The Roadmap to Cardiovascular Excellence: Strategic Steps for Hospital Leaders
© 2026 HMP Global. All Rights Reserved.
Any views and opinions expressed are those of the author(s) and/or participants and do not necessarily reflect the views, policy, or position of Cath Lab Digest or HMP Global, their employees, and affiliates.
Carol Wesley, MSN, MHA, RN
Senior Vice President at Corazon
Carol Wesley is a Senior Vice President at Corazon, offering program development for the Heart, Vascular, Neuroscience, Spine, Orthopedic, and Surgical service lines, with services in Consulting, Recruitment, Interim Management, Accreditation, and Peer Review. To learn more, visit www.corazoninc.com or call (412) 364-8200.
To reach the author, email carol.wesley@corazoninc.com
Click here for a PDF of this article, courtesy of Cath Lab Digest.
In today’s rapidly evolving healthcare landscape, cardiovascular (CV) care stands at the intersection of clinical innovation, operational complexity, and financial accountability. As heart disease remains the leading cause of death in the United States, hospital administrators face mounting pressure to deliver high-quality cardiovascular services that are both patient-centered and performance-driven.
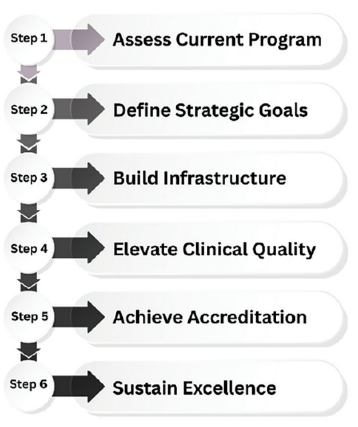
Achieving excellence in CV care is no longer a matter of incremental improvement. It requires a strategic, system-wide approach. From expanding service lines and integrating advanced technologies to optimizing workflows and elevating clinical outcomes, the journey to excellence demands thoughtful planning and execution. Each phase discussed below, from assessment and goal setting to accreditation, offers actionable strategies to help organizations align their CV services with national standards, market expectations, and long-term institutional goals. Whether your program is in its early stages or poised for expansion, this roadmap (Figure 1) provides a clear path forward to achieve measurable success and lasting impact.
Step 1: Assessing Your Current Program
The journey to cardiovascular excellence begins with a clear, honest understanding of where your program stands today. A thorough assessment is not simply gathering data, but a strategic process that uncovers the realities of clinical performance, operational efficiency, financial sustainability, and market relevance. For hospital administrators, this step lays the groundwork for informed decision-making and targeted improvement.
Why Assessment Matters
Without a comprehensive evaluation, even the most well-intentioned initiatives risk missing the mark. An effective assessment helps leaders:
• Identify high-performing areas to replicate or scale.
• Uncover inefficiencies that impact patient care and resource utilization.
• Reveal financial vulnerabilities or missed revenue opportunities.
• Understand how the program compares to national standards and competitors.
This process transforms raw data into actionable insights, guiding strategic planning and prioritization. A robust cardiovascular program assessment includes the program’s clinical performance, operational efficiency, the financial health of the program, and the organization’s market position.
• Clinical Performance: Evaluate outcomes including mortality, complication rates, and readmissions. Review adherence to evidence-based protocols and participation in national registries (e.g., American College of Cardiology’s National Cardiovascular Data Registry, Society of Thoracic Surgeons National Database).
• Operational Efficiency: Analyze patient throughput, cath lab and OR utilization, scheduling practices, and interdepartmental coordination. Identify bottlenecks and workflow gaps.
• Financial Health: Assess service line profitability, payer mix, reimbursement trends, and revenue cycle performance. Determine return on investment of existing technologies and staffing models.
• Market Position: Examine referral patterns, community demographics, competitive landscape, and service line differentiation. Understand how the program is perceived by patients and providers.
Benchmarking against national standards and peer institutions provides essential context, helping leaders understand where their program excels and where it lags. Corazon believes the assessment process provides the clarity and direction needed to move forward with confidence.
Step 2: Defining Strategic Goals

After thoroughly evaluating the current state of the CV program, including identifying accomplishments to date, the next essential step is to develop a strategy statement and develop well-defined strategic goals that will shape future direction and guide meaningful improvements (Figure 2). Corazon believes this is the phase where insight becomes intention. Data collected during the assessment is translated into a focused plan for improvement and growth.
Strategic goals serve as the compass for the program’s development, providing direction, establishing priorities, and ensuring that every initiative contributes to a broader vision of excellence. Goals should be aligned with the hospital’s overarching mission and tailored to the specific needs of the CV patient population, the competitive dynamics of the local market, and the institution’s long-term strategic objectives.
