Think Proximal: Recognizing Lumbosacral Spine Disorders in Foot and Ankle Presentations
Lower extremity pain, numbness, or weakness frequently presents to podiatry as an isolated foot problem, yet a substantial proportion originates proximally from the lumbosacral spine or nerve roots. Because radiculopathy and stenosis often occur without back pain, podiatrists must maintain a high index of suspicion—in this article, the author outlines key concepts to consider.
Key Takeaways
- Dermatomal sensory changes, subtle motor deficits, posture-dependent symptoms, and bilateral complaints may suggest lumbosacral pathology rather than isolated foot disease.
- A focused neurologic exam including myotomes, dermatomes, reflexes, neurodynamic tests, and gait can quickly identify clinically meaningful radiculopathy.
- Failure of foot-directed care or presence of red flags should prompt timely imaging, electrodiagnostics, systemic evaluation, and interdisciplinary referral.
Lower extremity sensory and motor disturbances and weakness often present first to podiatric offices, where patients may self-diagnose neuroma, diabetic neuropathy, fat pad atrophy, or a localized entrapment syndrome. Yet a substantial proportion of these complaints originate from the lumbosacral spine and nerve roots, even in individuals without back pain or sciatica. Contemporary guidelines emphasize that radicular and nerve root-level disorders frequently masquerade as foot, ankle, and lower leg pathology, and clinician should consider this whenever symptoms span dermatomal territories or involve mixed motor-sensory findings.1
Modern sedentary behavior with decreased walking, reliance on rideshare transportation, e-bikes replacing traditional cycling, and prolonged sitting, has accelerated spinal deconditioning. In my personal observation, back symptoms increase roughly 10% per decade; for example, 60% of 60-year-olds have back etiology. The mechanical stressors of childhood through older adulthood makes proximal drivers of foot complaints increasingly common. Because podiatry is often the first point of contact, podiatrists serve as essential gatekeepers within the neuromusculoskeletal system. Nerve symptoms in the feet should prompt consideration of systemic illness, vitamin B12 deficiency, diabetes, chemotherapy and radiation-related neuropathy, or lumbosacral pathology, rather than assuming a purely local cause.2
Why Podiatrists Must Think Proximally
The lumbosacral complex can generate symptoms that clinically resemble otherwise primarily lower extremity conditions: chronic heel pain; tarsal tunnel syndrome; Mortons neuroma; diabetic neuropathy; peroneal tendinopathy; exertional leg pain; or nonspecific polyneuropathic patterns.3 Patients frequently describe radicular paresthesias simply as “foot pain,” even when the underlying distribution is clearly dermatomal. Because many individuals with lumbosacral pathology do not report back discomfort, podiatrists must maintain a high index of suspicion whenever the history or examination does not align with a purely local diagnosis.
