Advancing Interventional Cardiology at Baystate Medical Center With Next-Generation Imaging and Technology
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Amir Lotfi, MD, FSCAI1; Andrew Goldsweig, MD, MS, FSCAI2
1Chief of Cardiology; 2Director of Heart and Vascular Clinical Research Baystate Medical Center, Springfield, Massachusetts
Click here for a PDF of this article. Logging in or registration may be required (it's free!).
Baystate Medical Center in Springfield, Massachusetts, is the only academic and tertiary care medical center in western New England, serving nearly one million people across a wide regional catchment. Under the leadership of Amir Lotfi, MD, Chief of Cardiology, the program has expanded steadily in both procedural volume and scope. That growth has been supported by deliberate investment in people and infrastructure, including the recruitment of Andrew Goldsweig, MD, MS, in 2023 as Director of Heart and Vascular Clinical Research. Dr. Goldsweig helped bring online Baystate’s new suite of four state-of-the-art Philips Azurion FlexArm labs. To improve workflow, support accuracy, and manage safety for patients and staff, Drs. Lotfi, Goldsweig, and colleagues are incorporating Philips solutions such as Dynamic Coronary Roadmap, co-registered physiology and imaging with IntraSight, and echo-fluoro fusion imaging with EchoNavigator, into routine practice.

Dr. Lotfi, can you start by telling us about Baystate Medical Center and your goals for it as a center of excellence?
Baystate Medical Center is a 780-bed, independent academic medical center and a teaching site for UMass Chan Medical School – Baystate. It is the only comprehensive cardiac center in western Massachusetts, serving patients across western Massachusetts, northern Connecticut, southern Vermont, and New Hampshire. We also oversee three additional regional hospitals and accept referrals from seven more, so our reach is substantial. We perform more than 6,000 cath lab procedures annually, including over 1,300 coronary interventions. Our percutaneous coronary intervention (PCI) program is among the largest in the state and consistently ranks in the top 6% nationally by National Cardiovascular Data Registry (NCDR) data, with rolling NCDR mortality in the 90th percentile for survival. Our electrophysiology (EP) colleagues perform more than 1,000 atrial fibrillation ablations each year. We are committed not just to volume, but to continuous improvement and outcomes across the continuum of care.
Tell us about Baystate Medical Center’s recent expansion.
In March 2023, we opened four new cath labs and two new EP labs, and have since added a third EP lab as volumes continue to grow. These labs allow us to bring the latest technology to our patients. We are also the largest ST-elevation myocardial infarction (STEMI) center in Massachusetts, accepting transfers from 10 hospitals. State-of-the-art labs ensure that whether it’s an emergency STEMI, a complex PCI, or a structural case, our teams can deliver the highest quality care with advanced imaging, physiology, and device platforms. Clinically, we’ve raised our game while facing the same pressures as other hospitals — doing more with less amid staffing challenges. It’s been satisfying to build a department that meets those goals without compromising patient care.
How important are imaging and advanced tools in your program?
They are essential for both patient care and fellow education. In the past 10½ months, we used intravascular imaging in more than 1,100 cases and performed nearly 400 physiology assessments. These tools are evidence-based, improve decision-making — especially for intermediate lesions — and elevate the quality of our interventions. They are also vital in training; we want fellows to understand not only how to open an artery, but how to apply evidence and imaging to optimize outcomes.

Research and education are recurring themes in your leadership. Can you share more?
We are active in clinical research as a leading enroller in multicenter trials and through investigator-initiated studies, with work focusing on STEMI shock and coronary physiology. We recently published on wall shear stress and outcomes in Computers in Cardiology and Biology.1 Research keeps us asking better questions and brings validated innovations back to our patients. Education is equally important. Our fellowship has grown to six general cardiology fellows, three interventional fellows, and one EP fellow annually, with plans to expand. We also host an annual educational conference — now in its 12th year — which has grown from 20 attendees in a hospital classroom to hundreds at MGM Springfield. That reflects our commitment to advancing knowledge within our institution and across the region.
How would you sum up what makes Baystate unique?
Baystate is a bit of a hidden gem. We deliver high-volume, high-quality care in a community setting while sustaining the research and education expected of an academic center. Most importantly, we do it through a culture of collaboration, transparency, and continuous improvement. With the right commitment, you can build a world-class cardiovascular program anywhere in the country.
