STEMI Team Communication at Mount Sinai Hospital Using the STEMIcathAID App
What are the communication challenges faced by teams caring for acute myocardial infarction patients?
Ever since I can remember, the cath lab has dealt with ST-elevation myocardial infarction (STEMI) calls essentially the same way: a combination of phone calls, pager alerts, and emails alerts the response team. Inter/intra team communication has always been a challenge, with more than a dozen people involved in each case. Each person takes time to respond. Often we would struggle to understand where the patient was, and would have to call in and ask directly. Getting performance metrics after each case for the American Heart Association’s Mission:Lifeline registry was always a time-consuming task as well. Having an empty room is quite uncommon during the day in a busy cath lab, and knowing if the patient is 10 or 60 minutes out is crucial. At the end of the day, every little challenge adds seconds and results in delays.
Why was a phone app a good solution?
People have already had decades to improve how we handle phone calls and pagers, and at some point, it makes more sense to try something new. Our future is digital. Health records aren’t going back to paper and our messages aren’t going to be sent through an air system again. As more of our lives transition to the internet, the healthcare industry must adapt and adopt.
How does STEMIcathAID work?
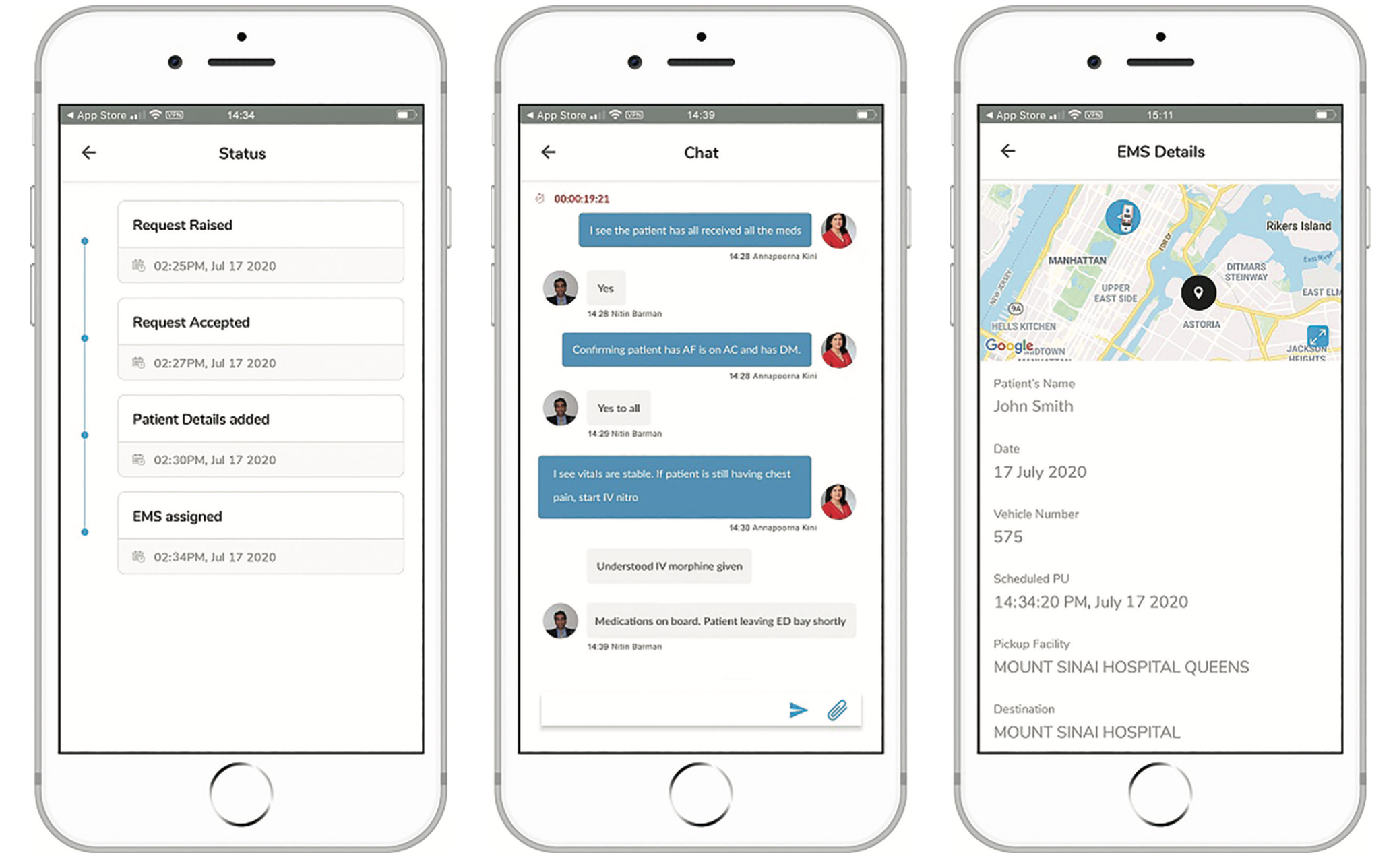
Multiple members are brought onto the case instantly via their phones. The app has secure shared data and chat features.
