My Last Day in the Cath Lab: A Personal Reflection
© 2025 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Morton J. Kern, MD, MSCAI, FACC, FAHA
Clinical Editor; Interventional Cardiologist, Long Beach VA Medical Center, Long Beach, California; Professor of Medicine, University of California, Irvine Medical Center, Orange, California
Disclosures: Dr. Morton Kern reports he is a consultant for Abiomed, Abbott Vascular, Philips, ACIST Medical, and Opsens Inc.
Dr. Kern can be contacted at mortonkern2007@gmail.com.
Click here for a PDF of this article. Logging in or registration may be required (it's free!).
 I retired last week. No, I’m not sick and not dying. I’ve already used up my 50 days of paid work for this year, and thus I’m out of the cath lab. I have mixed emotions about stepping out of the lab, and thought I’d share some of my thoughts on this life-changing event.
I retired last week. No, I’m not sick and not dying. I’ve already used up my 50 days of paid work for this year, and thus I’m out of the cath lab. I have mixed emotions about stepping out of the lab, and thought I’d share some of my thoughts on this life-changing event.
A Life in the Cath Lab
I love the cath lab, where I spent nearly all my professional career. Over my 40+ years, the cath lab has evolved dramatically and continues to grow, providing important advances in care for all heart patients.
In 1979, as a first-year cardiology fellow at the Brigham and Women’s hospital in Boston, I recall my first cases, scrubbing with Dr. Zoltan Turi, my second-year fellow. We did a right heart cath with a stiff 8 French (F) Cournand Dacron catheter. Like all trainees then, I had to observe cases for 6 weeks before advancing to First Operator spot for the left heart and coronary angiography. After the first few catheterizations, I knew invasive cardiology was for me. Thank you, Zoltan. Over the ensuing years, I enjoyed gaining experience and diving deep into how to do things better.
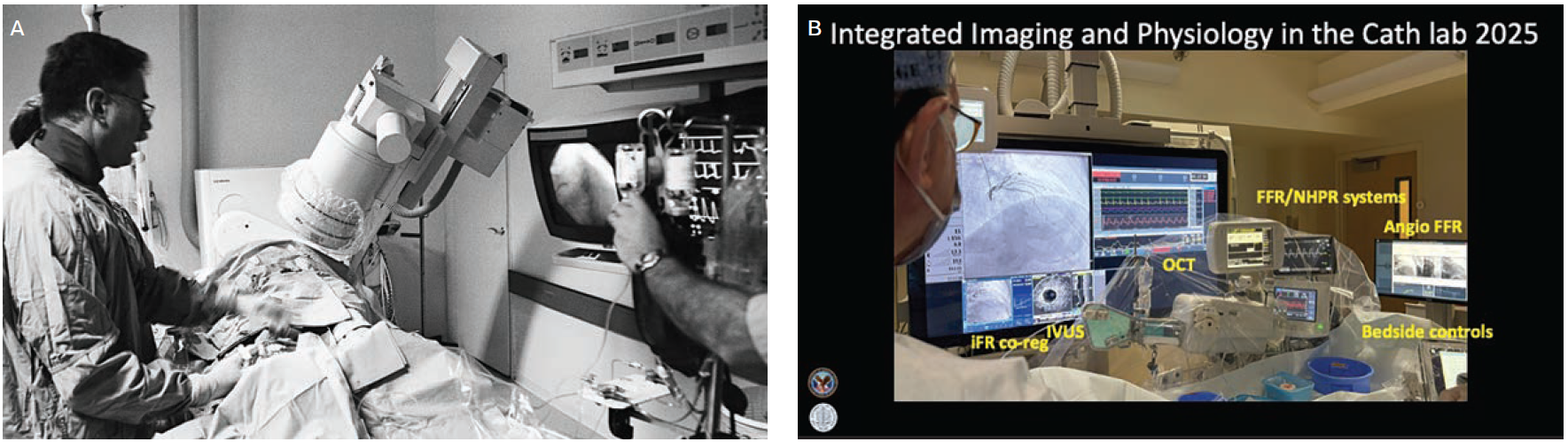
I think about how far we’ve come since then. On my last cath day, I was standing next to a freshly-minted first-year cardiology trainee. It was a bittersweet moment — a cliché, but true. How many fellows have I worked with? How many unusual patients and novel findings, and how many hemodynamic conundrums did we come across over 4 decades in the lab? Like other interventionalists of my generation, I marvel at the advances. Take a look at the 2 cath labs, in 1985 and in 2025 (Figure 1). In 1979, we only performed elective right and left heart caths, with ventriculography being a routine — no unstable patients, no congestive heart failure or ST-elevation myocardial infarction (STEMI) patients. We could not envision a world with percutaneous coronary intervention (PCI), stents, STEMI, thrombolysis, routine coronary physiology, computed tomography angiography, fractional flow reserve, mechanical support devices, and a myriad of other unworldly innovations in transcatheter aortic valve replacement and structural heart interventions. The specialties of electrophysiology, interventional cardiology, and heart failure had yet to be developed. Hundreds of novel techniques, procedures, and devices came out in the cath lab. I relish being part of that development and the feeling that we help make life wonderous for many patients.