Dr. Goldsweig, could you describe the heart and vascular program at Baystate?
Baystate has always been a major regional presence, but over the past decade, our programs have grown substantially, both in volume and in sophistication. Today we perform over 1,500 PCI procedures a year, more than 400 TAVR procedures, and over 300 left atrial appendage occlusion (LAAO) cases annually. Those numbers continue to rise, and so does the complexity of what we can offer patients locally. As a group of roughly 30 cardiologists, we provide the full spectrum of cardiovascular care, from primary prevention to multi-valve replacement, left ventricular assist devices, extracorporeal membrane oxygenation (ECMO), and beyond.
You recently oversaw the modernization of Baystate’s cath labs, opening an entirely new suite with four cath labs, as well as two EP labs, a neuro lab, and a flex lab. What did that involve?
For cardiology alone, we went from two aging cath labs to four brand-new rooms, each equipped with Philips Azurion FlexArm systems. The result was a tremendous upgrade. Not every interventional team gets to rebuild its department from the ground up. We were fortunate to move into an entirely new space rather than renovating in place. We finished procedures in our old rooms on a Friday and came in on Monday to find ourselves in an entirely new, state-of-the-art facility.
Why did you choose ceiling-mounted FlexArm systems, and how have they changed your workflow?
Philips Azurion FlexArm is a ceiling-mounted system that can move around the patient in virtually any configuration. That capability is important because structural heart disease procedures often require anesthesia at the head of the bed, echocardiographers at the left shoulder, and plenty of ancillary equipment. With a fixed C-arm, accommodating all of that can be frustrating. The FlexArm eliminates those bottlenecks.
From a scheduling perspective, standardization was also key. We designed each of the four rooms to handle any type of procedure, whether PCI, TAVR, mitral valve transcatheter edge-to-edge repair (M-TEER), LAAO, or peripheral intervention, without compromise. Such flexibility avoids inefficiencies like having a “structural room” that sits empty if another case runs late. Every lab is fully equipped, which makes case flow much smoother. The large detector systems give us maximum versatility. We sacrifice a bit of angulation compared to smaller detectors, but we can perform any procedure in any room. That flexibility is especially critical as structural case volumes continue to grow.
How have the new Philips systems helped with efforts around radiation reduction?
Radiation safety is a priority for both patients and staff. Philips’ ClarityIQ algorithm has cut patient radiation exposure by about 70% compared to our previous systems.2 We can now perform long chronic total occlusion cases while keeping kerma well under 500 mGy. For operators, we use RADPAD scatter shields for every case, along with 0.5 mm lead aprons, caps, and eyewear. We trialed some advanced shielding systems but found they didn’t integrate well with workflow. Between ClarityIQ and RADPAD, our team feels protected while maintaining efficiency.
Another valuable feature is the ability to adjust dose on the fly. From the tableside controls, I can toggle between three “fluoro flavors.” Most of the time we work at the lowest dose and at 7.5 frames per second, but if I need to see fine detail, I can temporarily increase the dose and then step right back down. That balance of safety and image quality is a big advantage.
What strategies have you implemented to help with contrast reduction?
Acute kidney injury is one of the most serious complications of PCI. We have established a departmental priority to minimize contrast exposure. Philips’ Dynamic Coronary Roadmap feature overlays previously acquired cine angiograms as “ghost images,” allowing us to navigate without repeating injections. When used, Dynamic Coronary Roadmap been shown to reduce contrast in PCI by more than 28%.3 We have also hardwired best practices into our workflow. During the pre-procedure time-out, we state the patient’s creatinine clearance and a maximum allowable contrast dose (three times the creatinine clearance). Every operative report includes the actual contrast used. And every patient is enrolled in a hydration protocol modeled on the POSEIDON trial, using left ventricular end-diastolic pressure (LVEDP) to guide fluid administration. Together, these steps have dropped our acute kidney injury rate from middle-of-the-pack to the lowest 10% nationally, according to recent NCDR data. That degree of renal protection is a tangible patient benefit.
Can you share more about your use of physiology and intravascular imaging?
