Beyond the Band: Evolving Solutions for Transradial Hemostasis
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Transradial Technologies with Gautam Kumar, MBBS, MRCP(UK), FACC, FASE, FSCAI1, and Bailey Ann Richardson, NP-C, RNFA, CNOR, RCIS2
1Professor of Medicine, Emory University School of Medicine; Grady Memorial Hospital, Atlanta, Georgia;
2Interventional Cardiology Nurse Practitioner, Austin, Texas
Disclosures: Dr. Kumar and Bailey Ann Richardson report no conflicts of interest regarding the content herein.
Dr. Gautam Kumar can be contacted at gautam.kumar@emory.edu.
Bailey Ann Richardson, NP-C, RNFA, CNOR, RCIS, can be contacted at baileyestesnp@gmail.com.
Click here for a PDF of this article. Logging in or registration may be required (it's free!).
Since first described by Dr. Lucien Campeau in 1989, the transradial approach (TRA) to cardiac catheterization has steadily gained momentum, with widespread adoption accelerating over the past two decades.1 Today, TRA is the preferred method for many interventionalists worldwide due to its clear benefits: improved patient comfort, reduced access site bleeding, shorter recovery times, and earlier ambulation compared to transfemoral access.2
As TRA continues to dominate the interventional cardiology landscape, attention has increasingly shifted to optimizing post-procedural management, particularly radial artery closure. The current standard, external compression bands, has been instrumental in enabling TRA’s rise but is not without significant limitations. Vascular complications, including radial artery occlusion (RAO), the most frequently encountered issue, with reported incidence ranging from 5% to 12% as well as hematoma formation, pseudoaneurysm, and arteriovenous fistula, remain pressing concerns.3 Although many RAO cases go undetected due to their asymptomatic nature, the implications are significant, potentially compromising future access for coronary artery bypass grafting or dialysis.
In addition to vascular issues, neurologic and device-related complications have emerged. Excessive compression or improper technique during hemostasis can contribute to nerve injury or complex regional pain syndrome. Meanwhile, the labor-intensive nature of current compression band protocols, marked by extended removal times, frequent patient monitoring, and inconsistent patient comfort, underscores the urgent need for innovation.
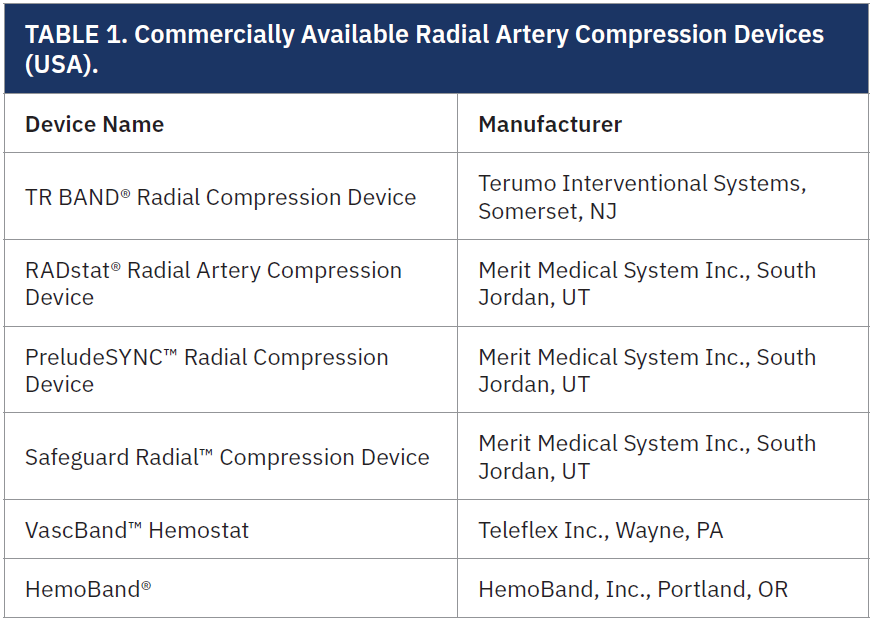
As TRA becomes the global standard, the drawbacks of legacy closure techniques are coming into sharper focus. Suboptimal hemostasis strategies not only affect outcomes but may also contribute to slower adoption of TRA in certain regions of the world, such as the United States. These realities highlight the need for next-generation solutions that improve procedural efficiency, reduce complications, and enhance both the patient and provider experience (Table 1).
Answering the Call for Innovation
Recognizing the unmet need in radial artery hemostasis, Dr. Gautam Kumar, an interventional cardiologist at Emory University in Atlanta, Georgia, has been working on several techniques that focus on optimizing clinical safety and improve procedural workflow.