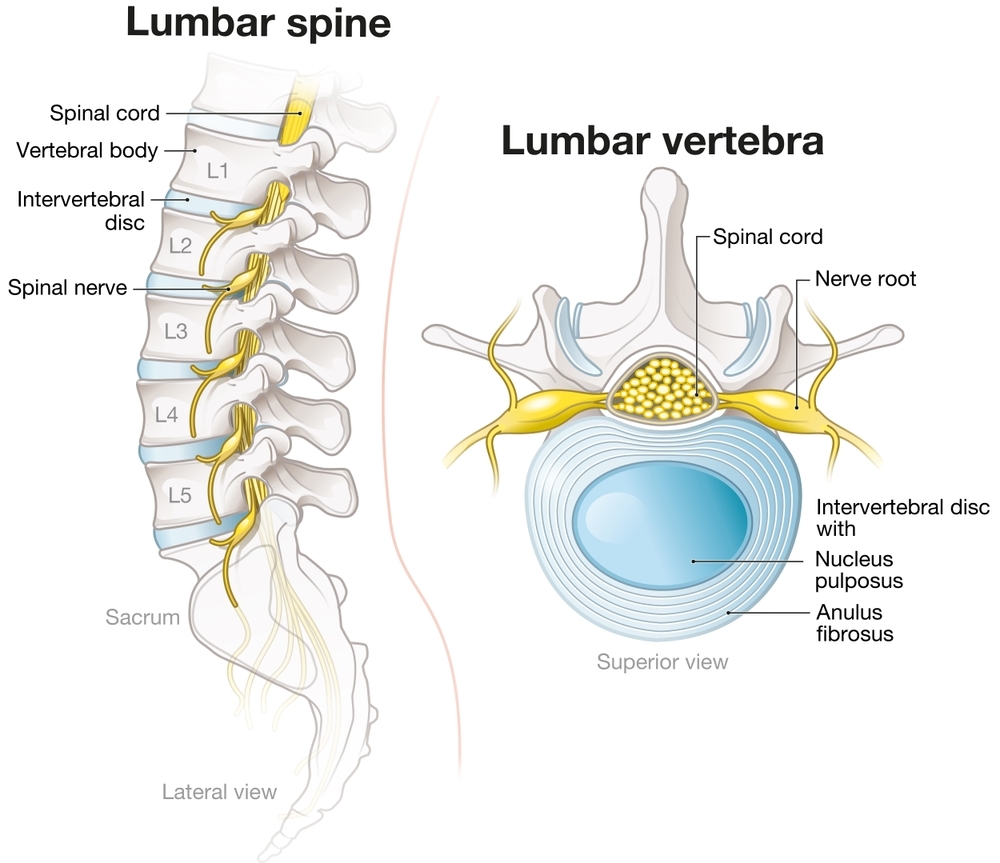
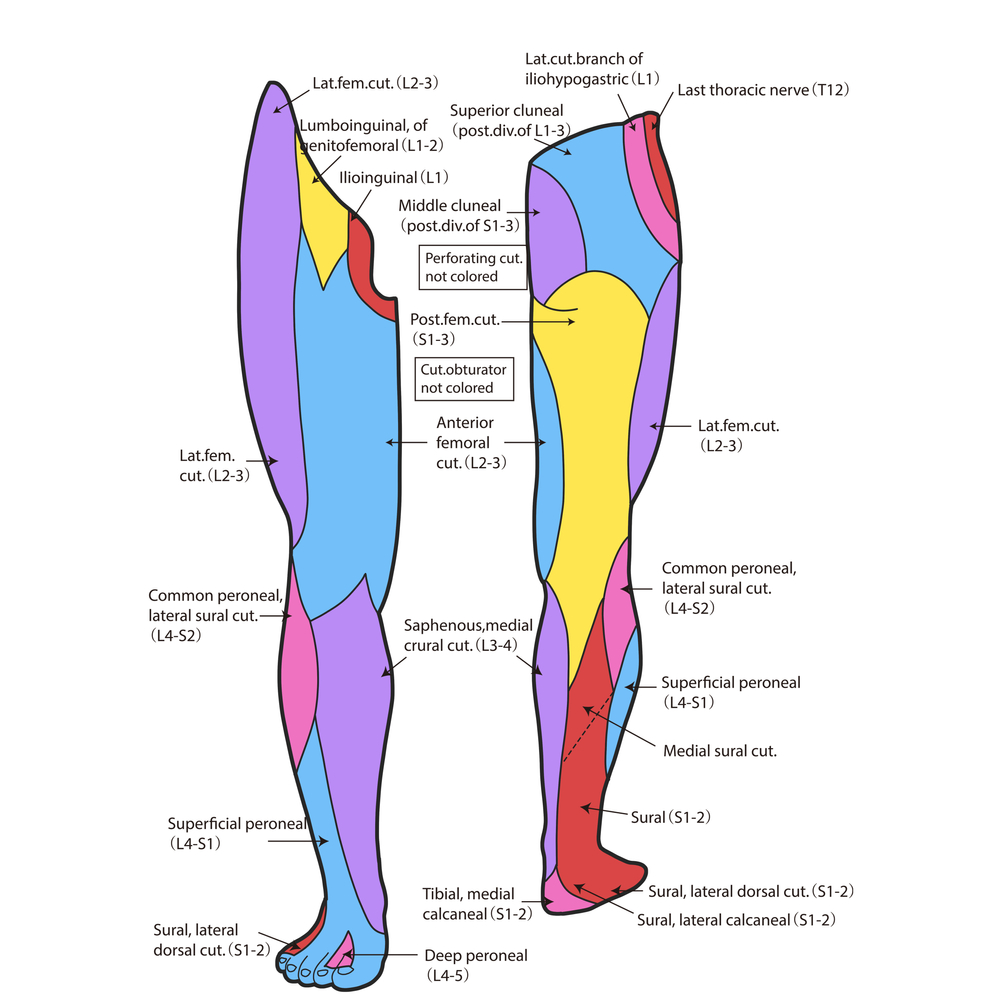
Several clinical features should trigger consideration of a proximal source. When pain is poorly localized, migratory, or disproportionate to physical examination, this may signal radiculopathy rather than mechanical foot pathology. Sensory changes following a dermatomal distribution—medial ankle or leg in L4, dorsum of the foot in L5, or the lateral foot and plantar heel in S1—favor root involvement over tibial or peroneal nerve entrapment. Subtle motor deficits may be even more diagnostically significant: difficulty heel walking can indicate L5 dysfunction, difficulty toe walking suggests S1 involvement, and inability to perform a single-leg heel raise is one of the most sensitive signs of S1 pathology that I see in my practice.
Symptom behavior modulated by spinal mechanics is also informative. Leg symptoms aggravated by sitting, forward flexion, coughing, or Valsalva maneuver can often reflect discogenic radiculopathy, whereas symptoms provoked by standing or ambulation and relieved by leaning forward (the classic “shopping cart sign”) suggest neurogenic claudication from lumbar stenosis. Bilateral foot or leg symptoms, gait unsteadiness, and leg heaviness frequently point toward stenosis and are rarely explained by isolated entrapment neuropathies. Often, symptoms are more noticeable at night, or in different positions, such as sliding out of a car or sitting on an uneven couch for extended periods of time.