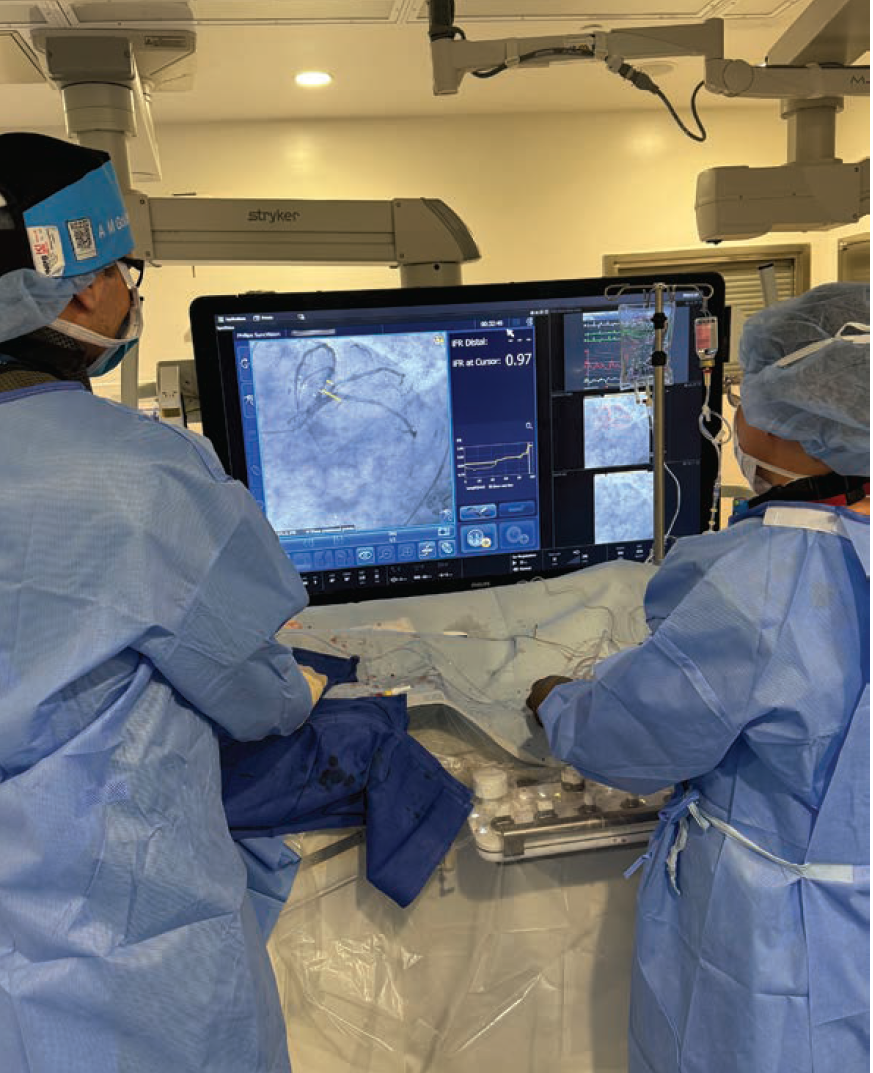
We use physiology in roughly 25% of cases and intravascular imaging in nearly 100%, so these technologies are absolutely central. With the IntraSight platform integrated into the Azurion system in each room, IVUS and instantaneous wave-Free Ratio (iFR) are literally at our fingertips, allowing us to assess vessel function and structure in real time during PCI. The Philips IVUS is plug-and-play, so we can quickly place a catheter and perform a pullback to evaluate stent landing zones and vessel size. A major step forward has been the integration of IVUS and iFR Co-registration. We no longer just have an angiogram and a separate IVUS pullback. Instead, the two are linked. I can click on the angiogram and see exactly what the IVUS shows at that location. With iFR, without the use of hyperemic agents, we can localize ischemia to precise spots in the vessel, down to hundredths of a unit. That precision eliminates geographic miss and ensures complete revascularization. The use of co-registration also reduces the number of angiograms needed, which means less contrast and radiation, making our interventions more effective, efficient, and safer.
What tools do you rely on for structural heart interventions?
Imaging is everything in structural heart disease. For echocardiography, we use Philips EPIQ CVxi systems. For transesophageal echocardiography (TEE)-guided procedures, we have the choice of X8-2t and X11-4t probes. The latter is especially helpful for smaller patients or those who can’t tolerate a larger TEE.
A major advance has been the Philips VeriSight Pro 3D Intracardiac Echo (ICE) Catheter. VeriSight Pro delivers TEE-like images without the need for general anesthesia. About half of our LAAO cases are now performed with ICE under conscious sedation and with same-day discharge. Patients prefer ICE, which avoids anesthesia risks and improves throughput. If needed, we can seamlessly switch between ICE and TEE on the same platform, with the touch of a button.