As interest grows in refining the patient experience and reducing staff workload, the introduction of new closure technologies stands to redefine our approach to radial access recovery. Innovations in this space could represent a pivotal shift in how we manage hemostasis- potentially reducing complication rates, shortening recovery time, and freeing up valuable nursing resources.
The Problem With Status Quo
As highlighted by Dr. Kumar in a recent cross-disciplinary meeting, the most used radial artery compression devices, while effective at prevention overt bleeding, often fall short due to inconsistent outcomes, time-consuming protocols, and limited adaptability across patient populations.
“We’ve known for years that complications, while clinically silent in many cases, compromise future access and patient outcomes,” said Dr. Kumar. “It is important to address that directly from a physiology and workflow standpoint.”
Current hemostasis protocols ongoing assessment and site management, placing added strain on cath lab teams and introducing variability in care. While many of these complications go unnoticed due to a lack of symptoms, they can jeopardize future vascular access and long-term patient care options.

We invited interventional cardiology nurse practitioner Bailey Ann Richardson, AGNP-C, MSN, RN-BC, RCIS, RNFA, into a discussion with Dr. Kumar to gain practical insight into how innovation might be adopted on the front lines.
What method are you currently using post-radial access?
Bailey: Most labs continue to rely on external compression bands. While there are slight differences between brands, they all follow the same basic principles of compression and timed weaning. These devices have been widely adopted, but their application is still manual and labor-intensive.

Dr. Kumar: Exactly. These bands served us well in early transradial practice, but they haven’t evolved to meet modern demands. We need closure solutions that are more precise, more efficient, and less dependent on constant nursing intervention.
Are you familiar with and using patient hemostasis protocols?
Bailey: Yes, I follow patent hemostasis protocols when feasible. The challenge is consistency. In real-world conditions with high patient volume or staffing shortages, it’s difficult to maintain the level of oversight required to do it correctly every time.
Dr. Kumar: And that is a major driver behind our push for innovation. We want to eliminate the guesswork. The ideal device should maintain arterial patency without relying on precise, technician-driven adjustments. It should simplify the process and minimize error by design.
How would you describe your experience with pressure band devices?
Bailey: Pressure bands are the current standard in the cath lab. They have simplicity of use with a relatively short learning curve. When applied and monitored properly, there tend to be few complications. Once the patient leaves the lab and goes to recovery is when we tend to have more complications, especially as the patient becomes more mobile. Often, this can be managed by the recovery team, but on occasion, the specialists in the lab are called to provide assistance. Proper application, monitoring, and frequent adjustments all take time; time that could be spent on higher-level patient care.
Dr. Kumar: Exactly. Current devices introduce variability into care and require a high degree of manual involvement. That kind of inefficiency is not sustainable for today’s cath lab. We need tools that are more reliable, hands-free, and workflow friendly.
Do patients often complain about discomfort when using current pressure devices?
Bailey: Yes, more often than you’d expect. Common complaints include tightness, pain, and bruising. While the discomfort may not always be severe, it impacts the patient’s perception of the procedure and their overall experience.
Dr. Kumar: Patient comfort isn’t just about hospitality; it is directly tied to outcomes and satisfaction. Devices should achieve hemostasis without compromising patient well-being.
How valuable would a hands-free, self- regulating closure device be?
Bailey: Incredibly valuable. A device that self-regulates would mean faster patient turnover, fewer complications, and reduced burden on nursing staff. It would be an asset and much needed innovation for the cath lab.
Dr. Kumar: It would be great to introduce a smart closure solution that adapts in real time, maintains safety, and removes unnecessary complexity. Reducing both the cognitive load and hands-on requirements for staff is critical as procedure volumes continue to grow.
Final Thoughts
Reimagining radial closure is more than a technical upgrade; it is a clinical imperative. By embracing smarter, more intuitive technologies, we can reduce complications, alleviate the burden on cath lab teams, and deliver a more seamless recovery experience for patients. As transradial access continues to dominate the landscape, it is time for our closure strategies to evolve in parallel — prioritizing safety, efficiency, and patient-centered care.
“The inclusion of follow-up ultrasound would make these strategies even stronger,” said Dr. Kumar. “We’re not just stopping the bleed; we’re preserving the artery for future use.”
References
1. Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989;16(1):3-7. doi:10.1002/ccd.1810160103
2. Rao SV, Cohen MG, Kandzari DE, Bertrand OF, Gilchrist IC. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55(20):2187-2195. doi:10.1016/j.jacc.2010.01.039
3. Bajraktari G, Rexhaj Z, Elezi S, Zhubi-Bakija F, Bajraktari A, Bytyçi I, Batalli A, Henein MY. Radial access for coronary angiography carries fewer complications compared with femoral access: a meta-analysis of randomized controlled trials. J Clin Med. 2021;10:2163. doi:10.3390/jcm10102163