Here is how a transfer may look:
1. A referring physician suspects a STEMI and performs an electrocardiogram (ECG) as they normally would. They open the app and upload a picture of the EKG with some basic information. They click submit.
2. Simultaneously, the alarm is received within a couple of seconds by:
a. On-call cath lab attending for ECG review;
b. On-call cath lab fellow who will assist in the case;
c. Transfer center to dispatch and ambulance and help with sign-offs.
3. The emergency department (ED) and cath attendings discuss the case over the phone and decide if the patient is a good candidate for catheterization, if the patient is not a good candidate for cath, or if the patient is not but should still be transferred to the cardiac intensive care unit.
4. Only when the case is accepted by the cath attending are the nurses and technologists brought onto the case. They discuss medications, assess the status of the patient, and share any relevant information through fields in the application or the dedicated secure chat platform.
5. While the teams coordinate care, the GPS position of the ambulance is viewable, there are special notifications such as ‘cath lab ready to receive patient’, shock screening questions, and status notifications and updates.
There is no more struggle to gather the STEMI team because they are brought on within seconds, know where the patient is at all times, and are prepared with any special care the patient may require once he or she arrives. While the case is ongoing, everybody sees a running first medical contact clock to provide a sense of urgency and reminder to meet our metrics. After the case, we export everything for careful review.
What were the challenges around the app’s creation and implementation?
Security and compliance is paramount in healthcare. We also had to introduce a new system to hundreds of people of all ages and with varying degrees of tech-savviness. It wasn’t easy, but everybody is getting used to it and I don’t think we have any desire to go back to the old way now.
What was the impact of the COVID-19 pandemic?
Originally, we tried to start our pilot program right as COVID hit the world. Nothing has really changed for us; people are still having heart attacks. We just ask about COVID swabs now so we can use extra personal protective equipment for positive patients.
What do team members like about using the app?
People love the instant communication, not having to track down any missing persons, and knowing where the patient is so they can have them ready for ED departure or cardiac cath lab arrival. STEMIcathAID is not only novel, but it has genuine value in improving our patient care. People are excited to use it and wea are hearing interest both from other departments and outside of the health system.
What benefits have you seen thus far?
We plan on publishing our findings in the future, but we can say that there is a clear improvement across the board based on the Mission:Lifeline metrics. The patient spends less time in the ED and never waits for a room to clear out. A lost minute here and there may not feel significant, but the Mission:Lifeline registry treats time metrics as pass or fail. Both for the patients’ short- and long-term outcomes, as well as the performance metrics, every minute counts.
What do you plan for the future and any advice?
We plan on expanding app use to other emergencies, such as trauma and stroke, that can benefit from the communication features we rely on for STEMI. My advice for people looking to optimize current workflows is that sometimes incremental improvements can only do so much. Years of improving how we call each other on the phone and activate pagers can only be taken so far. Sometimes you need to come up with something new. n
Learn more about the STEMIcathAID app at www.STEMIcathAID.com