Goal setting is not a one-size-fits-all exercise, but regardless of scope, the process must be intentional, inclusive, and data-informed. By defining strategic goals early in the journey, hospital leaders create a roadmap that connects clinical aspirations with operational realities, ensuring that every step forward is purposeful, measurable, and aligned with the pursuit of CV excellence.
Aligning with Organizational Priorities
Cardiovascular services are often a cornerstone of a hospital’s clinical and financial performance. Therefore, goals should reflect and support system-wide initiatives such as:
• Expanding access to specialty care.
• Improving patient outcomes and satisfaction.
• Enhancing operational efficiency and cost-effectiveness.
• Strengthening market position and referral relationships.
By aligning CV goals with institutional priorities, hospital leaders ensure that resources are allocated effectively and that program growth contributes to overall success.
Setting SMART Goals for CV Program Success
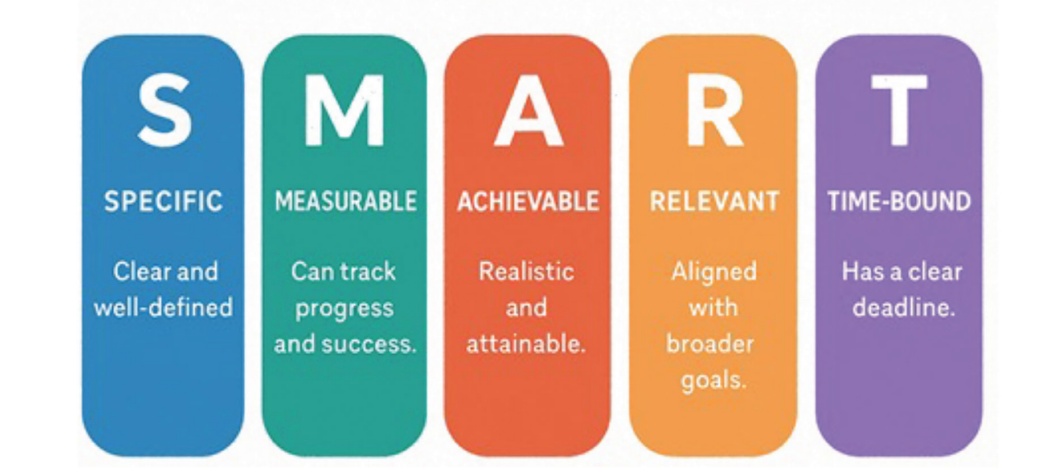
Strategic goals must be more than aspirational. They need to be specific, measurable, achievable, relevant, and time-bound (SMART) to drive meaningful progress and accountability (Figure 3). SMART goals provide a structured framework that helps hospital leaders and cardiovascular teams stay focused, track performance, and make informed adjustments along the way.
Some examples of SMART goals in cardiovascular program development include:
• Reducing 30-day readmission rates for heart failure by 15% within 12 months
This goal targets a key quality metric that impacts both patient outcomes and reimbursement. It’s specific, measurable, and tied to a defined timeline, making it actionable and trackable.
• Increasing cath lab utilization by 20% through improved scheduling and throughput
This operational goal addresses resource efficiency and capacity management. It encourages process improvement and supports financial sustainability.
• Launching a structural heart program with defined volume and revenue targets
This growth-oriented goal supports service line expansion and market differentiation. By setting volume and financial benchmarks, administrators can evaluate success and adjust strategy as needed.
• Achieving accreditation within 18 months to validate quality and differentiate the program
This goal aligns with both clinical excellence and strategic positioning. Corazon believes that accreditation serves as a milestone that reflects commitment to best practices and enhances the program’s reputation.
These objectives provide clarity and accountability across departments. When goals are SMART, teams can monitor progress using key performance indicators, identify barriers early, and recalibrate strategies to stay on course. If necessary, third-party consultants can work closely with hospital leaders to define and refine SMART goals that align with institutional priorities and position CV programs for long-term success.
Engaging Stakeholders in the Planning Process
Strategic goal setting is most effective when it reflects the perspectives and priorities of those who are directly involved in delivering CV care. Engaging a diverse group of stakeholders ensures that goals are not only clinically relevant and operationally feasible but also supported across the organization. This collaborative approach fosters ownership, alignment, and momentum.
Key stakeholders in clinical and operational initiatives encompass a diverse group whose engagement is critical to success. This includes:
• Physicians, both employed and those aligned through community partnerships, who bring clinical expertise and frontline insights. Their involvement ensures that proposed changes align with patient care standards and evidence-based best practices.