A lack of improvement despite appropriate foot-directed care warrants reevaluation. Patients treated repeatedly and unsuccessfully for plantar fasciitis, neuroma, or tendinopathy often prove to have radiculopathy, stenosis, or systemic neuropathy once the provider views the clinical pattern proximally.
Look, listen, feel, and watch the patient. It is critical in diagnosis. In my experience, a brief, structured screening exam can identify most clinically meaningful radiculopathies in less than 90 seconds. Key elements that I include are:
- assessment of knee extension (L4);
- ankle dorsiflexion and great-toe extension (L5);
- plantarflexion via single-leg heel raise (S1);
- sensory testing across L4–S1 dermatomes;
- patellar and Achilles reflexes; and
- straight leg raise or slump test that reproduces leg symptoms.
Gait evaluation—detecting foot slap (L5), weak toe-off (S1), or wide-based ambulation (stenosis)—helps provide additional localization. Maintaining this proximal mindset does not require podiatrists to practice as spine specialists; rather, it ensures early recognition of conditions that would otherwise be misattributed to the foot, enabling timely referral and preventing unnecessary procedures.
Index of Suspicion: Key Clinical Patterns
Lumbar Radiculopathy. Dermatomal pain patterns are central to radiculopathy. L5 symptoms typically radiate along the lateral leg to the dorsum of the foot, while S1 symptoms involve the posterior leg and plantar surface. Myotomal weakness and reflex changes often mirror these sensory findings. Neurodynamic tests such as the straight leg raise and slump test are well-validated for detecting radicular involvement.4,5 Dermatomal pain accompanied by objective neurologic findings strongly supports a proximal etiology over a primary foot condition.