The Cath Lab Handbook
I don’t know how I came to be a teacher. I found that the best way to really learn something is to teach it. I love working with fellows, residents, nurses, technologists, and students to share what I know and glean from them what I should, but don’t. As I reflect on my teaching, I am most proud of the ongoing editions of The Cardiac Catheterization Handbook, created not only for fellows but for all those who work in the cath lab and all those soon to pass through, working in the supporting industries advancing the field.
I’ve been asked how the Handbook came to be. Here’s the short version. As a fellow, Dr. William Grossman, my attending physician in the cath lab, mentor, and later, my friend, had written the definitive text on the subject. We used his book, Cardiac Catheterization and Angiography (2nd ed, 1980), as our bible. At our daily 4pm cath conference, we would sit around the conference table that was covered with hemodynamic tracings from the “E for M” electronic recorder, and discuss our findings. At some point, Bill would grab the chain attached to his book, pull it out from under the papers and read us a passage to settle any argument that we were having. I was in awe of this knowledge, and yet found the book complex, mysterious, and at times, incomprehensible. I thought about the fact that there was no simple introductory material for new fellows and nurses to initiate them to the lab and its routines.

Photo of Dr. Grüntzig, courtesy David Williams, MD. Middle image, reprinted with permission from Kern MJ, et al. Am J Cardiol. 1993 May 20;71(14):26D-33D. Image at right, reprinted from The New England Journal of Medicine, Grüntzig AR, Senning A, Siegenthaler WE. Nonoperative dilatation of coronary-artery stenosis: percutaneous transluminal coronary angioplasty., vol. 2, pages 61-68. Copyright ©1979 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
My first faculty job at the University of Texas, San Antonio, was where my first percutaneous transluminal coronary angioplasty (PTCA) took place, using Dr. Andreas Grüntzig’s original DG 4.5F balloon catheter (Figure 2). It really opened my eyes and stimulated me to learn more. After 3 years, I moved to St. Louis, Missouri, where I became co-director of the cath lab. PTCA rapidly evolved into PCI, with the advent of devices such as stents, and the industry around the cath lab flourished. As new fellows, nurses, techs, and industry representatives showed up in the lab every week, I realized there was no instruction manual to orient them in the cath lab. Robert Roth, RN, my Nurse Chief, colleague, and friend, helped me and my co-authors write the first Cardiac Catheterization Handbook, which was published in 1991. Its goal was to describe, in simple terms, what a cath lab is, how the lab works, who works there, and what information comes out of the procedures. It had
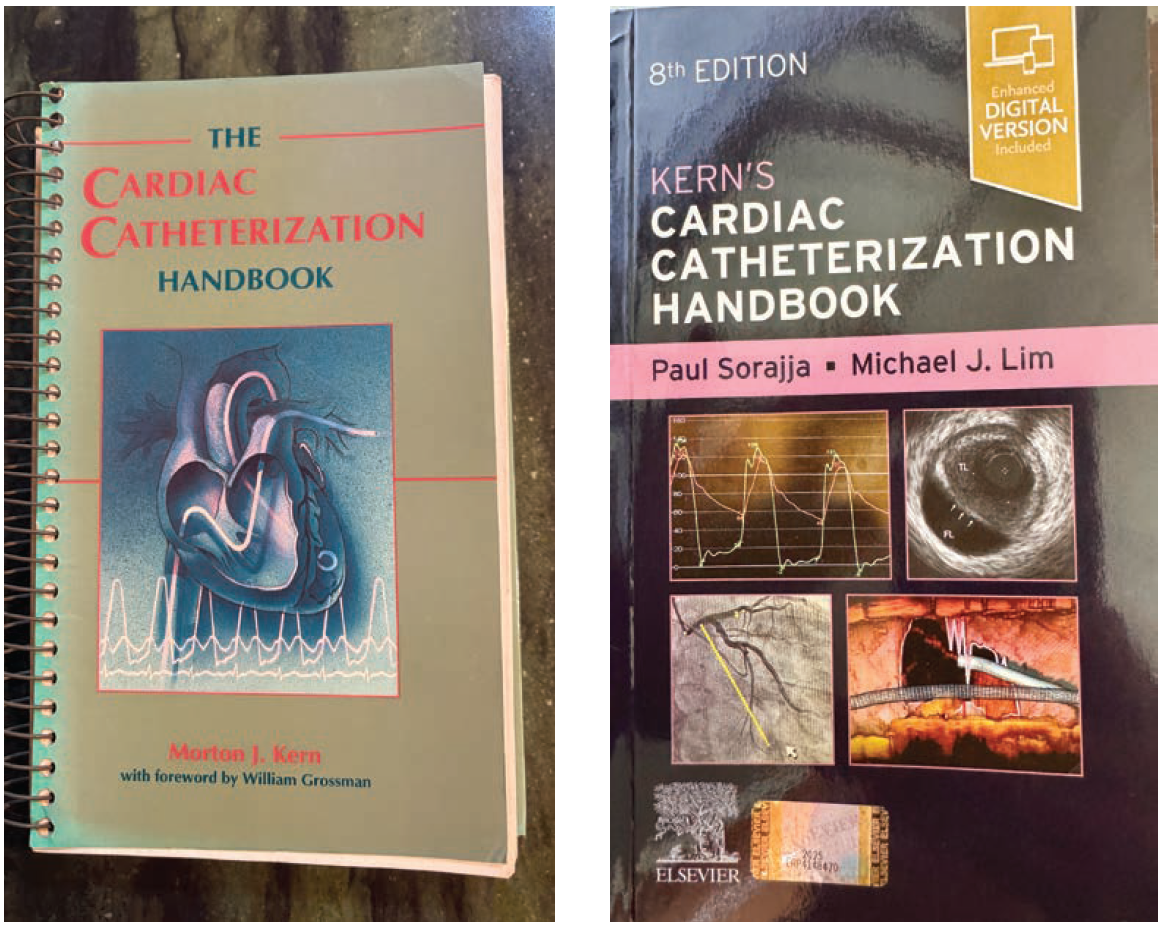
everything a fellow and nurse/tech needed to know to begin their lab rotation. As luck would have it, a Pfizer company representative bought 10,000 copies and gave them away as promotions, and the Handbook became an overnight success. The 8th edition of The Cardiac Catheterization Handbook was released in 2025 under the editorship of Drs. Mike Lim and Paul Sorajja. Thank you, Mike and Paul, for taking over this fulfilling work (Figure 3).
