Renee Tawil, RN, Nurse Manager; Nikki Shillabeer, RN, Assistant Nurse Manager; Tresy Thomas, APN, Lead APN; Margaret McGowan, RN, Clinical Nurse Educator Specialist; Betsy Bouchard, RN, Assistant Nurse Manager; & Meagan Scrimer, RN, Assistant Nurse Manager.
How many staff members do you have?
In our entire Invasive Cardiology department, we have 81 registered nurses (RNs), 26 radiologic technologists (RTs), 7 advanced practice nurses (APNs), 7 patient care technicians, 6 access service representatives/secretaries, and 2 service line coordinators. Of this group, 33 nurses and 19 RTs are dedicated to the cath lab. Our leadership team consists of a nurse manager, a supervisor, a clinical nurse educator specialist, and 5 assistant nurse managers.
Currently, 44 interventional cardiologists have privileges in our cath lab. These physicians cover a large area of central New Jersey among 10 different cardiology groups. Our department benefits from a highly engaged and visible cardiology leadership team composed of Dr. Renato Apolito (Director, Catheterization Lab), Dr. Riple Hansalia (Director, EP Lab), Dr. Matthew Saybolt (Director, Structural Heart), and Dr. Brett Sealove (Chair of Cardiology).
Under the leadership of Program Director Dr. Jesus Almendral and Associate Program Director Dr. Jeffrey Selan, our cardiac fellows play a significant role in our patient care. We are excited to expand our training opportunities with the launch of our Interventional Fellowship Program, led by Dr. Matthew Schoenfeld as Program Director.

What are the roles of the staff members in your cath lab?
Our highly skilled RNs are central to patient care in the cath lab. As circulators, they conduct comprehensive patient assessments, monitor hemodynamics, and administer medications, including moderate sedation. To have the skill, knowledge, and autonomy to perform these roles, we require all of our nurses to have at least 2 years of critical care nursing experience. Additionally, these nurses document procedural events and record hemodynamics. Our RNs also rotate through the prep and recovery areas to provide seamless continuity of care from admission to discharge. Advanced training for experienced cath lab RNs is offered in structural heart and neurological procedures.
Working closely together, our RTs are essential partners in the lab. They scrub in alongside interventional cardiologists and fellows, expertly managing the imaging equipment and providing procedural support. They are also trained to document events in our hemodynamic management system. Our Lead RT, Bob Kochel, oversees equipment and supplies and supports staff training and continuing education.

Do you have a cardiogenic shock protocol?
Using the American College of Cardiology (ACC), Society for Cardiovascular Angiography and Interventions (SCAI), and the National Cardiogenic Shock Initiative as guidance for best practice, our group collaborates with the cardiovascular intensive care leaders, fellows, and interventional cardiologists to develop protocols for this patient population. We have established nursing interventions that begin when cardiogenic shock is suspected and continue these interventions throughout the patient’s hospitalization.
Our team meets monthly to review cardiogenic shock cases, enhancing our clinical knowledge and refining our care protocols. We were part of the National Cardiogenic Shock Initiative and are currently in the Can Escalation Reduce Acute Myocardial Infarction Mortality in Cardiogenic Shock (CERAMICS) trial led by Henry Ford Health System.