Lumbar Spinal Stenosis and Neurogenic Claudication. Patients often describe bilateral leg heaviness, aching, or paresthesia that worsens with standing or walking and improves with sitting or forward flexion. Clinical guidelines highlight the importance of distinguishing neurogenic claudication, which typically presents with normal pulses and clear posture-related modulation, from vascular insufficiency.6 Symptoms often worsen at night when individuals remain in fixed positions, which further narrows foraminal spaces.
Lumbosacral Radiculopathy. Lumbosacral radiculopathy involvement produces multifocal, frequently asymmetric weakness with severe proximal pain. Diabetic lumbosacral neuropathy is well described and may include systemic features such as unintentional weight loss.7 Neoplastic, traumatic, or iatrogenic plexopathies can present similarly. Distal symptoms often mislead clinicians toward podiatric diagnoses unless the patient undergoes a proximal screening.
High-Risk Spinal Pathology. Red flag findings including saddle anesthesia, new bladder and bowel dysfunction, rapidly progressive bilateral weakness, infection risk, or history of cancer, warrant immediate imaging and neurosurgical or additional consultation. Some individuals present solely with bilateral leg or foot sensory loss, so structured questioning is essential.
Patterns Suggesting a Proximal Source. Symptoms crossing multiple peripheral nerve territories, fluctuating with posture, or worsening at night should prompt proximal evaluation. Vague calf sensations, intermittent heaviness, or unexplained gait changes often reflect lumbosacral pathology rather than local foot disease.
Focused Examination: Clues to a Lumbosacral Origin
A concise neurologic evaluation provides exceptional diagnostic value. Strength testing across L4–S3 myotomes, reflex assessment, and sensory examination of L4–S3 dermatomes can identify subtle asymmetries.5 Neurodynamic maneuvers previously discussed, such as straight leg raise and slump testing are particularly helpful when they reproduce leg symptoms rather than back discomfort.4
Gait observation may reveal L5 foot slap, S1 toe-off weakness, Trendelenburg compensation, or wide-based cautious ambulation in stenosis. A careful history, particularly around nocturnal symptoms, postural relief, systemic factors (diabetes, vitamin deficiencies), chemotherapy exposure, or recent activity changes, often clarifies the clinical picture.
Diagnostic Workup
Imaging. Flexion-extension X-rays and lumbar magnetic resonance imaging (MRI) are indicated when objective neurologic deficits, dermatomal sensory loss, positive neurodynamic findings, progression of symptoms, or failure of foot-specific treatments suggest proximal pathology. The North American Spine Society supports selective MRI use guided by neurologic correlation rather than nonspecific back pain.1
For patients presenting with foot drop due to lumbar degenerative disease, a recent meta-analysis involving 918 individuals demonstrated that lumbar decompression produced at least one manual muscle testing (MMT) grade improvement in 82% of cases and full or near-full recovery (MMT 4–5) in 60%, while 18% experienced no improvement.9 These findings reinforce decompression as the preferred treatment in appropriate candidates and emphasize the importance of early recognition of radicular causes within podiatric pathology.
Electrodiagnostic Testing (EMG/NCS). EMG and nerve conduction studies reliably distinguish radiculopathy from distal entrapment neuropathies and can reveal plexopathy or multifocal disease. Electrodiagnostics are especially valuable when symptoms persist postoperatively despite adequate decompression. In one recent case, new contralateral calf pain and foot drop after lumbar decompression were ultimately attributed to common peroneal entrapment neuropathy on electromyography (EMG) testing rather than recurrent radiculopathy.8 You, as a podiatrist, must align yourself with a skilled specialist who does EMG tests.
Laboratory Evaluation. Targeted labs such as hemoglobin A1c (HbA1c), vitamin B panel, thyroid function tests, and inflammatory markers, assist in identifying systemic neuropathies that may coexist with or mimic radiculopathy. Such evaluations are critical when bilateral or atypical patterns are present.