• Clinical staff, such as nurses, technologists, and other allied health professionals, who are instrumental in executing care delivery. Their feedback helps shape workflows that are both efficient and patient-centered.
• Administrative leaders, including executives and department leaders, who provide strategic direction, allocate resources, and champion organizational priorities. Their support is essential for sustaining long-term improvements and aligning initiatives with broader institutional goals.
By actively involving these stakeholders from the outset, organizations can foster collaboration, enhance buy-in, and drive meaningful, sustainable change across the continuum of care.
Step 3: Building Infrastructure for Growth
Strategic goals are only as effective as the infrastructure that supports them. For cardiovascular programs to thrive, administrators must ensure that the physical, technological, and operational foundations are not just present but fully optimized to sustain growth and deliver high-quality care. This goes beyond capital investment; it demands a deliberate, forward-thinking approach to resource planning, facility design, and system integration.
Infrastructure is the backbone of a successful CV program. Without the right tools, space, and systems, even the most ambitious goals can falter. Hospitals must assess how their current assets align with projected service line expansion, anticipated patient volume, and evolving clinical demands. This includes evaluating whether cath labs can accommodate increased procedural loads, whether imaging capabilities meet diagnostic requirements, and whether data systems enable real-time performance tracking.
Effective infrastructure planning must also respond to market dynamics and patient expectations. As cardiovascular care becomes increasingly specialized and competitive, hospitals must position themselves as leaders in access, innovation, and efficiency. This means creating environments that foster multidisciplinary collaboration, integrating technologies that enhance care delivery, and designing pathways that make it easier for patients to engage with services. Corazon believes that whether you are launching a new service line or optimizing existing operations, infrastructure development is a critical step in the journey toward CV excellence.
Modern cardiovascular care demands investing in technology, advanced facilities, and equipment. These investments should be driven by projected patient volumes, service line growth plans, and a thorough return-on-investment (ROI) analysis. To guide decision-making, administrators should evaluate:
• Capacity and Efficiency for Procedural Growth – Can current facilities not only handle increased procedural volume but do so efficiently? This includes evaluating whether workflows are optimized to minimize patient wait times, reduce turnover between procedures, and support high-throughput environments without compromising quality. Administrators should assess whether physical space, staffing models, and equipment utilization are aligned to support both growth and operational excellence. Efficient use of resources, such as streamlined scheduling, integrated systems, and flexible room configurations, can significantly enhance throughput and patient experience while controlling costs.
• Imaging capabilities – Are tools like cardiac MRI, CT (including FFR-CT), and echocardiography sufficient to meet diagnostic needs?
• Monitoring and diagnostic systems – Do existing technologies support early detection and effective management of chronic cardiovascular conditions?
Enhancing Data and Analytics Infrastructure
Robust data systems are essential for tracking performance, identifying trends, and supporting clinical decision-making. Key priorities include implementing dashboards for real-time monitoring of key performance indicators.
• Integrating EHR Systems for Seamless Documentation and Care Coordination – A well-integrated EHR system is essential for streamlining documentation, enhancing communication across care teams, and improving overall efficiency. Integration should enable real-time access to patient data, reduce duplication of effort, and support clinical decision-making through embedded protocols and alerts. It also facilitates smoother transitions of care, allowing providers to track patient progress across settings and specialties. For cardiovascular programs, this means ensuring that diagnostic results, procedural notes, medication histories, and follow-up plans are easily accessible and consistently updated, ultimately improving care coordination, reducing errors, and enhancing patient outcomes.
• Leveraging Predictive Analytics to Anticipate Patient Needs and Optimize Resource Allocation – Predictive analytics uses historical and real-time data to forecast patient trends, clinical risks, and operational demands. For CV programs, this means anticipating fluctuations in patient volume, identifying individuals at risk for acute events, and proactively managing chronic conditions. By analyzing patterns in admissions, diagnostics, and treatment outcomes, hospitals can better allocate staff, schedule procedures, and manage inventory. This not only improves clinical outcomes but also enhances efficiency, reducing bottlenecks, minimizing waste, and ensuring that resources are deployed where they are needed most. Ultimately, predictive analytics supports smarter decision-making and a more agile, patient-centered care model.
Strengthening Referral Networks and Access Pathways
Sustainable growth in CV programs depends on maintaining a steady and diverse patient pipeline. To achieve this, hospitals must take a proactive approach to building and optimizing referral relationships and access channels. Key strategies include:
• Building Strong Relationships With Referring Providers – Establishing trust and consistent communication with primary care physicians, specialists, and regional partners is essential. Hospitals should offer clear referral protocols, timely feedback on patient outcomes, and collaborative opportunities that reinforce shared goals in patient care.