Since we have both the Azurion X-ray and EPIQ echo systems from Philips, we are able to fuse live x-ray and live fluoro imaging using the EchoNavigator feature. EchoNavigator is controlled by the imager on the echo touchscreen and is displayed on the large cath lab FlexVision monitor. EchoNavigator is invaluable for tasks like septal crossing in M-TEER or navigating paravalvular leaks. The Azurion system recognizes the echo probe and projects its orientation onto the fluoro screen. The echo imager can place a virtual dot on the fluoroscopy screen at the site of the leak, giving me a target so I can easily cross at that site.

Baystate is also very active in clinical research. How have these technologies supported that work?
They have been a catalyst. We were leading enrollers in the IMPROVE trial, which will solidify the central role of IVUS in PCI. We have also led enrollment globally in the OCCLUFLEX trial of Occlutech’s new PFO closure device, with 37 patients enrolled. We are among the top enrollers in Medtronic’s EXPAND TAVR study for moderate aortic stenosis and are leading enrollment in the Cordis SELUTION drug-coated balloon trial, where we have enrolled 88 patients.
Cutting-edge imaging and interventional tools facilitate participation at the highest levels. This work also motivates our fellows and staff to be engaged in research, because they can see firsthand that we are helping to shape the future of the field.
Do you have advice for other programs considering a major lab renovation?
Start with a forecast of your procedure mix and how it may evolve. Structural heart disease is growing rapidly, and procedural indications are expanding. Diagnostic cath volumes are declining, while coronary computed tomography angiography is becoming more central. Ambulatory sites of service are also shifting, with PCI moving to ambulatory surgery centers in some states.
In sum, the key is to embrace change. Build flexibility into your lab design and your workflows, so you are ready not just for what you anticipate but also for what you can’t predict. And make sure the whole team is part of the planning process, including nurses, technologists, imagers, anesthesia, and surgeons, because everyone’s perspective helps build a lab that truly works.
How do Philips technologies position Baystate for future needs?
Philips has positioned its systems as platforms that evolve. We didn’t just buy today’s fluoroscopy; we invested in continuous updates and education. Philips provides ongoing in-servicing, software upgrades, and training. This relationship is a long-term partnership.
How would you summarize the impact of these upgrades on Baystate’s mission?
We are now positioned to deliver world-class interventional cardiology care for our community while advancing the science through research. The combination of high-volume experience, cutting-edge Philips technology, and a culture of quality improvement means our patients don’t have to travel to Boston or New York for advanced care. They can get the most advanced care right here in Springfield.
For me, the most gratifying part is knowing we are doing procedures more safely, meaning with less radiation, less contrast, and greater precision, while also leading clinical trials that will define best practices for years to come. That’s a rare and exciting combination, and it reflects the strength of the entire Baystate team.
This article is supported by Philips. MAT-5785. The opinions and clinical experiences presented herein are specific to the featured topic(s), are not linked to any specific patient and are for information purposes only. The medical experience(s) derived from these topics may not be predictive of all patients. Individual results may vary depending on a variety of patient-specific attributes and related factors. Nothing in this presentation is intended to provide specific medical advice or to take the place of written law or regulations.
References
1. Lotfi A, Caraeni D, Haider O, Pervaiz A, Modarres-Sadeghi Y. Computational fluid dynamics model utilizing proper orthogonal decomposition to assess coronary physiology and wall shear stress. Comput Biol Med. 2025 Apr; 188: 109840. doi:10.1016/j.compbiomed.2025.109840
2. Buytaert D, Eloot L, Mauti M, et al. Evaluation of patient and staff exposure with state of the art X-ray technology in cardiac catheterization: A randomized controlled trial. J Interv Cardiol. 2018 Dec; 31(6): 807-814. doi:10.1111/joic.12553
3. Hennessey B, Danenberg H, De Vroey F, et al. Dynamic Coronary Roadmap versus standard angiography for percutaneous coronary intervention: the randomised, multicentre DCR4Contrast trial. EuroIntervention. 2024 Feb 5; 20(3): e198-e206. doi:10.4244/EIJ-D-23-00460
Find More:
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Renal Denervation Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center