Do you have a process to review complications?
Our cath lab has a very robust Quality Assurance (QA) process. A team that includes the Chair of Cardiology, the Director of the Cardiac Cath Lab, interventional cardiologists, nursing leadership, and advanced practice providers meets monthly to review complications.
According to SCAI best practice and ACC recommendations, we review cath lab deaths, in-lab cardiac arrests, emergency coronary artery bypass grafts (CABG), strokes, unanticipated PCI, vascular complications, contrast-induced nephropathy/in-hospital dialysis, anaphylaxis, respiratory depression requiring reversal/intubation, medication errors, verbal miscommunication, and cases with excessive radiation. These cases are then further tracked by the Outcomes Department and are filed for trending.
What are some changes you have made regarding patient safety?
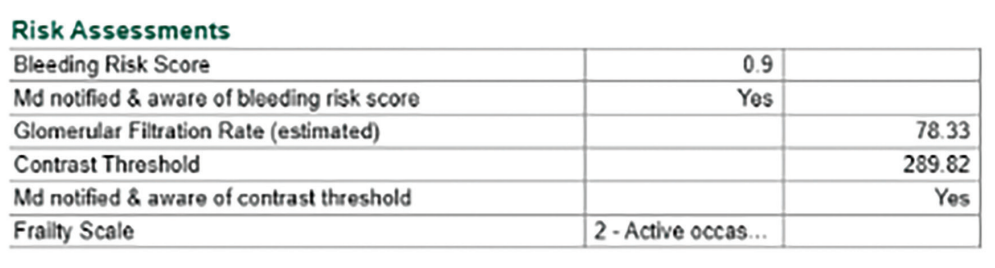
To mitigate the risk of contrast-induced nephropathy (CIN), we have implemented two key protocols. First, we utilize the ACC recommendation of calculating a patient-specific contrast threshold by multiplying the glomerular filtration rate (GFR) by 3.7. This value is then documented in the electronic medical record (EMR) (Figure 1) and on our nursing communication tool, and verbalized during the procedural timeout. During the procedure, the circulating nurse then monitors contrast administration, and verbalizes when the physician has used half of the contrast threshold amount and when the threshold is met. Cases that exceed the contrast threshold are recorded by the NCDR registry and then reviewed during our monthly QA meetings. We have also developed a proactive intravenous hydration protocol to protect high-risk CIN patients.
Other risk assessments we perform and document (Figure) include the Clinical Frailty Scale and a Bleeding Risk Assessment. The Clinical Frailty Scale is a method to assess the overall level of fitness or frailty of patients 65 years or older undergoing left heart catheterizations or PCIs. By assessing this, we can provide individualized medical care and even plan for transitions in care leaving the hospital. We also utilize the ACC CathPCI Bleeding Risk Calculator in order to better identify patients undergoing PCIs who are at higher risk of developing bleeding complications. By evaluating this risk and communicating it among the procedural and post-procedural team, we can implement early and continuous monitoring and interventions to minimize the risk of bleeding complications.
Additionally, every outpatient that is discharged from our unit receives a follow-up call from one of our nurses. We use this time to confirm they are taking their prescribed medications, answer their questions, and reinforce their care plan, bridging the gap between hospital and home.
Do you have a radiation safety protocol?
We have a multi-layered radiation safety protocol to ensure the lowest possible exposure to the patient and staff. Our GE imaging systems provide automated auditory alerts at five-minute fluoroscopy intervals and require staff to acknowledge the alarm. Furthermore, our protocol mandates verbal notification to the physician at key dose thresholds (3 Gy and each subsequent 1 Gy). Cases exceeding 5 Gy require a review in our monthly Quality Assurance meetings and are filed for trending. These patients also receive direct patient education that is documented in the EMR and receive a 14-day follow-up call from one of the APNs to review any skin changes.
To minimize patient radiation exposure, our default fluoro is set to 7.5 frames per second. Our physicians are also cognizant of positioning the equipment and utilize techniques such as bringing the image intensifier closer to the patient, avoiding steep angles, and varying the beam’s location.
Every team member is equipped with personal dosimeter badges, with their exposure levels monitored monthly by our physicists to ensure they remain well below the 5000 mRem annual limit. We also provide additional monitoring for expectant mothers, issuing a fetal monitoring badge to ensure the dose remains under the 500 mRem gestational limit. This monitoring is complemented by physical shielding, including annually inspected lead aprons and integrated lead shields built into our procedural tables.
What new projects has your cath lab been working on?
With the expansion of our department, one major focus was improving our patient care and satisfaction. By involving our procedurally trained cath lab nurses in the prep and recovery process, we ensure patient education is delivered by clinicians with direct, expert knowledge of the procedures. This promotes improved patient education and instills confidence in the care we provide.
To further enhance continuity, we introduced a dedicated overnight nursing staff within our unit, nearly eliminating the need for transfers to inpatient units and ensuring uninterrupted, expert care around the clock. We also provide patient education folders to all PCI patients that include information on dual antiplatelet therapy (DAPT), coronary artery disease, and other pertinent information. This is reinforced by post-discharge follow-up calls, conducted by our nurses the day after discharge. These calls are instrumental in identifying potential complications, addressing patient concerns, and ensuring a safe and supported transition back home.
We have expanded our clinical capabilities to include endovascular neurological angiograms and interventions, utilizing the advanced imaging of our bi-plane lab. With support from the OR and endovascular neurosurgeons, we have trained select experienced RNs and RTs to manage this patient population.
What makes your cath lab stand out?
Our team makes our cath lab stand apart from others. Every individual plays a vital role, not just in a procedure, but in a patient’s life. That commitment is reflected in our outstanding patient outcomes.
We must commend our seasoned staff for their extraordinary efforts throughout our recent expansion. They have consistently delivered compassionate, expert care to our patients while simultaneously teaching our new team members. Their clinical skill and knowledge are invaluable assets that have been essential during this period of rapid growth.
Recognition is also due to our newest team members. Joining a department in the midst of a major expansion is not easy, and yet they have met the challenge with determination and enthusiasm. We encourage their continued education and are dedicated to helping them build long, successful careers in the cath lab. Careers that will one day rival the incredible 30-year cath lab experience of our very own Victor, RT, and Cheryl, RN.
We appreciate you for taking the time to learn about our cath lab, and we thank Cath Lab Digest for fostering a community of collaboration and education.
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center











