A Supply Cost Reduction Initiative
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Latisha Washington, MSN, RN, BSN, NE-BC, CNOR;
Dona Hoffman, MHA, RN, BSN, NE-BC
Advocate Sherman Hospital, Elgin, Illinois
Contact the authors:
Abstract
Advocate Sherman Hospital, a 255-bed community hospital, like others across the country, has seen a degradation in its overall profitability over the past five years. A series of financial deep dives were conducted involving local and system finance, hospital operations, medical group operations, nursing, and business development. A focus on direct contribution margin (DCM) meetings yielded a focus on Cardiovascular Services, procedural areas, Hospital Outpatient Department (HOD), inpatient settings and clinics to identify margin improvement. Strategies for cost reduction included supply standardization, leadership-physician collaboration, and utilizing system contract options for preferred products.
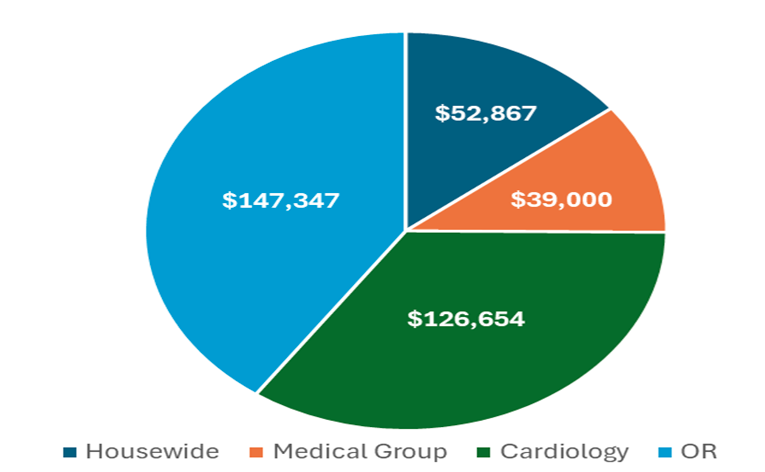
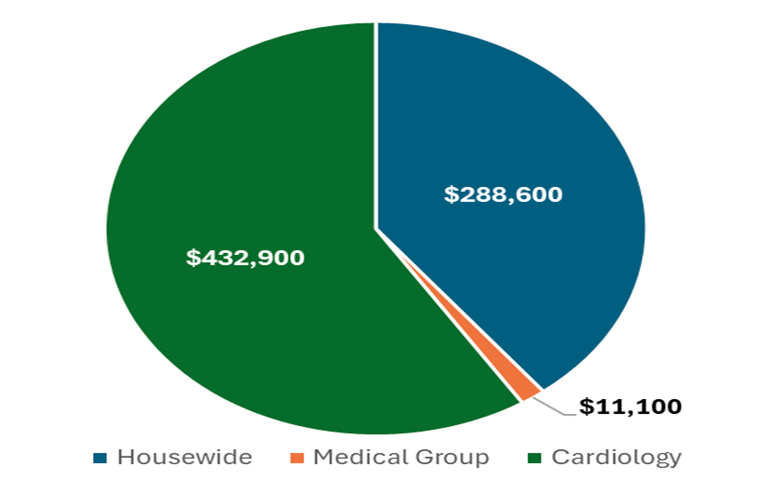
As a result of the work completed by the Supply Cost Initiative team, supply savings has yielded an estimated $365,868 for Q3 and Q4 2024 and a projected $732,600 for 2025. This workflow is being considered for adoption at other Advocate sites.
Local Problem/Purpose
An aggressive budget led to a focused review on supply cost reduction.
• Cardiovascular and Surgical Services were identified as top focus areas.
• As the initiative matured, the focus spread hospital wide, as well as to clinics and Immediate Care Centers.
• Lower cost with no impact to or identify improvement in quality.
Outcomes
• Successful cost reductions (see Figures 1-2) with no negative impact to quality outcomes.
• Implemented all product scanning in Cardiovascular OR and for Interventional platform (Cath lab and EP).
• Implemented welcome letter to physicians in their onboarding re: preferred supply and vendor alignment.
• Educated cath lab team on billing – aligned item sheets to ensure supply items were charged.
• Implemented a process to credit duplicate implants.
• Engaged hospital leadership and service lines in progress and identified savings.
• Presented data on the changes observed in patient outcome measures.
• Leadership, physician, and teammate engagement.
Approach
Cost Savings Initiative
• Executive team identified two co-leads
A multidisciplinary team was compiled including CNO, VP Business Development, Finance, Executive Director Cardiovascular Services, Director Perioperative Surgical Services, VP Supply Chain, Business Analyst, Business Manager, Manager Interventional Services and Manager Surgical Services.
• Team created a charter and identified prioritization and multiple workstreams for tracking progress.
• Implemented weekly meeting cadence
• Validated supply data and data sources
• Identified physician champion for each specialty area
• Change management included identifying, executing and monitoring tactics put in place
CNO provided each leader with a comprehensive supply list for review and efficiency recommendations. Each opportunity was shared with other Advocate sites.
• Worked with Pharmacy to reduce unnecessary and/or expensive medications.
• Implemented value analysis team (VAT)
Barriers
• Supply data: retrieval, validity, source, and timing
• Timing for implementation of identified opportunities and follow-up
Strengths
• Teamwork
• Organized approach – documentation and Monday meeting cadence.
Quality
Quality performance was maintained or enhanced through the implementation of supply adjustments.
Conclusion
This project demonstrated the value of multidisciplinary engagement in improving data-driven outcomes, with a notably high level of participation from clinicians, leaders and teammates. While data mining proved to be arduous and intensive process, it was essential for ensuring data validity and extracting meaningful insights. Our findings align with the growing recognition of collaborative approaches in healthcare analytics, though our project uniquely emphasized real-time collaborative engagement. Limitations include the manual nature of data extraction. Future work could encompass more targeted service line savings opportunities.
Implications for Practice
• Validate data and data source
• Engage front-line product utilization discussions
• Scan 100% supply items
• Validate billing practices and credit process
• Non-preferred or non-contracted item listing shared across sites
• Include service lines to include GI and Women’s Health
Acknowledgements
Latisha Washington – Director, Perioperative/Interventional Services
Dona Hoffman – Executive Director North Region, Cardiovascular Service Line
Sarah Christ – Business Intelligence Analyst
Rebecca Chung – NPD, Perioperative & Interventional Services
Trent Gordon – Vice President, Business Development
Travis Miller – Vice President, Supply Chain Management Operations
Susan Morby – CNO
Tina Schulz – Manager, Interventional Services
James Scott – Director, Supply Chain
Pete Weber – Business Manager (Retired)
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center
Go to Cath Lab Digest's Current Issue
Go to the Journal of Invasive Cardiology Issue