Systemic and Peripheral Mimics. Peripheral neuropathy typically follows a symmetric stocking distribution rather than a dermatomal one. Entrapment neuropathies are usually focal and mechanistically reproducible. Vascular claudication (arterial or venous) typically improves with rest rather than spinal flexion. Systemic diseases such as rheumatoid arthritis or chemotherapy-induced neuropathy may produce mixed presentations.
Perioperative neuropathies, particularly common peroneal nerve injuries after lumbar surgeries, are another key mimic; these injuries often present as postoperative calf pain or foot drop even when spinal imaging is reassuring.8 Recognizing these mimics prevents diagnostic anchoring and supports comprehensive evaluation.
Building the Referral Loop: Podiatry, PM&R, Neurology, Nonsurgical Orthopedics
Podiatrists may initially receive referrals for such cases from primary physicians. As the podiatrist, you are the one who initiates the initial evaluation and diagnostic testing. You navigate your part of the pathway by identifying atypical patterns, performing focused neurologic screening, ordering appropriate imaging or electrodiagnostics, and recognizing red flags. Physical medicine and rehabilitation (PM&R) physicians contribute detailed spine evaluation, further gait analysis, rehabilitation planning, and interventional procedures. Neurologists are integral when differentiating radiculopathy from plexopathy, systemic neuropathies, or rapidly progressive neurologic disease. Personal trainers, yoga instructors, pilates trainers, and physical therapists are also common referral sources who initiate contact with you as the podiatrist.
Clear communication—detailing dermatomal patterns, motor findings, reflex changes, neurodynamic results, and systemic considerations—ensures efficient interdisciplinary management. Patients often return to podiatry for long-term gait optimization, orthotic management, and limb preservation once proximal pathology is addressed.
Dr. Romansky is a fellowship-trained Diplomate of the American Board of Foot and Ankle Surgery and part of the Podiatry Today Editorial Advisory Board. He is a team podiatrist for the US Men's and Women's National and World Cup Soccer teams, a design consultant to multiple shoe gear companies, and a medical consultant to many of Philadelphia's professional sports teams. Most recently, Dr. Romansky has been working as a health consultant for the Major League Baseball Umpires Association (MLBUA). He is also on the Board of Directors for the Gout Education Society.
References
1. North American Spine Society. Evidence-Based Clinical Guidelines for Multidisciplinary Spine Care: Diagnosis & Treatment of Lumbar Disc Herniation With Radiculopathy. North American Spine Society; 2020.
2. Hammi C, Yeung B. Neuropathy. [Updated 2022 Oct 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542220/
3. Alexander CE, Weisbrod LJ, Varacallo MA. Lumbosacral Radiculopathy. [Updated 2024 Feb 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430837/
4. McGill Spine Program. Lumbar Radiculopathy Clinical Pathway and Neurodynamic Testing. McGill University; 2021.
5. Orthobullets. Lumbosacral spine and lower extremity neurologic exam. Orthobullets. Published 2022. Accessed 2022.
6. Kreiner DS, Shaffer WO, Baisden JL, et al. Evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2013;13(7):734-743.
7. Dyck PJ. Diabetic lumbosacral radiculoplexus neuropathy. UpToDate. Accessed 2024.
8. Wang PW, Zhang Y, Li J, et al. Acute common peroneal nerve injury after posterior lumbar decompression: a case report. Front Surg. 2024;11:1329860. doi:10.3389/fsurg.2024.1329860
9. Than CA, Hajeir MY, Darwashi LMA, et al. Characterizing spinal decompression for foot drop caused by lumbar degenerative disease: a systematic review and meta-analysis. J Clin Med. 2025;14(13):4470. doi:10.3390/jcm14134470
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Podiatry Today or HMP Global, their employees, and affiliates.