• Streamlining Intake and Scheduling Processes – Reducing administrative barriers and delays in scheduling can significantly improve patient access and satisfaction. This includes ensuring timely follow-up to prevent leakage and improve conversion rates.
• Expanding Telehealth and Outreach Programs – Leveraging virtual care platforms and community outreach initiatives helps extend services to underserved and remote populations. These programs not only improve access but also strengthen the hospital’s presence in key markets and support continuity of care.
Network development strategies that enhance access, improve patient experience, and increase market share are essential. By aligning referral pathways with strategic growth objectives, hospitals can position their CV programs for long-term success.
Step 4: Elevating Clinical Quality
At the heart of any successful cardiovascular program is a steadfast commitment to clinical excellence. Elevating quality is not a one-time initiative but a continuous, organization-wide effort that demands disciplined execution, transparent data practices, and a culture of accountability. This commitment must be embedded in every aspect of care delivery, from bedside protocols to leadership strategy.
In today’s healthcare environment, where clinical outcomes are increasingly tied to reimbursement, public reporting, and competitive positioning, quality is both a strategic imperative and a moral obligation. Hospitals must prioritize evidence-based practices, invest in ongoing staff education, and implement robust performance monitoring systems. Real-time data should inform decision-making, highlight areas for improvement, and celebrate successes.
Moreover, fostering a culture of accountability means empowering teams to take ownership of outcomes, encouraging interdisciplinary collaboration, and ensuring that quality metrics are not just tracked but acted upon. When clinical excellence becomes a shared value across the organization, it drives better patient outcomes, enhances reputation, and supports long-term program growth.
Standardizing care through evidence-based guidelines reduces variability, improves outcomes, and supports accreditation efforts. Hospitals should:
• Adopt national protocols for acute coronary syndrome, heart failure, and arrhythmia management.
• Embed clinical decision support tools within the EHR to guide treatment decisions.
• Conduct regular reviews of protocol adherence and update practices based on emerging research.
Measuring and Monitoring Performance
Robust performance measurement is essential for identifying gaps and driving improvement. Key metrics include:
• Door-to-balloon time for ST-elevation myocardial infarction (STEMI) patients.
• 30-day readmission rates for heart failure and post-procedure patients.
• Mortality and complication rates for surgical and interventional procedures.
Third-party consultants can help organizations build dashboards and reporting systems that provide real-time visibility into clinical performance and support data-driven decision-making.
Fostering a Culture of Continuous Improvement
Quality improvement is most effective when it is embedded into the culture of the organization. Leaders should empower clinical teams to lead quality initiatives and participate in peer review, celebrate successes and share lessons learned across departments, and engage in national registries and quality collaboratives to benchmark performance and adopt best practices. Corazon believes that a culture of quality is developed through leadership coaching, performance audits, and strategic planning.
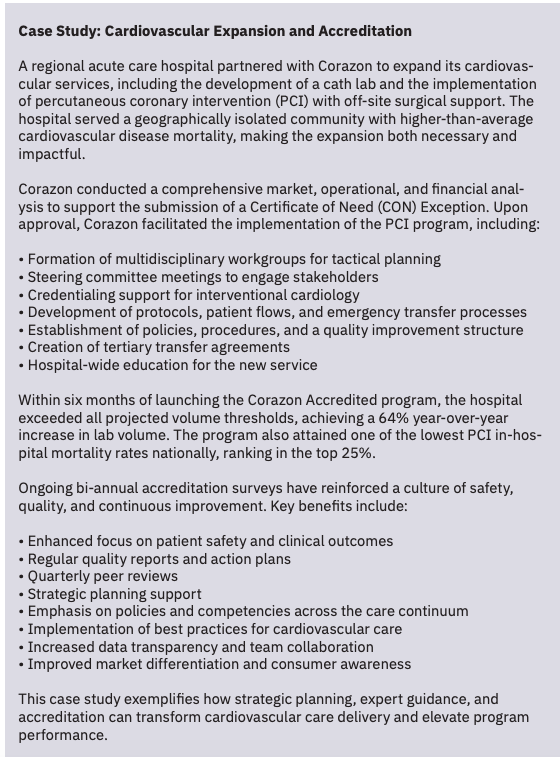
Step 5: Achieving Accreditation
Accreditation is a powerful milestone on the journey to cardiovascular excellence and signals a program’s commitment to delivering safe, evidence-based, high-quality care. It is a strategic asset that validates clinical rigor, operational discipline, and a culture of continuous improvement. For hospital administrators, pursuing accreditation is not simply about meeting external standards, it is about elevating the program’s reputation, enhancing performance, and unlocking new opportunities for growth and sustainability.