Thoughts for a New Trainee
What was I thinking on my last day in the lab? Mostly, the same things I was always thinking with a new fellow: I was guiding him/her through their initial experience and sharing my expectations of what they should learn by the end of their rotation. Here are a few of my tips:
For Fellows:
- Learn the routine.
- Communicate to the team.
- Keep your head in the game.
- Do what I show you. Don’t invent any new technique.
- Don’t talk too much.
- Don’t explain to me how to do the steps, just do them and I’ll catch you if you fall.
- Read and learn after you leave the lab for the day.
- “3 strikes and you’re out” — 3 chances to get ultrasound access the first week.
- Know your patient.
- Review the procedure before and after with the attending.
For Cath Lab Attendings:
- Be instructive but not intimidating.
- Explain to the fellows the meaning of “brevity, clarity and wit”.
- Be curious: ask why the findings are expected/unexpected.
- Emphasize that the patient’s safety and well-being are our top priorities above all else.
For the Nurses:
- Thanks for reminding me of things — heparin? GRF?
- Thanks for watching out for problems — Heart block? Hypotension? Agitation (both the patient’s and mine)?
- Keep your sense of humor.
For the Team:
- Rise above rudeness and stay professional.
Fall in Love With Concepts, Not Techniques
Every case presents an opportunity to learn something new. For example, I always like to examine the hemodynamics and discover new things. I inherited my love of hemodynamics from Dr. Bill Grossman, and my love of coronary physiology from Dr. William Barry. I thought my research with a coronary sinus catheter, measuring coronary venous outflow (reflecting antegrade coronary blood flow), would set the world on fire. While I was enthusiastic, the 2 Bills (Grossman and Barry) reminded me: “Don’t fall in love with a technique, fall in love with the concepts” — very true and especially useful to remember when thinking about research. In short order, coronary sinus thermodilution gave way to a Doppler catheter, and that yielded to a coronary Doppler guidewire. At the same time, translesional coronary pressure measured with an angioplasty pressure wire became a routine part of PCI, relegating the Doppler wire to a dusty research corner of the lab. But that’s a story for another day.
The Cath Lab Team
Every team makes the case smooth, protects the patient, facilitates a good result, and supports each other and the operators. Cardiac catheterization is a team sport. Every team and lab has a culture that evolves over time, as people come and go from the lab. I’ve always tried to cultivate an environment that uplifts everyone. Of all the things I’ll miss about the cath lab, it’s the camaraderie that I will miss the most.
The Bottom Line: Current and Future
I’ve written an Editor’s Page for Cath Lab Digest since 2006. Sharing my thoughts through CLD was one of the most rewarding activities around life in the cath lab. I enjoy collecting “Conversations in Cardiology”, writing about interesting cases and techniques, reviewing studies, and many other topics of interest both in and out of the lab. I thank Rebecca Kapur, the managing editor, her support staff, and the CLD team at publisher HMP Global. It is a great educational publication. (Just to remind you, I’m not dead yet, and hope to continue the CLD page for a while longer).
Over the coming years, I will follow my own teachings — keeping my eyes and mind open for new advances, and taking opportunities to discover better ways to help my colleagues, patients, friends, and family. My last day in the lab was the first day of a new journey, one I hope to share with you as a new ‘Bottom Line’ as I find my new way.
Further Reading
- Yu J, Kern MJ. Brevity, clarity and wit: 10 commandments for a 10-minute talk. Cath Lab Digest. 2019 Dec; 27(12):6-9.
- Kern MJ. What should a new team member do on day 1 in the cath lab? Cath Lab Digest. 2022 Aug; 30(8):6-9.
Find More:
Grand Rounds With Morton Kern, MD
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Peripheral Artery Disease Topic Center