In today’s competitive healthcare environment, accreditation serves as a clear differentiator. It communicates to patients, payers, and referring providers that your cardiovascular program adheres to nationally recognized best practices and is held accountable to measurable outcomes. This distinction can influence referral patterns, strengthen market positioning, and support strategic partnerships.
Moreover, the process of achieving accreditation often drives internal transformation. It prompts a deep review of protocols, workflows, documentation, and performance metrics, which leads to operational efficiencies and improved clinical outcomes. The return on investment is tangible: accredited programs frequently experience better reimbursement rates, improved outcomes, reduced risk exposure, and stronger alignment with value-based care models. By investing in accreditation, hospital leaders elevate the quality of care and strengthen the foundation for long-term growth, sustainability, and competitive advantage. With guidance from experienced partners like Corazon, hospitals can navigate the accreditation journey with confidence, ensuring that the process not only results in accreditation but also delivers lasting value across the organization.
Step 6: Measuring Success and Sustaining Excellence
Achieving excellence is not a one-time accomplishment but an ongoing commitment to performance, innovation, and accountability. Once strategic goals are in motion and accreditation is achieved, there must be methods established to measure progress, evaluate impact, and ensure long-term sustainability. This final step in the roadmap ensures that the program remains agile, responsive, and aligned with evolving standards and patient needs.
Defining and tracking key performance indicators is essential for monitoring success across clinical, operational, and financial domains. Common CV-focused key performance indicators include:
• Procedure volumes and growth trends.
• Door-to-balloon time and other time-sensitive metrics.
• Readmission and complication rates.
• Patient satisfaction and engagement scores.
• Contribution margin by service line.
Corazon believes that customized dashboards and reporting tools provide real-time visibility and support data-driven decision-making.
Ongoing program reviews and evaluation is critical to maintaining momentum and identifying areas for recalibration. Leaders should regularly schedule quarterly or biannual reviews of performance data, revisit strategic goals, and adjust timelines or tactics as needed, and engage stakeholders in reviewing outcomes and identifying new opportunities. Reviews foster transparency, accountability, and continuous improvement.
Recognizing achievements, whether it is meeting a quality benchmark, launching a new service, or earning accreditation, reinforces a culture of excellence. Sustaining excellence requires more than metrics. It requires a shared commitment to delivering the highest standard of cardiovascular care, every day.
Conclusion
Cardiovascular excellence is not achieved through isolated efforts; it is the result of a strategic, coordinated journey that touches every aspect of program development, from clinical quality and operational efficiency to infrastructure, workforce, and accreditation. For hospital administrators, this roadmap provides a clear and actionable framework to enhance CV services in a manner that aligns with institutional goals, meets patient needs, and positions the organization for long-term success.
Now is the time to take the next step. Whether your program is preparing for expansion, seeking accreditation, or simply aiming to improve outcomes, a well-defined roadmap can transform vision into reality, and set your CV program apart in a competitive healthcare landscape. Expert guidance from partners like Corazon can help hospitals can navigate this journey with confidence. Regardless of your path forward, leaders must ensure that every initiative is grounded in data, driven by strategy, and supported by a culture of excellence.
References
-
National Center for Health Statistics. Multiple Cause of Death 2018–2023 on CDC WONDER Database. Accessed February 1, 2025. https://wonder.cdc.gov/mcd.html
-
Bhatt AB, Biesbrock GK, Biga C. Best practices for transforming cardiovascular care delivery and implementation: a modern framework. J Am Coll Cardiol. 2025 Apr 22; 85(15): 1580-1582. doi:10.1016/j.jacc.2025.02.020
-
olu-Akinnawo O, Ezekwueme F, Awoyemi T. Telemedicine in cardiology: enhancing access to care and improving patient outcomes. Cureus. 2024 Jun 21; 16(6): e62852. doi:10.7759/cureus.62852
-
O’Donnell B, Gupta V. Continuous Quality Improvement. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559239/
-
Corazon. Elevating Program Quality and Cardiovascular Patient Care. (2023, May 19). Accessed January 9, 2025. https://corazoninc.com/why-accreditation-matters-for-elevating-cardiovascular-care/#:~:text=Accreditation%20is%20a%20seal%20of,in%20the%20U.S.%20to%20date
Find More:
Renal Denervation Topic Center
Cardiovascular Ambulatory Surgery Centers (ASCs) Topic Center
Grand Rounds With Morton Kern, MD
Peripheral Artery Disease Topic Center










